
Journal of Perioperative Medicine
Open Access
ISSN: 2684-1290

ISSN: 2684-1290
Research Article - (2019) Volume 2, Issue 1
Background: The use of Ultra-fast-track (UFT) management in cardiac surgery may shorten hospital length of stay (Hosp-LOS) when is part of a protocol of enhance recovery after surgery (ERAS).
Methods: We retrospectively analyzed the data of the patients undergoing elective off-pump coronary artery bypass grafting (OPCAB) using UFT under a pilot program of ERAS at a Venezuelan nonprofit cardiac center from 2010 to 2014. The primary goal was to describe the short-term outcome of a consecutive case-series managed with desfluraneremifentanil- intercostals nerve block for OPCAB by Left-Anterolateral Thoracotomy and followed up by multidisciplinary enhance recovery pathway. The secondary goals were to identify perioperative predictors for UTF-failure and Hosp-LOS >4 days and try to propose a predictive risk model from the variables involved.
Results: 1,943 bypasses were performed on 673 patients. 61.5 ± 9.5 years old, EuroSCORE was 5.2 ± 4.1. 97.8% was extubated in Operating Room (UFT-success) and 2.2% extubated in the intensive care unit (UFT-failure). The reintubation rate was 0.5%. Patients had an Intensive Care Unit length of stay (ICU-LOS) of 29 ± 4.2 hours; 636 patients (94.5%) had ICU-LOS ≤ 24 h, 2.1% readmitted to ICU. The Hosp-LOS after discharge from ICU was 50.5 ± 9.9 hours, 633 (94.1%) had Hosp-LOS ≤ 4 days. Univariate analysis revealed as independent risk factors for UFT-failure: age, female sex, EuroSCORE, Severity of Angina Pectoris, EF <30%, Redo, COPD, PRBC transfusion, use of elective IABP and duration of surgery(t-Qx). However, multivariate logistic regression analysis and backward elimination method found as strong risk factors for UFT-failure: transfusion of ≥ 2 PRCB Adjusted Odds Ratio (AOR=6.02) (95%CI) (p<0.05), t-Qx 3-4 hrs, (AOR=77.3)(95%CI) (p <0.001) and t-Qx > 4 hrs, (AOR=157.5) (95%CI) (p <0.001). Univariate analysis revealed as independent risk factors for Hosp-LOS >4 days : Age>80 y-old, female sex, NYHA>III, EuroSCORE, severity of Angina pectoris , EF <30%, Redo, renal failure, IABP, PRCB transfusion, UFT-failure, t-Qx and ICU-LOS (p<0.001). Multivariate logistic regression analysis and backward elimination method found as strong risk factors for Prolonged Hosp-LOS ( >4 days) : Redo (AOR=7.68) (95%CI), t-Qx>3 hrs (AOR>74) (95%CI) (p<0.001) and ICU-LOS >24 hrs (AOR=29.3) (95%CI) (p<0.001).
Conclusions: As most patients were extubated in the Op.Room, had short ICU-LOS (<24 h) and short Hospital- LOS (≤ 4 days). UTF appears to have clinical benefits in this setting. In general, age>80 y.o , female sex, severity of EuroSCORE and ≥ 2 PRBCs transfusion were risk factor for UTF-failure and prolonged Hosp-LOS. However, the stronger predictive factors for UTF-failure and Hosp-LOS>4 days were transfusion of ≥ 2 PRCB, Redo, duration of surgery >3 h and ICU-LOS >24 h. Prospective studies would better elucidate the risk factors for longer Hospital-LOS and attendant morbidities.
Keywords: Ultra-fast track; Off-pump coronary artery bypass graft; Left anterolateral thoracotomy; Beating heart; Early extubation; Enhanced recovery after surgery (ERAS)
OCAPB: Off-pump Coronary Artery Bypass; LAT: Left Anterolateral Thoracotomy; CABG: On-pump Coronary Artery Bypass Graft; UFT: Ultra-Fast-Track; UTF-success: Extubation in Operative Room; UFT-failure: Extubation in Intensive Critical Unit; NYHA: New York heart association; ASA: American Society of Anaesthesiologist; Op.Room: Operatory Room; ICU: Intensive Critical Unit; ICU-LOS: Intensive Critical Unit Length of Stay; Hosp-LOS: Hospitalization Length of Stay; ERAS: Enhance Recovery After Surgery; PRCB: Packet of Red Cell Blood; EF: Ejection Fraction; OR: Odds Ratio; AOR: Adjusted Odds Ratio; CI: Confidence Interval; AUC: Area Under Curve; t-Qx: Duration of Surgery; IBP: Invasive Blood Pressure; PR: Pulse Rate; RR: Respiratory Rate; TOF: Tren Of Four; NSAIDS: Non Steroidal Anti-Inflammatory Drugs; CPB: Cardiopulmonary Bypass; IABP: Intra-Aortic Ballom Pump; Redo: Previous CABG;
ARDS: Respiratory Distress Syndrome; COPD: Chronic Obstructive Pulmonary Disease; BMI: Body Mass Index; DM: Diabetes Mellitus; HTA: Arterial Hypertension; PAD: Peripheral Artery Disease; TEE: Trans-Esophageal Echocardiography; VAS: Visual Analogue Scale; MI: Myocardial Infarct; RWMA: Regional Wall Motion Abnormality; A.P(CCS): Angina Pectoris Canadian Cardiovascular Society grades; LV: Left Ventricular; CAD: Coronary Arterial Disease; AF: Atrial Fibrillation; PCI: Percutaneus Coronay Inteventional Procedure; LIMA: Left Internal Mammary Artery; RIMA: Right Internal Mammary Artery.
Fast track anesthesia in cardiac surgery, which enables extubation within 0-6 hours of the end of surgery, gained acceptance after the 1990’s when it was proven to reduce intensive care unit length of stay (ICU-LOS), use of resources, and cost [1]. The same could be said for ultra-fast track (UFT) anesthesia with the use off-pump coronary artery bypass grafting (OPCAB) which enables extubation in the operating room (Op.Room), immediately after the surgery is completed, with relatively few major complications [2-5]. A direct relationship has been suggested between UFT extubation and reductions in the use of sedatives, analgesics, intravenous fluids, inotropic agents, vasopressors, and anti-arrhythmics in the ICU [6,7]. Originally designed for lowrisk patients, immediate extubation after OPCAB is becoming more common for high-risk cardiac surgery patients [8]. OPCAB procedures managed with fast-track protocols have been carried out by median sternotomy, [9] by left anterolateral thoracotomy (LAT), [10] and with minimally invasive direct coronary artery bypass (MIDCAB), with or without staged hybrid revascularization [11,12].
