Andrology-Open Access
Open Access
ISSN: 2167-0250
ISSN: 2167-0250
Short Communication - (2023)Volume 12, Issue 1
Peyronie's Disease (PD) affects up to 20% of males worldwide [1,2]. The pathophysiology of the disease has been postulated as repeated injuries into the Tunica Albuginea (TA) during intercourse [2]. This article focuses on literature pertaining surgical innovations published in the last 20 years. Some innovations did not have good outcomes, while others were undervalued or not allowed enough time to generate data that contributes information on long-term outcomes.
Surgical management of PD is indicated when the curvature causes enough distress to prevent the patients from having intercourse. This distress can be a result of the pain (their own and/or their partners) and the difficulty or utter inability of penile penetration [1,2].
The American Urological Association and European Association of Urology guidelines advise that curvature magnitude should guide treatment choice. In a nutshell, plication for curvatures <60˚ and grafting procedures for hinge defects, hourglass and complex curvatures ≥ 60˚ [1,2].
After the curvature, loss of penile length is the most common complaint [3]. The PD pathophysiology involves the replacement of normal TA with fibroid scar tissue. The myofibroblasts contract, decreasing the gap in the TA injury, further being replaced by collagen fibers preventing the area from stretching during the erection. After these fibers organize, they form the plaque responsible for the clinical findings of PD [4].
The primary objective to be observed when operating a PD patient is restoring penile function [1,2]. This author has a second objective: Restore penile anatomy as closely to pre-disease state. These two principles may look the same, but they are not.
Restoring the penile function aims to habilitate the penis for penetration. It does not necessarily restore the penis to its previous anatomy. Plications may correct the curvature but inevitably shorten the penis, making the long side of the curvature even to the short side.
Patients with minor curvature angles may not be bothered by losing a few millimeters in length. However, complex anatomical defects associated with penile length loss will demand more advanced surgical skills. This mainly consists of making the shorter side even with the longer one followed by a graft of the tunica defect (Figures 1A and 1B) [5].
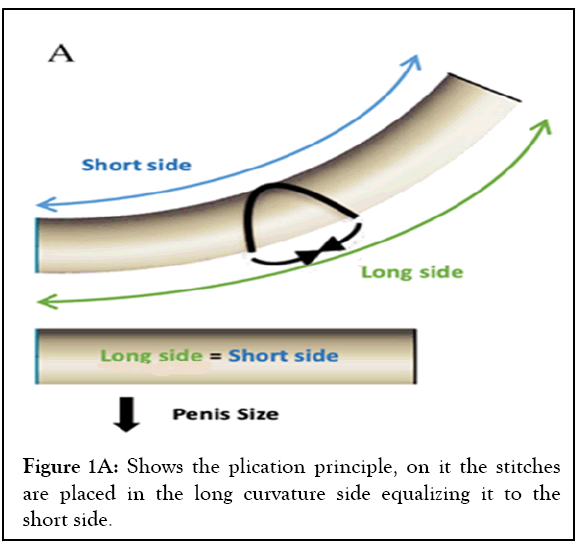
Figure 1A: Shows the plication principle, on it the stitches are placed in the long curvature side equalizing it to the short side.
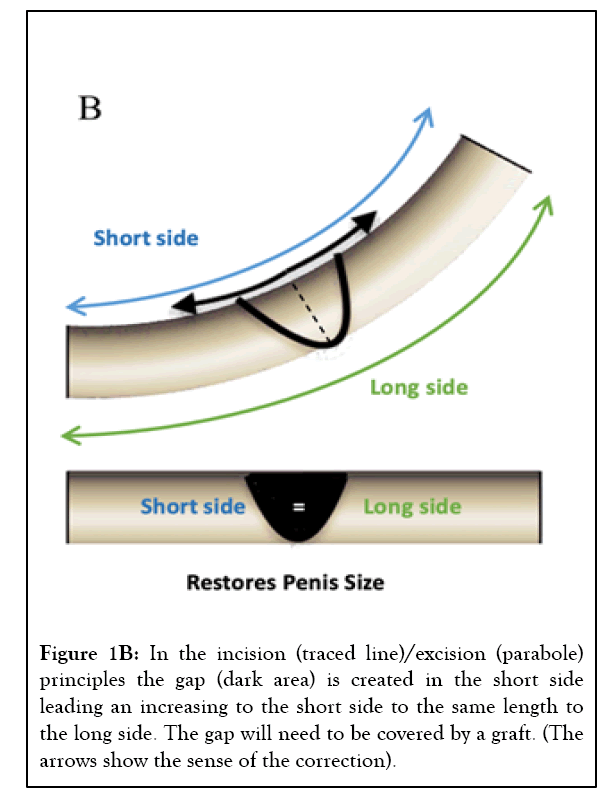
Figure 1B: In the incision (traced line)/excision (parabole) principles the gap (dark area) is created in the short side leading an increasing to the short side to the same length to the long side. The gap will need to be covered by a graft. (The arrows show the sense of the correction).