Enhanced recovery pathways are multimodal, evidence-based protocols including step-by-step management plans throughout the perioperative period. The benefits of UFT anesthetic management after OPCAB should be supported by structured protocols of enhance recovery after surgery (ERAS) properly adapted to this type of surgery and also to each hospital. Evidences suggest that enhanced recovery pathways improve postoperative recovery, reduce morbidity and hospital length of stay (Hosp-LOS), and cost of care for variety of surgical procedures by mean of attenuating perioperative physiologic stress (eg. psychological support, preoperative oral carbohydrate, respiratory exercise training, and afferent neural blockade) and decreasing the use of interventions that slow down recovery progress without improving outcomes (eg. prolonged preoperative fasting, prolonged urinary drains, delayed postoperative feeding ) [13]. Majority of ERAS evidence come from abdominal surgery [14], and some reports describe the impact of UFT plus ERAS on outcomes of OPCAB and thoracic surgery [15].
The aims of this descriptive and retrospective study were: 1) to show the short- term outcome ( ≤ 30 days) of a consecutive case series of 673 patients managed by UFT anesthetic technique utilizing a combination of desflurane, remifentanil, and intercostals nerve block in OPCAB by the LAT approach and supported by multidisciplinary enhance recovery pathway; 2) to identify perioperative predictors for UTF-failure and Hosp-LOS>4 days; 3) Try to propose a predictive risk model from the variables involved .
With institutional review board approval, we collected retrospective data of consecutive patients who had undergone OPCAB between June 2010 and December 2014 and met the criteria for extubation-in-Op. Room and followed up by an adapted ERAS protocol at a nonprofit cardiovascular surgery center (FundaCardio Foundation, Valencia, Venezuela), emergencies, and pediatric procedures were excluded. The ethics committee of the hospital provided us with a coded database for the retrospective review following strict compliance with the regulations of personal data protection.
Data collected included patient demographics and co-morbidities, European System for Cardiac Operative Risk Evaluation (EuroSCORE) and New York Heart Association (NYHA) functional class, whether patients were extubated in the Op.Room (UFT-success) or ICU (UFTfailure), intraoperative and postoperative complications, ICU-LOS, Hosp-LOS, and mortality at 30 days.
Enhanced recovery after surgery (ERAS)
Since the end of 2009 year, our team began to implement and testing a preliminary multidisciplinary program of structured perioperative support to provide early recovery after OPCAB in elective patients as complement of UTF protocol. The objective of the early recovery pathway was to introduce a standard multimodal approach, including preoperative patient and family education, psychological and nutrition support, opiod-sparing pain management, early and conducted mobilization, early feeding as possible and standardized drains management. Elements of the early recovery pathway used a specific physician and surgeon orders, patients-adapted cardiologic orders, daily nursing records and patient education booklet. The team was led by a surgeon (full-time coordinator) and an anesthesiologist, also included a cardiologist, ICU physician, expertise in nursing (inpatient and outpatient), a full-time outpatient nursing coordinator, physiotherapy, pharmacy, pain service, nutrition services. Protocol is summarize in Supplementary 1.
Anesthesia protocol
The preanesthetic evaluation was scheduled after two previous ERAS-training interviews, as minimum. During the pre-anesthetic interview, we reviewed the patient’s medical records, identify comorbidities and chronic medications, evaluate anesthetic risk, and stratify by EuroSCORE and NYHA functional class, and perform a physical exam. If it necessary, call internist, cardiologist or pulmonologist to optimized any pre-existing co-morbidity. Ask if the patients and family were properly informed and trained by ERAS team and check any doubt about perioperative information booklet. Then, we ask for the informed consent.
Prior to the surgery, routine medications are suspended as follows: Clopidogrel, prasugrel, or ticagrelor are suspended 7 days before surgery; dabigatran ,rivaroxaban or apixaban, 5 days before surgery; aspirin, the day before surgery; and eptifibatide or tirofiban, 12 hours before surgery. Warfarin is suspended 5 days before surgery and the international normalized ratio is monitored until the target of ≤ 1.5 is reached. Enoxiparine or another low molecular weight heparin is used when an anti- aggregant, anti-platelet, or anticoagulant is suspended; the last heparin dose is administered 24 hours before surgery. Premedication consists of oral benzodiazepine, midazolam 7.5 mg the night before surgery with 100-150 ml of Ensure Clear® (Abbott Nutrition Products) a fat-free flavored nutrition clear liquid after dinner (regular diet until 9 pm for the morning schedule patients, and 6 am for afternoon schedule patients) and gabapentin 600 mg two hours before surgery with 100 ml of G2 Gatorade® (PepsiCo) or Powerade® (Coca- ColaCo.).
The goal of the anesthetic plan was immediate extubation in the Op.Room. On arriving in the Op.Room, a peripheral intravenous (IV) line is catheterized in the right upper limb, standard ASA monitoring is started, and an arterial line is catheterized into the right radial artery for invasive blood pressure (IBP) monitoring. After facemask oxygenation with a FIO2 of 100% for 5 minutes, induction of anesthesia is initiated with remifentanil at 0.15-0.2 μg/kg/min IV infused by a volumetric pump and titration of propofol at 1-1.5 mg/kg IV. When eyelash loss reflex is achieved and bispectral index is about 50-55, rocuronium bromide doses are administered at 0.6 mg/kg IV, and the patient is intubated when one response or less to train of four (TOF) is achieved. Trans-esophageal echocardiography (TEE) is then used to assess standard ASA views and identify any new feature or cardiac issue. The left subclavian vein is catheterized and central venous pressure is checked. The procedure then moves to the left pulmonary exclusion with a bronchial blocker guided by a flexible fiberoptic under 90% oxygen to manage the patient with right-sided one lung ventilation (OLV) to facilitate the surgical approach. Ventilation monitoring includes basic parameters of mechanical ventilation and pressure-volume and flowvolume loops. If selective ventilation cannot be established or the patient cannot tolerate OLV, the left lung is gently compressed with a laparotomy sponge. Maintenance of anesthesia is accomplished with desflurane 0.5-0.8 MAC (ET.vol%) to maintain the bispectral index between 40 and 60, a variable dose of remifentanil infusion to maintain hemodynamic stability (IBP and PR ± 10%-15% of pre-anesthesia induction value), and ketamine 0.15 mg/kg/h IV. Muscle relaxation (by monitoring post-tetanic count stimulation) is maintained at a profound to intense level with additional rocuronium doses at 0.3 mg/kg IV. For adequate control of body temperature, we use an underbody thermal blanket, administer normothermic endovenous fluids using a fluid warmer, and turn off air-conditioning in the surgical room. Corporal temperature is measured by a continuous nasopharyngeal, bladder, and rectal thermometer.
Other protocols
The blood transfusion trigger is hemoglobin (Hb) ≤ 8/dL. Transfusion management is determined by hematocrit (Hct), ventricular function, oxygen saturation of central vein blood (ScvO2), serum lactate, and co-morbidities, and the goal is to keep a Hct above 20%-25% in patients with normal hemodynamic parameters (ScvO2>70 mmHg, and serum lactate23 mEq/Lt. Hourly urine output is registered through a Foley catheter. Anticoagulation therapy is performed at a heparin dose of 1.2 mg/kg IV to achieve an activated clotting time target of 300 ± 20 seconds. A tranexamic acid bolus 10 mg/kg IV is followed by 1 mg/kg/h IV, and finally, heparin is reversed with protamine sulfate IV, which is calculated at a dose of 1 mg per every 100 units of heparin.
Surgical technique
The myocardial revascularization is performed on the beating heart by the LAT using a tissue stabilization system (Figure 1). The patient is positioned with the left side elevated at approximately 45°, rotated decubitus toward the right with the help of a rolled towel. External pads for emergency defibrillation are placed on the right supero-anterior and left infero-posterior sides of the chest wall, and the incision is carried out on the fourth or fifth left intercostal space. The left internal mammary artery (LIMA) is harvested under direct visualization in a skeletonized fashion using a Finochietto retractor. If needed, the right internal mammary artery (RIMA) is harvested after the pericardial fat and thymus are carefully removed. When required, proximal graft anastomoses are performed using a side-bite partial clamp in the conventional fashion. The distal anastomoses are made on the beating heart using a pressure stabilizer and intracoronary shunt whenever possible. For the grafting of the circumflex and right coronary territory, the heart is lifted out of the pericardium using an apical suction device [10]. Maintaining myocardial perfusion during the anastomosis is crucial since ventricular tachycardia or hemodynamic instability caused by myocardial ischemia could lead to an emergency conversion to sternotomy [8-12,16]. Before leaving the Op.Room, fentanyl 0.5-1.0 μg/kg is administered if necessary.
Criteria for extubation in the Op.Room
Five respiratory criteria must be met no longer than 40 minutes for a patient to be eligible for extubation in the Op.Room:
Respiratory criteria: 1. SpO2 >92% or PaO2 >60 mmHg; 2. Spontaneous RR>8 bpm; 3. ETCO22
Muscle relaxation status: TOF>0.9. (spontaneously, or sugammadex 2 mg/kg)
Neurologically intact (follows verbal commands, intact cough/gag reflex),
Acid-base status (pH >7.35), normal electrolytes.
Hemodynamic status (IBP and PR ± 15-20% of baseline, nonthreatening arrhythmias, without evident bleeding (0.5 ml/Kg/h. Use of inotrope/vasopressor therapy is not an absolute contraindication. However, extubation is avoided if the vasoactive-inotropic score (VIS) is ≥ 10.16
Normothermia (body temperature 36°C-37°C) is maintained during the entire surgical procedure.
Pain management (visual analog scale ≤ 4/10): Intercostals nerve block performed by surgeon with 20 mL bupivacaine 0.5% and 4 mg of dexametasone at the level of the surgical approach, one level above and below the intercostal space used for the surgery. A multi-perforated epidural catheter through the incision and positioned in the involved intercostal space to administer a programmed continuous infusion of bupivacaine 0.5% at a rate of 10 ml/h for the first 48 h. Rate its modified according a numeric pain rating scale. NSAIDS: ketoprofen 100 mg IV and paracetamol 1 gr IV are also used. Muscle relaxants are reversed with sugammadex at 2 mg/kg IV. Desflurane and a remifentanil infusion are discontinued, and the patient is ventilated with 100% oxygen. Before extubation, the patient is then transported to the ICU in a 35° sitting position, with a 50% O2 face mask.
Postoperative care
The patient is delivered to the ICU conscious, capable of responding to simple orders, and possibly with mild pain (VAS <4/10). For rescue pain relief, morphine is administered by patient-controlled analgesia consisting of a 1 mg bolus of morphine with a 15-minute lockout and maximal dose of 3 mg/h. All infusions are checked. If the vital parameters are acceptable, cardiovascular drugs are gradually reduced. If the left lung is well re-expanded and tubes have stopped draining or
Once discharged, the patient is given the telephone number of a surgical team member (surgeon coordinator) in case there are any symptoms or complications. During ERAS interview before the surgery, the patient and family would have been taught how to perform respiratory exercises and manage wounds, and the patient, encouraged to start walking as soon as possible (Supplementary 1). A team of nurses performs daily at-home wound care for a week. The patient is then followed with regular outpatient appointments with either the surgeon or cardiologist at 1, 2, 4, 6, and 8 weeks postoperatively.
Statistical analysis
Analyses were performed using SPSS version 16.0 for Windows (SPSS,Chicago,IL,USA). Descriptive statistic: Demographic and clinical variables were described by means, standard deviations, median, mode, ranges (min-max) for continuous variables, and absolute and relative frequency (%) for categorical variables. Many of the variables were presented as dichothomous. Age was redefined as a dichotomous variable using the cut-off of 80 years, to calculate odds ratios for age.
Inferential statistic: to look for predictors (risk factors) for UTFfailure and prolonged Hosp-LOS: 1st Step) Estimation of Crude (no adjusted) Odds Ratio (OR) with 95% confidential interval (CI). Univariate logistic regression analysis was used to evaluate association between each independent variable with extubation outcome (UFTfailure) and prolonged Hosp-LOS, defined as >4 days. 2nd Step) Estimation of Adjusted OR (AOR): Multivariate binary logistic regression model was used including all significant variables (p st step. 3rd Step) Backward elimination method is to identify the independent variables with enough explanatory ability. (4th Step) ROC curve analysis, calculation of AUC (95% CI with initial cut-off point of p=0.5) and criterion for selection of the optimum cut-off points by Youden’s index to illustrate the diagnostic ability of decision making rule of both predictive models, for UFT failure and Hosp-LOS >4 days.
The alpha level was set at p <0.05(5%) and power at 80%.
A total of 673 consecutive patients who were 518 male (77%), 155 female (23%) and a mean age of 61.5 ± 9.5 years old (y.o), median 61 y.o (range, 36-90 years) were included in the study. All had undergone OPCAB by the same surgical, anesthetic, and critical care team. The mean EuroSCORE was 5.2 ± 4.1 (range, 0-17). The NYHA functional classification was Class I, 72 patients (10.7%); Class II, 385 (57.2%); Class III, 150 (22.3%) and Class IV, 66 (9.8%). The mean ejection fraction (EF) was 47 ± 10 %, 335 patients (49.8%) of patients had EF >50% and 41 patients (6.1%) had EF <30%. Coronary artery disease affected three vessels in 580 patients (86.2%); within this group, 57 (8.4%) required four or more grafts. A majority (546, 81.1%) were diagnosed with hypertension and 412 (61.2%) were taking two or more antihypertensive medications. A total of 456 (67.7%) had hyperlpidemia and close to half (41%) had diabetes mellitus type 2.None patient had DM tipo I. 168 patients had obesity with BMI 30-37 Kg/mt2 , the majority were Class I(BMI 30-34 Kg/mt2) following the World Health Organization classification. There were 215 (31.9%) with chronic obstructive pulmonary disease. Twice as many (446, 66.3%) smoked 10 or more cigarettes per day. Nearly half had experienced a previous myocardial infarction (Table 1).