The correlation between the grafting size/area and ED incidence is well-established. Larger grafts increase the odds of developing ED in the post-operatory period [6,7]. Classically, the grafting surgery for PD without penile prosthesis can be excisional, which consists of resection of the plaque; partially excisional, where only a segment of the plaque is resected or incisional in which there is no plaque resection (Figures 2A-2C).
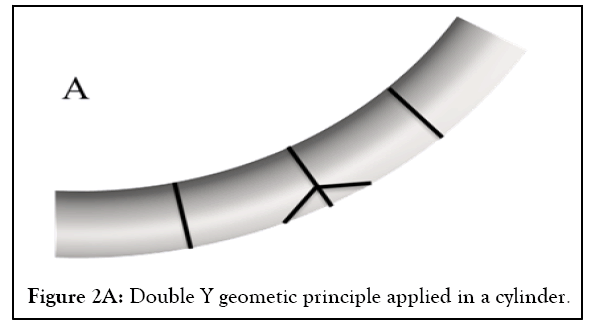
Figure 2A: Double Y geometic principle applied in a cylinder.
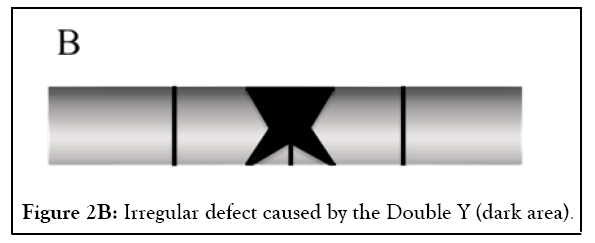
Figure 2B: Irregular defect caused by the Double Y (dark area).
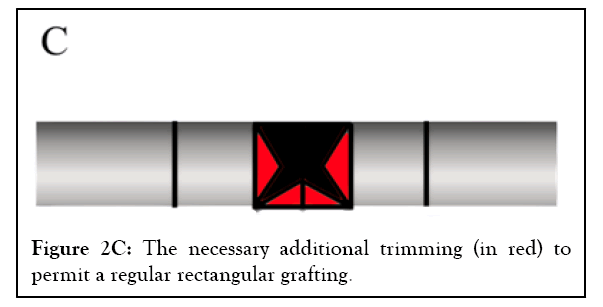
Figure 2C: The necessary additional trimming (in red) to permit a regular rectangular grafting.
Incisional techniques cause less damage to the erectile sinusoid tissue when compared to excisional ones. The double Y is among the most utilized incisional techniques it leads to irregular TA defects and large grafting areas [3,5]. The irregular edges will need trimming for a good grafting placement [8,9] (Figures 3A-3C).
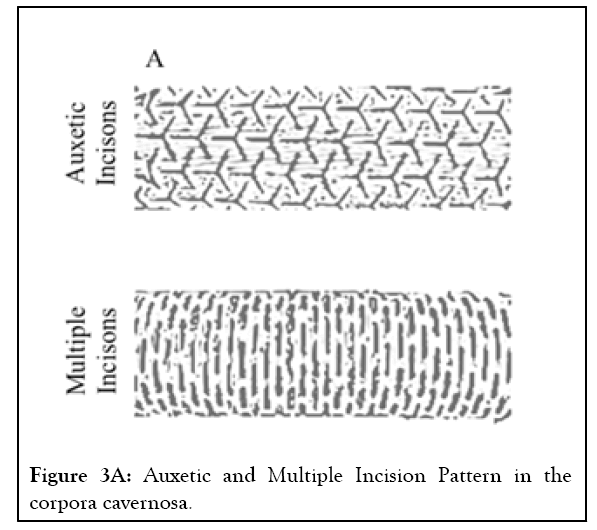
Figure 3A: Auxetic and Multiple Incision Pattern in the corpora cavernosa.
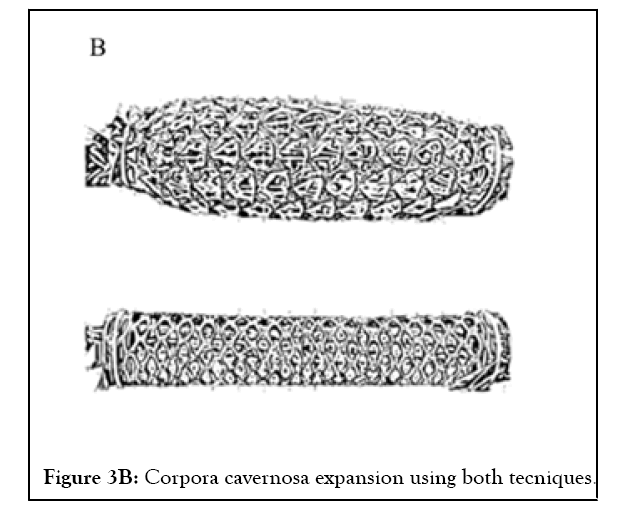
Figure 3B: Corpora cavernosa expansion using both tecniques.