| Total N (%) / mean ± sd | |
|---|---|
| Patients | 673 (100) |
| AGE (y.o) | 61.5 ± 9.5 |
| Age Group | |
| <=80 y | 641 (95.2) |
| >80 y | 32 (4.8) |
| Gender | |
| Male | 518 (77) |
| Female | 155 (23) |
| Smoker | |
| No | 227 (33.7) |
| Yes | 446 (66.3) |
| NYHA | |
| Class I | 72 (10.7) |
| Class II | 385 (52.7) |
| Class III | 150 (22.3) |
| Class IV | 66 (9.8) |
| CAD | |
| 1 vessel | 40 (5.9) |
| 2 vessels | 53 (7.9) |
| 3 vessels | 580 (86.2) |
| Left Main Stem | |
| No | 547 (81.3) |
| Yes | 126 (18.7) |
| A. P(CCS) | |
| Grade III | 355 (52.7) |
| Grade IV-A | 144 (21.4) |
| Grade IV-B | 127 (18.9) |
| Grade IV-C | 47 (7.0) |
| HTA | |
| No | 127 (18.9) |
| Yes | 546 (81.1) |
| LV Function (EF) | 47.3 ± 10.2 |
| Group LV (EF) | |
| >50% | 335 (49.8) |
| 30%-50% | 297 (44.1) |
| <30% | 41 (6.1) |
| Mycocardial Infraction | |
| No | 342 (50.8) |
| Yes | 331 (49.2) |
| PCI | 148 (21.9%) |
| Pre-Stroke | |
| No | 617 (91.7) |
| Yes | 56 (8.3) |
| REDO | |
| No | 617 (91.7) |
| Yes | 56 (8.3) |
| PAD | |
| No | 448 (66.6) |
| Yes | 225 (33.4) |
| DM II | |
| No | 397 (59.0) |
| Yes | 276 (41.0) |
| Hyperlipidema | |
| No | 217 (32.2) |
| Yes | 456 (67.8) |
| Obesity (BMI>30 WHO) | |
| No | 217 (32.2) |
| Yes | 456 (67.8) |
| Renal F (Creatinine>2.0 mg/dl) | |
| No | 568 (94.4) |
| Yes | 105 (15.6) |
| COPD (GOLD) | |
| No | 458 (68.1) |
| (FEV1/FVC<70%,FEV1≥80%) 1 | 128 (19.0) |
| (FEV1/FVC<70%, FEV1 50%-80%) 2 | 87 (12.9) |
| PRBC | |
| 0 | 561 (83.4) |
| 1 | 74 (11.0) |
| >=2 | 38 (5.6) |
| IABP | |
| No | 607 (90.2) |
| Yes | 66 (9.8) |
| Euroscore | 5.2 ± 4.1 |
| Risk Euroscore | |
| Low | 374 (55.6) |
| Medium | 239 (35.5) |
| Severe | 60 (8.9) |
| t- QX | |
| <=3 h | 615 (91.4) |
| 3-4 h | 48 (7.1) |
| >4 h | 10 (1.5) |
| Extubation | |
| UFT-success | 658 (97.8) |
| UFT-failure | 15 (2.2) |
| ICU-LOS | |
| <=24 h | 636 (94.5) |
| 24-72 h | 17 (2.5) |
| >72 h | 20 (3.0) |
| HOSP-LOS | |
| <=4 d | 633 (94.1) |
| >4 d | 40 (5.9) |
| Qx-Approach | |
| ALT | 653 (97%) |
| PLT | 20 (3%) |
| Coronary Vessel Targets | |
| Left anterior descending | 648 (96%) |
| Obtuse marginal | 465 (69%) |
| Diagonal branches of LCA | 386 (57%) |
| Posterior descending | 281 (42%) |
| Circumflex | 68 (10%) |
| Right coronary | 60 (9%) |
| Left main stem | 35 (5%) |
| Grafts | |
| Saphenous vein | 1123 |
| LIMA | 644 |
| Radial artery | 109 |
| RIMA | 67 |
| Rescue Surgical Procedures | |
| Femoro-femoral CPB | 3 (0.4%) |
| Conversion to sternotomy | 0 |
| Complications | |
| Pulmonary infection | 18 (2.7%) |
| Arrhythmia (AF) | 16 (2.4%) |
| Reoperation for bleeding | 13 (1.9%) |
| Death | 11 (1.6%) |
| Low CO syndrome | 8 (1.2%) |
| Acute renal (non-HD) | 6 (0.9%) |
| Stroke | 6 (0.9%) |
| Myocardial infarction | 4 (0.6%) |
Table 1: Short-Time Outcome, Descriptive data, Demographic, clinical and surgical variables. N (%)/mean ± standard desviation(sd).
In all 1,943 bypasses were performed with an average of 3 ± 1 bypass grafts per patient. The approach was by LAT in 653 patients (97%) and posterolateral thoracotomy in 20 (3%). 91.4% of patient had a surgery time (t-Qx) ≤ 3 h and 58 patients (8.6%)>3 h. Sixty-six patients (9.8%) received elective intra-aortic balloon pump (IABP) because of having met two or more of following conditions: left main stem disease, unstable angina pectoris, myocardial infarction ≤ 30 days, redo, and EF ≤ 30%. No cases converted to sternotomy. Three patients required hemodynamic support by femoro-femoro cardiopulmonary bypass (CBP) although the beating heart was kept during coronary arteries bypasses placement (Table 1).
Postoperative outcomes
Nearly all patients (658, 97.8%) were extubated in the Op.Room whereas only 15 (2.2%) were extubated later in the ICU (UFT-failure), for the most part because of bleeding. Three patients (0.5%) were reintubated within the first 72 h in the ICU. The mean ICU-LOS was 29 ± 4.2 h, mode 20 h (range, 8-480 h), and nearly all patients (636, 94.5%) were in the ICU for less than 24 h. The ICU readmission rate was 2.1% (14 patients). Three patients were readmitted twice, and one patient three times; all four died. The most common reasons for ICU readmission were pneumonia (9 patients), sepsis (9), acute respiratory distress syndrome (6), and multiorgan failure syndrome (5). The mean of Hosp-LOS after discharge from the ICU was 50.5 ± 9.9 hours, mode 48 hrs (range, 22-528 hours).
633 patient had Hosp-LOS ≤ 4 days (94.1%) and 5.9% with Hosp-LOS>4 days .Overall, the more common complications were pulmonary infection (18,2.7%), arrhythmia (16,2.4%), and reoperation for bleeding (13,1.9%) (Table 1). Mean volume of blood lost was 541.5 ± 61.3 mL (range, 63-3500 mL); 112 (16.6%) patients received a mean of 1.0 ± 2.5 PRBC units (range,0-8 Units p.p); 74 patients were transfused with 1 PRBC units and 38 patients (5.6%) received ≥ 2 PRBC. Eleven patients (1.6%) died within 30 days of the procedure. Those who died were diagnosed with multiple complications, the most common of which were multiorgan failure syndrome (9),acute respiratory distress syndrome (8), pneumonia (6), and sepsis (6).
Univariate analysis revealed as independent risk factors for UFTfailure: age, female sex, EuroSCORE, Severity of Angina Pectoris (IVgrade CCS), EF<30%, Redo, COPD, PRBC transfusion, use of elective IABP and duration of surgery (t-Qx). Redo was strongly significant (OR=36.5, p<0.001) (Table 2).
| N (%)/mean ± sd | OR (95%CI) | p-value | ||
|---|---|---|---|---|
| Extubation | ||||
| UFT-success | UFT-failure | |||
| Patients | 658 (97.8) | 15 (2.2) | ||
| Age (Y) | 61.3 ± 9.4 | 73.1 ± 9.8 | 1.13 (1.07-1.19) | <0.001*** |
| Group Age | ||||
| <=80 y | 630 (98.3) | 11 (1.7) | 1 | |
| >80 y | 28 (87.5) | 4 (12.5) | 8.18 (2.45-27.3) | 0.001** |
| Gender | ||||
| Male | 515 (99.4) | 3 (0.6) | 1 | |
| Female | 143 (92.3) | 12 (7.7) | 14.4 (4.01-51.7) | <0.001*** |
| Smoker | ||||
| No | 219 (96.5) | 8 (3.5) | 1 | |
| Yes | 439 (98.4) | 7 (1.6) | 0.44 (0.16-1.22) | 0.114 |
| NYHA | ||||
| Class I | 68 (94.4) | 4 (5.6) | 1 | 0.082 |
| Class II | 381 (99.0) | 4 (1.0) | 0.18 (0.04-0.73) | 0.017* |
| Class III | 146 (97.3) | 4 (2.7) | 0.47 (0.11-1.92) | 0.29 |
| Class IV | 63 (95.5) | 3 (4.5) | 0.81 (0.17-3.76) | 0.787 |
| CAD | ||||
| 1 Vessel | 40 (100) | 0 (0) | 1 | |
| 2 Vessels | 51 (96.2) | 2 (3.8) | ||
| 3 Vessels | 567 (97.8) | 13 (2.2) | 1.04 (0.23-4.70) | 0.956 |
| Left Main Stem | ||||
| No | 536 (98.0) | 11 (2.0) | 1 | |
| Yes | 122 (96.8) | 4 (3.2) | 1.59 (0.50-5.10) | 0.429 |
| AP(CCS) | ||||
| Grade Iii | 353 (99.4) | 2 (0.6) | 1 | 0.016* |
| Grade IV-A | 140 (97.2) | 4 (2.8) | 5.04 (0.91-27.8) | 0.063 |
| Grade IV-B | 122 (96.1) | 5 (3.9) | 7.23 (1.39-37.7) | 0.019* |
| Grade IV-C | 43 (91.5) | 4 (8.5) | 16.4 (2.92-92.3) | 0.001** |
| HTA | ||||
| No | 119 (93.7) | 8 (6.3) | 1 | |
| Yes | 539 (98.7) | 7 (1.3) | 0.19 (0.07-0.54) | 0.002** |
| Lv Function (Ef) | 47.4 ± 10.2 | 41.9 ± 12.1 | 0.95 (0.91-0.99) | 0.046* |
| Group Lv Function (Ef) | ||||
| >50% | 331 (98.8) | 4 (1.2) | 1 | 0.009** |
| 30%-50% | 290 (97.6) | 7 (2.4) | 1.99 (0.58-6.89) | 0.274 |
| <30% | 37 (90.2) | 4 (9.8) | 8.94 (2.14-37.2) | 0.003** |
| Myocardial Infarction | ||||
| No | 336 (98.2) | 6 (1.8) | 1 | |
| Yes | 322 (97.3) | 9 (2.7) | 1.56 (0.55-4.45) | 0.4 |
| Pre-Stroke | ||||
| No | 603 (97.7) | 14 (2.3) | 1 | |
| Yes | 55 (98.2) | 1 (1.8) | 0.78 (0.10-6.07) | 0.815 |
| REDO | ||||
| No | 638 (98.9) | 7 (1.1) | 1 | |
| Yes | 20 (71.4) | 8 (28.6) | 36.5 (12.0-110.3) | <0.001*** |
| PAD | ||||
| No | 440 (98.2) | 8 (1.8) | 1 | |
| Yes | 218 (96.9) | 7 (3.1) | 1.77 (0.63-4.93) | 0.278 |
| DM II | ||||
| No | 387 (97.5) | 10 (2.5) | 1 | |
| Yes | 271 (98.2) | 5 (1.8) | 0.71 (0.24-2.11) | 0.543 |
| Hyperlipidema | ||||
| No | 212 (97.7) | 5 (2.3) | 1 | |
| Yes | 446 (97.8) | 10 (2.2) | 0.95 (0.32-2.82) | 0.927 |
| Obesity | ||||
| No | 494 (97.8) | 11 (2.2) | 1 | |
| Yes | 164 (97.6) | 4 (2.4) | 1.09 (0.34-3.49) | 0.877 |
| Renalfailure(Creatinine>2.0 mg/Dl) | ||||
| No | 556 (97.9) | 12 (2.1) | 1 | |
| Yes | 102 (97.1) | 3 (2.9) | 1.36 (0.38-4.91) | 0.636 |
| COPD | ||||
| No | 451 (98.5) | 7 (1.5) | 1 | 0.072 |
| 1 | 125 (97.7) | 3 (2.3) | 1.55 (0.39-6.07) | 0.532 |
| 2 | 82 (94.3) | 5 (5.7) | 3.93 (1.22-12.7) | 0.022* |
| PRBC | ||||
| 0 | 560 (99.8) | 1 (0.2) | 1 | <0.001*** |
| 1 | 72 (97.3) | 2 (2.7) | 15.6 (139-173.0) | 0.026* |
| >=2 | 26 (68.4) | 12 (31.6) | 258.5 (32.3-2063) | <0.001*** |
| IABP | ||||
| No | 597 (98.4) | 10 (1.6) | 1 | |
| Yes | 61 (92.4) | 5 (7.6) | 4.89 (1.62-14.8) | 0.005** |
| Euroscore | 5.1 ± 3.9 | 11.8 ± 5.4 | 1.34 (1.20-1.49) | <0.001*** |
| Risk Euroscore | ||||
| Low | 373 (99.7) | 1 (0.3) | 1 | <0.001*** |
| Medium | 233 (97.5) | 6 (2.5) | 9.61 (1.15-80.2) | 0.037* |
| Severe | 52 (86.7) | 8 (13.3) | 57.4 (7.03-468.1) | <0.001*** |
| t-Qx | ||||
| <=3 H | 614 (94.8) | 1 (0.2) | 1 | <0.001*** |
| 3-4 H | 38 (79.2) | 10 (20.8) | 161.6 (20.1-295.4) | <0.001*** |
| >4 h | 6 (60.0) | 4 (40.0) | 409.3 (39.7-224.7) | <0.001*** |
Table 2: Extubation Outcome, Descriptive data: N (%) or media ± standard desviation(sd), Univariate binary logistic regression for each variable: No adjusted Odds Ratio (OR), 95%(CI) and p-value.