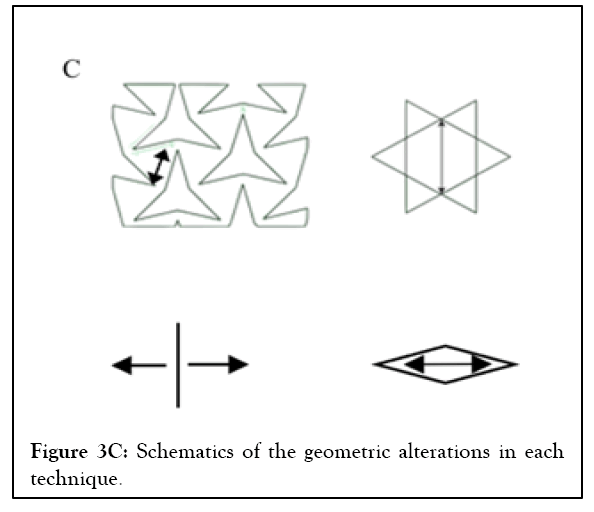
Figure 3C: Schematics of the geometric alterations in each technique.
Another consideration to be taken when grafting a patient is the final biomechanical aspect. In 2014 it was postulated that the double Y does not fix the penile mechanical alterations [9], which can further contribute to post-operatory ED. In 2016, an innovative mathematical method for decreasing the grafting area with a pure incisional technique was published (iGrafter ) [10]. No other articles using the iGrafter were published after this. Last year, a group compared the Double Y vs. iGrafter , using 3D printed models with a standard dorsal monoplane curvature. The results show that the iGrafter decreased the grafting area by 50.2% compared to the double Y [11].
The grafting materials are other factors to consider. Autologous grafting has recently been replaced for heterologous grafts due to more promising results and decreased operative times. Synthetic graft materials were tested in the past with poor results. In the last few years, some European surgeons using Tachosil as grafting material report good results [2,12]. In animal models, PD is induced by injecting fibrinogenic substances into the TA [4]. In this author's opinion, using a fibrinogenic agent as grafting material seems counterintuitive in a disease where the pathophysiology is fibrin-collagen deposition.
In patients with PD associated ED, the implantation of a Penile Prosthesis (PP) is indicated. The curvature can be repaired using the same strategies for non-ED patients (i.e., plication and grafting). Minor curvatures can sometimes be corrected by placing the PP alone or adding maneuvers as the modeling after the PP placement [1,2,5].
Since 2012, innovative techniques to correct PD using PP have been described: Circular grafting [13], Sliding technique [14], Modified Sliding Technique (MoST) [15], and Multiple Slit Technique (MuST) [16].
In 2020, the TA mesh concept was published. On it, the surgeon performs small incisions in the TA, expanding the tissue, breaking the PD plaque, and correcting the curvature and any hinges in the penis. The author claimed that his technique could recover the penis' length and girth to pre-PD dimensions [17].
A translational research article published in 2021 proposed using the auxetic principle to correct any fibrotic penile alteration with fabric models. It compared the auxetic incisions to the mesh model and demonstrated that these incisions, when expanded, dilate the fabric cylinder in triangles increasing the penile length and circumference. Using the same fabric model, the authors demonstrated that the mesh model could expand the cylinder only in one aspect: Length or circumference, depending on how the mesh incisions are made [18]. A video with the auxetic technique in a patient is available [19], but an article has yet to be published showing long-term results in various cases.
It is important setting realistic expectations about outcomes with the patient. Having a better understanding of penile biomechanics and its effects on erections helped develop new surgical advances that can decrease the chance of ED in patients who have preserved EF. In patients in which ED is already present, this knowledge acquired aided in developing new TA expansion techniques that have promising results in restoring the penis anatomy close to its previous PD aspect.
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
[CrossRef] [Google Scholar] [Pubmed]
Citation: Machado B, Jaime FF (2023) Peyronie's Disease: Are We Offering the Best to Our Patients? A Critical Comment on the Current Literature and an Optimistic Look into the Future. Andrology.12:278
Received: 10-Feb-2023, Manuscript No. ANO-23-21765; Editor assigned: 13-Feb-2023, Pre QC No. ANO-23-21765; Reviewed: 27-Feb-2023, QC No. ANO-23-21765; Revised: 06-Mar-2023, Manuscript No. ANO-23-21765; Published: 13-Mar-2023 , DOI: 10.35248/2167-0250.23.12.278
Copyright: © 2023 Machado B, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.