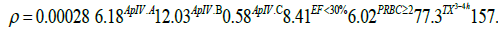
After performing multivariate logistic regression analysis and backward elimination method, the stronger predictor factors for UFTfailure were: transfusion of ≥ 2 PRCB revealed Adjusted OR (AOR=6.02) (95%CI) (p <0.05), t-Qx 3-4 h, (AOR=77.3)(95%CI) (p<0.001) and t-Qx >4 h, (AOR=157.5) (95%CI) (p<0.001). EF <30% had (OR=8.41) (95%CI) (p=0.059) (Table 3).
| UFT-Failure | ||
|---|---|---|
| AOR (95%CI) | p-value | |
| A.P(CCS) | ||
| Grade III | 1 | 0.035* |
| Grade IV-A | 6.18 (0.82-46.5) | 0.077 |
| Grade IV-B | 12.0 (1.66-87.3) | 0.014* |
| Grade IV-C | 0.58 (0.05-6.44) | 0.054* |
| Group LV (EF) | ||
| >=30% | 1 | |
| <30% | 8.41 (0.92-76.7) | 0.059 |
| PRBC | ||
| 0 / 1 | 1 | |
| >=2 | 6.02 (1.02-35.4) | 0.047* |
| t-QX | ||
| <=3 h | 1 | 0.002** |
| 3-4 h | 77.3 (6.04-991.4) | 0.001** |
| >4 h | 157.5 (8.73-2843.2) | 0.001** |
Table 3: UFT-failure: Extubation in UCI. A.P(CCS): Angina Pectoris Canadian Cardiovascular Society grades.LV: Left Ventricular, EF: Ejection Fraction PRBC: Packet Red Blood Cell Units Transfused. t-Qx: Surgery duration.
The equation of the predictive model for UFT-failure was:
where ρ is the probability for UFT-failure (Graphic 1).
ROC analysis and AUC=0.977 with optimum cut-off point of p=0.082 revealed a sensitivity 93.3% and specificity 95.6% of predictive model for UFT-failure (Graphic 1.1).
Graph 1.1 :ROC for predictive model of UFT-failure At Cut-off p=0.5: AUC (95% CI): 0.977 (0.954-1.000); Sensitivity (%): 46.7%; Specificity (%): 99.4%; Youden´s indexa: 0.459 Cut-off p=0.082: Sensitivity (%):93.3%; Specificity (%): 95.6%; Youden´s indexa: 0.889 Diagnostic validity of predictive model for UFT-failure: ROC analysis and discrimination threshold (cut-off points)
Univariate analysis revealed as significant predictors or independent risk factors for Hosp-LOS >4 days: Age >80 yo ,female sex, NYHA>III, EurosCORE, severity of Angina pectoris CCS, EF <30%, Redo, Renal failure, IABP, PRCB transfusion, UFT-failure failure , t-Qx and ICULOS (p <0.001).Transfusion of 1 PRCB increased 48.8 times the risk of Hops-LOS >4 days, and transfusion of ≥ 2 PRCB showed (OR= 686) (95%CI) (Table 4).
| N(%) / mean ± sd | OR (95%CI) | p-value | ||
|---|---|---|---|---|
| HOSP-LOS | ||||
| <=4 d | >4 d | |||
| Patients | 633 (94.1) | 40 (5.9) | ||
| Age (Y) | 60.9 ± 9.2 | 71.0 ± 9.6 | 1.11 (1.08-1.15) | <0.001*** |
| Group Age | ||||
| <=80 y | 611 (95.3) | 30 (4.7) | 1 | |
| >80 y | 22 (68.8) | 10 (31.3) | 9.26 (4.03-21.3) | <0.001*** |
| Gender | ||||
| Male | 503 (97.1) | 15 (2.9) | 1 | |
| Female | 130 (83.9) | 25 (16.1) | 6.45 (3.31-12.6) | <0.001*** |
| Smoker | ||||
| No | 210 (92.5) | 17 (7.5) | 1 | |
| Yes | 423 (94.8) | 23 (5.2) | 0.67 (0.35-1.29) | 0.229 |
| NYHA | ||||
| Class I | 59 (81.9) | 13 (18.1) | 1 | <0.001*** |
| Class II | 375 (97.4) | 10 (2.6) | 0.12 (0.05-0.29) | 0.017* |
| Class III | 140 (93.3) | 10 (6.7) | 0.32 (0.14-0.78) | 0.012* |
| Class IV | 59 (89.4) | 7 (10.6) | 0.54 (0.20-1.45) | 0.219 |
| CAD | ||||
| 1 vessel | 40 (100) | 0 (0) | 1 | |
| 2 vessels | 51 (96.2) | 2 (3.8) | ||
| 3 vessels | 542 (93.4) | 38 (6.6) | 3.19 (0.76-13.4) | 0.114 |
| Left Main Stem | ||||
| No | 517 (94.5) | 30 (5.5) | 1 | |
| Yes | 116 (92.1) | 10 (7.9) | 1.49 (0.71-3.13) | 0.297 |
| AP(CCS) | ||||
| Grade III | 340 (95.8) | 15 (4.2) | 1 | 0.003** |
| Grade IV-A | 136 (94.4) | 8 (5.6) | 1.33 (0.55-3.22) | 0.522 |
| Grade IV-B | 119 (93.7) | 8 (6.3) | 1.52 (0.63-3.69) | 0.35 |
| Grade IV-C | 38 (80.9) | 9 (19.1) | 5.37 (2.20-13.1) | <0.001*** |
| HTA | ||||
| No | 110 (86.6) | 17 (13.4) | 1 | |
| Yes | 523 (95.8) | 23 (4.2) | 0.29 (0.15-0.55) | <0.001*** |
| Lv Function (Ef) | 47.3 ± 10.2 | 46.3 ± 10.5 | 0.99 (0.96-1.02) | 0.544 |
| Group Lv Function (Ef) | ||||
| >50% | 320 (95.5) | 15 (4.5) | 1 | 0.042* |
| 30%-50% | 278 (93.6) | 19 (6.4) | 1.46 (0.73-2.92) | 0.288 |
| <30% | 35 (85.4) | 6 (14.6) | 3.66 (1.33-10.0) | 0.012* |
| Myocardial Infarction | ||||
| No | 323 (94.4) | 19 (5.6) | 1 | |
| Yes | 310 (93.7) | 21 (6.3) | 1.15 (0.61-2.18) | 0.665 |
| Pre-Stroke | ||||
| No | 581 (94.2) | 36 (5.8) | 1 | |
| Yes | 52 (92.9) | 4 (7.1) | 1.24 (0.43-3.62) | 0.692 |
| REDO | ||||
| No | 629 (97.5) | 16 (2.5) | 1 | |
| Yes | 4 (14.3) | 24 (85.7) | 235.9 (73.2-59.2) | <0.001*** |
| PAD | ||||
| No | 425 (94.9) | 23 (5.1) | 1 | |
| Yes | 208 (92.4) | 17 (7.6) | 1.51 (0.79-2.89) | 0.213 |
| DM II | ||||
| No | 373 (94.0) | 24 (6.0) | 1 | |
| Yes | 260 (94.2) | 16 (5.8) | 0.96 (0.50-1.84) | 0.893 |
| Hyperlipidema | ||||
| No | 202 (93.1) | 15 (6.9) | 1 | |
| Yes | 431 (94.5) | 25 (5.5) | 0.78 (0.40-1.51) | 0.464 |
| Obesity | ||||
| No | 478 (94.7) | 27 (5.3) | 1 | |
| Yes | 155 (92.3) | 13 (7.7) | 1.49 (0.75-2.95) | 0.259 |
| Renal Failure | ||||
| No | 543 (95.6) | 25 (4.4) | 1 | |
| Yes | 90 (85.7) | 15 (14.3) | 3.62 (1.84-7.13) | <0.001*** |
| COPD | ||||
| No | 436 (95.2) | 22 (4.8) | 1 | 0.194 |
| 1 | 117 (91.4) | 11 (8.6) | 1.86 (0.88-3.95) | 0.105 |
| 2 | 80 (92.0) | 7 (8.0) | 1.73 (0.72-4.19) | 0.222 |
| PRBC | ||||
| 0 | 559 (99.6) | 2 (0.4) | 1 | <0.001*** |
| 1 | 63 (85.1) | 11 (14.9) | 48.8 (10.6-225.1) | <0.001*** |
| >=2 | 11 (28.9) | 27 (71.1) | 686.0 (144.8-3249) | <0.001*** |
| IABP | ||||
| No | 576 (94.9) | 31 (5.1) | 1 | |
| Yes | 57 (86.4) | 9 (13.6) | 2.93 (1.33-6.47) | 0.008** |
| Euroscore | 4.9 ± 3.9 | 9.3 ± 4.9 | 1.24 (1.15-1.32) | <0.001*** |
| Risk Euroscore | ||||
| Low | 365 (97.6) | 9 (2.4) | 1 | <0.001*** |
| Medium | 219 (91.6) | 20 (8.4) | 3.70 (1.66-8.28) | 0.001** |
| Severe | 49 (81.7) | 11 (18.3) | 9.10 (3.59-23.1) | <0.001*** |
| t-QX | ||||
| <=3 H | 611 (99.3) | 4 (0.7) | 1 | <0.001*** |
| 3-4 h | 20 (41.7) | 28 (58.3) | 213.9 (68.5-667.6) | <0.001*** |
| >4 h | 2 (20.0) | 8 (80.0) | 611.0 (97.5-3828.4) | <0.001*** |
| Extubation | ||||
| UFT-Success | 628 (95.4) | 30 (4.6) | 1 | |
| UFT-Failure | 5 (33.3) | 10 (66.7) | 41.9 (13.5-130.2) | <0.001*** |
| ICU-LOS | ||||
| <=24 h | 628 (98.7) | 8 (1.3) | 1 | |
| >24-72 h | 5 (29.4) | 12 (70.6) | 502.4 (155.5-1622) | <0.001*** |
| >72 h | 0 (0.0) | 20 (100) | ||
Table 4: Independent variables associated with Hospital length of Stay (HOSP-LOS), Descriptive data: N (%) or media ± standard desviation (sd), Univariate binary logistic regression for each variable: No adjusted Odds Ratio (OR), 95%(CI) and p-value.
Multivariate analysis and backward elimination method revealed as stronger predictor factors for Hosp-LOS>4 days the following variables:
t-Qx >3 h (AOR > 74) (95%CI) (p <0.001) and ICU-LOS >24 h (AOR=29.3) (95%CI) (p <0.001) and Redo (AOR=7.68) (95%CI) with an important statistic tendency (p=0.059).. Preoperative use of IABP reduce risk of Hosp >4 days, (AOR=0.06, 0.01-0.51) ((p=0.01) (Table 5).
| HOSP-LOS >4 days | ||
|---|---|---|
| AOR (95%CI) | p-value | |
| REDO | ||
| No | 1 | |
| Yes | 7.68 (0.93-63.4) | 0.059 |
| IABP | ||
| No | 1 | |
| Yes | 0.06 (0.01-0.51) | 0.010* |
| t-QX | ||
| <=3 h | 1 | 0.001*** |
| 3-4 h | 74.2 (15.4-358.2) | <0.001*** |
| >4 h | 95.1 (3.96-2285.9) | 0.005** |
| ICU-LOS | ||
| <=24 h | 1 | |
| >24 h | 29.3 (4.44-193.1) | <0.001*** |
Table 5: Independient risk factors associated with Hosp-LOS >4 days Multiple binary logístic regression: Adjusted odds ratio (AOR) by backward elimination method, 95%(CI) and p-valor.
The equation of the predictive model for prolonged Hosp-LOS was:
where ρ is the probability to Hosp-LOS >4 days (Graphic 2).
ROC analysis and AUC=0.972 with optimum cut-off point of p=0.016 revealed a sensitivity 95.0% and specificity 96.4 % of predictive model for Hosp-LOS >4 days (Graphic 2.1).
Previous studies have reported possible contraindications to early extubation including obesity, female sex, excessive bleeding, inotropic support, use of IABC, hypothermia, prolonged extracorporeal circulation, and prolonged surgery time [17]. While UFT anesthesia management may not yet be common practice in myocardial revascularization surgery in every practice, published reports have noted that immediate extubation in the Op.Room after cardiac surgery is feasible, safe, and, moreover, has benefits compared to later extubation. [2,3,5].
An aim of this study was to describe the short-term outcome (≤ 30 days) of a consecutive case-series of 673 patients managed by a combination of desflurane, remifentanil, and intercostals nerve block in OPCAB procedures by LAT surgical approach and followed up by multidisciplinary enhance recovery pathway, a “preliminary” protocol including preoperative patient and family educational material, preoperative training and consensus-based standard perioperative management protocol [13-15] (Supplementary 1).
Our patients, a heterogeneous group with varying levels of risk, generally spent a short time in the ICU (94.5% of patients left the ICU within 24 h) and short Hosp-LOS with relatively low rates of morbidity (2.1% were readmitted to the ICU) and mortality (1.6%). In most of our cases, 94.1.8% of patients had Hosp-LOS ≤ 4 days, and followed by a week of at-home nursing care, enabling our patients to return to their daily activities as quickly as possible. We defined as prolonged Hospitalization as length of stay>4 days due to the observation of our previous case-series [10]; our cut-off matches with others publications [18].
The safety of ICU discharge within the first 24 h after a CABG has been previously described 18 and UFT has not been associated with an increased incidence of readmission to the ICU or hospital [19]. In our case-series ,the univariate logistic regression analysis found many factors that influenced to increase the probability for UFT-failure, including female gender and age >80 y.o. Others independent variables were significantly associated with UFT-failure such as EuroSCORE, severity of angina pectoris, previous diagnostic of COPD and COPD severity, poor LV function and PRBC transfusion. While the literature does not suggest that advanced age is a contraindication for UFT anesthesia [20], female patients and age >80 y.o are nevertheless at risk for longer ICU-LOS and Hosp-LOS. However, the strongest risk factors for UFT-failure were revealed by multivariate analysis: Severity of angina pectoris, poor LV function, PRCB transfusion and duration of surgery. In fact, surgery time >3 h increase 70 times the risk of UTF failure, in the same way, transfusion of ≥ 2 PRCB increase 6 times the risk for UFT-failure and Angina Pectoris grade IV up to 12 times. EF<30% showed a very strong negative influence over success of UTF.
In our study, only 6 patients (0.9%) had postoperative neurological dysfunction and stroke, very low stroke rate in comparison with others series of CABG with CBP. On the other hand, OPCAB together with the non-aortic touch technique, especially in the elderly with advanced atherosclerotic disease, avoids the deleterious effects of CPB and reduces the risk for cerebral embolism [21]. Further, no differences have been found in recall and intraoperative awareness compared with traditional management [22].
Conventional anesthetic techniques incorporate high doses of opioids such as fentanyl and sufentanil to reduce intraoperative oxidative stress and sympathetic-adrenergic stimulation, those are associated with more than 3-6 hours of mechanical ventilation, require more IV fluids or vasopressors, and require more than 24 h in the ICU. This prolonged time to emergence delays hospital discharge and could be associated with poorer outcomes [23].
In our case-serie only 40 patients (5.9%) had a Hosp-LOS >4 days. Majority of the independent variables associated with UFT-failure, also were associated with prolonged hospitalization .Additionally, univariate analysis identifies NYHA functional class, renal failure, Redo and UCILOS (p <0.001) as risk factors for Hosp-LOS >4 days. Multivariate analysis with backward elimination method showed the duration of surgery (t-Qx>3 hrs) (AOR>75) and ICU-LOS>24 h (AOR=30) (p<0.001) as the strongest risk factors for prolonged Hosp-LOS. Otherwise, because the use of elective IABP prevented intra-operative complications in the high-risk patients, it may reduce the probability of prolonged Hosp-LOS, AOR=0.06 [0.01-0.51] (95%CI) in this particular group. Elective IABP was used to support and maintain hemodynamic stability during graft construction in our high-risk patients with left main coronary artery disease, unstable angina, recent MI, reoperation and/or EF ≤ 30%. We believe that prophylactic use of IABP may reduce the need for CPB support and emergency sternotomy which could be caused by ischemic events during anastomosis, thus reducing mortality among the patients in our study with the highest risk [24]. In addition, we used femoro-femoral CBP support to keep the heart beating without emergent sternotomy in 0.4% of our patients
The cornerstone of UFT anesthesia is multimodal perioperative analgesia including regional and local anesthesia based on American Pain Society guidelines [25]. In our protocol, the use of remifentanil, a short-acting opioid with a very rapid context-sensitive half-life, allows for profound analgesia during surgery without prolonged respiratory depression and with faster emergence. The use of volatile agents (desflurane or sevoflurane) is associated with reduced morbidity and mortality in CABG due to their cardioprotective effects. The choice of an anesthetic regimen based on the administration of these halogenated anesthetics is associated with a better outcome after coronary cardiac surgery [26,27]. We believe that the combination of desflurane and remifentanil, both of which have cardioprotective effects against ischemic reperfusion injury [26-28] has also contributed to our outcomes. Extubation in the Op.Room is especially achievable when OPCAB is used, as it decreases operating time and avoids the pathophysiological changes that are generally induced by CPB [8,29].
TEE is a minimally invasive technique to monitor left ventricular segmental wall motion during OPCAB surgery, but its greatest utility occurs after reperfusion [30]. Persistent segmental wall motion abnormalities after revascularization could prompt the surgeon to reassess the patency of the coronary bypass graft, which would then reduce the likelihood of postoperative angina pectoris or MI. The rate of postoperative MI in our study was 0.6%.
We believe that avoiding CPB, maintaining normothermia, using tranexamic acid and maintaining a meticulous surgical technique contributed to an acceptable rate of postoperative bleeding without an important increment of ischemic coronary, stroke, or thromboembolic events. Use of the LAT surgical approach could be another factor. Sternotomy is a faster approach, especially in hemodynamic emergencies, and may produce less pain than a traditional posterolateral thoracotomy, however, its association with periosteal reaction and marrow bleeding are concerning.
Although only 16.6% of our patients required blood transfusions (a result of eschewing CPB and following strict transfusion criteria), Hosp-LOS was nevertheless higher for those patients who received transfusions and were not extubated in the Op.Room (p<0.001). Our results match Scott et al. 9 so we found that Hosp-LOS>4 days was, in fact, a function of bleeding and needs of transfusions, OR=686 [144.8- 3,249] (95% CI ). Also, our results matches Zakhary [31], who found similar association between extubation outcome and age, sex, duration of surgery >3 h.
The precision of the predictive model for extubation outcome is high (AUC=97.7%), and particularly regarding specificity ability (99.4%). Moreover, with an optimum cut-off to estimate the probability for UFT-failure, the model achieved an increases of Sensibility (93.3%) and keeping good Specificity (95.6%).Additionally, the precision of the predictive Hosp-LOS model is high (AUC=97.2%), Sensibility 95% and Specificity 96.4% with an optimum cut-off point according to Youden Index. We encourage other authors to validate these proposal predictive models, but it is important to take into account our surgical approach.
Our study has limitations, including its descriptive nature and lack of long-term outcome data. In addition, we did not compare our work with those managed by CPB and UFT, neither we compared our results with pre-ERAS series (it is a preliminary protocol that has been recently testing since 2009). According to the literature, we think that standardizing an ERAS protocol for UTF-OPCAB management may be the most reasonable way to obtain the best results 15, but it must be confirmed by next randomized studies. Nevertheless, for more than 15 years we have used predominantly OPCAB by LAT approach with good results. Unfortunately, we did not include our cases-series before 2010 because with used various types of hypnotics for induction and other volatile agents.
In conclusion, the management described in this study allows very rapid recovery as well as a short ICU and Hosp- LOS, offering the possibility of cost reduction; this fact has permitted us to help a vast number of cardiac patients at our centre for years [32]. In general, age >80 y.o, female sex, severity of EuroSCORE and ≥ 2 PRBCs transfusion were risk factor for UTF-failure and prolonged Hosp-LOS .However, our study has developed two predictive models with high diagnostic validity for UFT-failure and prolonged Hosp-LOS that include as stronger perioperative risk factor transfusion of ≥2 PRCB, severity of angina pectoris, Redo, duration of surgery >3 hrs and ICU-LOS >24 hrs. More multicenter prospective studies with the aim of determining which variables are associated with increased risk for postoperative bleeding; UFT-failure, prolonged ICU-LOS and prolonged Hosp- LOS would enable better management of cardiac surgery patients and perhaps encourage the use of bloodless medicine techniques.
Ethical disclosures
Protection of human and animal subjects: The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data: The authors declare that no patient data appear in this article.
Right to privacy and informed consent: The authors declare that no patient data appear in this article. The ethics committee of the hospital (Fundacardio Fundation) approved to use the clinical information of the cases by providing us with a coded database for the retrospective review following strict compliance with the regulations of personal data protection.
The authors declare that they have no competing interests.
To access the data and all statistical process, please feel free to contact Mr. Juan Luis Gómez Martínez, statistical advisor of St. Halley Statistics by E-mail: juanluisgomez@sthalley.com (Supplementary 2).
We would like to thanks Mr. Juan Luis Gómez Martínez, statistical advisor of St. Halley Statistics for all the support he gave us, statistical guidance and patience.