Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Case Report - (2022)Volume 13, Issue 4
Purpose: To observe and describe a rare disease Phacomatosis Pigmentovascularis as case series.
Case: Detailed history taking and examination was done in the glaucoma clinic of Chittagong Eye Infirmary and Training Complex (CEITC) for the diagnosis of those suspected cases. Detailed systemic examinations of skin, cardiac and nervous system were done. Ocular examinations included visual acuity, intraocular pressure, gonioscopy (while possible), torch light and slit lamp examination and fundus evaluation were done.
Results: Total of 8 cases were included (Five male and three female). Average age group was 4+/-2 years. All of them had haemangiomatous lesion in the hand and feet. Five of them had haemangioma in the both side of the face. Five cases had bilateral and rest two had unilateral naevus of ota in the eye. Three cases had bilateral and rest five cases had unilateral mild buphthalmos and raised intraocular pressure (IOP). There was history of convulsion in two cases and CT brain revealed calcification in the brain. All cases needed trabeculectomy surgery to reduce IOP. Two cases needed Ahmed valve implant.
Conclusion: Phacomatosis pigmentovascularis is a rare entity. Early diagnosis and appropriate measurement can save their vision as well as life.
Haemangioma; Phacomatosis; Buphthalmos; Galucoma; Trabeculectomy
Phacomatosis Pigmentovascularis (PPV) is a disorder characterized by the co-existence of vascular and pigmentary birthmarks [1]. Signs and symptoms may include port wine stain, melanocytic nevi (commonly known as moles), epidermal nevi, dermal melanocytosis (areas of blue-gray discoloration), nevus spilus and patches of hyperpigmentation (areas of darker skin). Other skin features may include nevus anemicus (areas of lighter skin) and café au lait spots [2]. About half of people with PPV have systemic involvement, which means they have features affecting other areas of the body. People with systemic involvement may have neurologic, ocular (eye), or muscular abnormalities [2,3]. Several subtypes of PPV have been identified which are generally distinguished based on the specific type(s) of skin features present [1,2].
This is a observational case series study done for the last 7 years at the glaucoma clinic of CEITC. Patient presented in the paediatric outdoor with vascular malformation in the face were referred to the glaucoma clinic for detail evaluation. In glaucoma clinic history taking like ocular pain, photophobia, headache, and convulsion were taken and some examinations like vision, refraction, pupillary reaction, IOP measurement by digitally or by applanation tonometry, torchlight and or slit lamp examination and fundoscopy were done. Those patients had vascular malformation in and around the face we checked for oculocutaneous naevus, conjunctival vascular malformation and megalocornea. We did fundoscopy to exclude any glaucomatous change in the disc or haemangioma in the retina and choroid. Fundus photography was done where possible. CT scan of the brain was done while there was a history of convulsion and while it is affordable to the patient. Raised intraocular pressure was managed by trabeculectomy surgery. Tube implantation was done in the failed cases.
Among total 8 cases five of them were male and three female. Average age group was 4 +/-2 years. Older one was 6 years and younger was 2 years of age. All of them had haemangiomatous lesion in the hand and feet. But the oldest one had massive haemangioma in the trunk also associated with pachy naevus all over the body. Five of them had haemangioma in the both side of the face (Figure 1). Three of them had upper lid swelling in the affected side. Five cases had bilateral and rest two has unilateral naevus of ota in the eye those were distributed following a dermatome of frontal and maxillary division of trigeminal nerve. Three cases had bilateral and rest five cases had unilateral mild buphthalmos and raised IOP. Average IOP was 25+/-5 mmHg where it was possible to be measured. IOP was more where haemangiomatous lesion was more prominent. In two cases there was history of convulsion and CT brain revealed calcification in the brain. All of them were treated with brinzolamide and timolol combination two times daily for reduction of IOP but was not possible to be reduced. Fundus examination revealed C:D of average 0.8:1 except two cases where it was almost full cupping. All cases needed trabeculectomy surgery to reduce IOP. Two cases needed Ahmed valve implant. In two cases IOP was not controlled where Ahmed valve implantation has been planned (Figure 2).

Figure 1: Haemangiomatous changes in the both side of the face with buphthalmos in the right side.
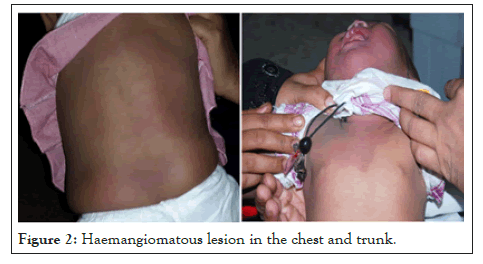
Figure 2: Haemangiomatous lesion in the chest and trunk.
Isolated PPV is typically a sporadic disorder that occurs for the first time in people with no family history of PPV [4]. Researchers have found that PPV can be caused by a somatic mutation in the GNA11 or GNAQ gene that is present only in the affected tissues of the body. These mutations are not present in the blood or in unaffected tissues, which means the disorder is likely due to non-inherited mutations that are randomly acquired after conception. In some cases of isolated PPV, the underlying cause remains unknown [1]. There is no family history of such disease in our cases and we did not do any genetic analysis.
Treatment and long-term outlook (prognosis) of PPV largely depends whether there is systemic involvement and which body parts or organ systems are affected [3,4]. Isolated PPV without systemic involvement typically does not require treatment. However, large skin lesions may cause problems with body image and self-esteem, so laser treatments may be considered to improve the appearance of skin. In our cases we referred the patient to the skin specialist and they were under observation.
Characteristic signs and symptoms of Phacomatosis Pigmentovascularis (PPV) involving the skin include port wine stain and various pigmentary lesions (lesions that are brown, black or blue in color). The port wine stain and pigmentary lesions may be extensive, affecting several areas of the body, including the face. Examples of associated pigmentary lesions include [2,3].
• Melanocytic nevi
• Epidermal nevi
• Nevus anemicus (areas of lighter skin)
• Hyperpigmentation (areas of darker skin)
• Cafe-au-lait spots
• Dermal melanocytosis (areas of blue-gray discoloration)
• Nevus of Ota
In our series they were presented with vascular malformation in the face and trunk and also in the limb as well as with naevus over face and in the eye (conjunctiva). Around half of people with PPV have systemic involvement (i.e., body systems other than the skin are affected). Eye conditions such as ocular melanosis (also called ocular melanocytosis) are common. Ocular melanosis refers to a blue-gray pigmentation in the white of the eye (the sclerae). This condition often occurs along with nevus of Ota and may affect one or both eyes [5]. In our series five cases had bilateral and two cases had unilateral naevus in the face and eye. Naevus follows the dermatome of T1 and T2.
Eye naevus is subconjunctival melanocytosis in nature. Complications of nevus of Ota include glaucoma and melanoma, so people with nevus of Ota require careful examination and follow-up by an ophthalmologist [6,7]. Other eye conditions reported in PPV include iris hamartomas, iris mammillations and iris nodules. When neurologic abnormalities are present they usually become apparent in the first few months of life and may include developmental delay, seizures, intracranial calcifications (calcium deposits within the brain) or cerebral atrophy [3]. Some people with PPV also have Sturge-Weber syndrome or Klippel- Trenaunay syndrome, each of which causes various signs and symptoms [8]. Two of our cases had cerebral calcification in the CT scan. In almost all of our cases there was secondary glaucoma. The pathogenesis is combined. Developmental anomaly, raised episcleral venous pressure and melanocyte accumulation in the angle were the mechanism. We did gonioscopy in two cases where we found angle anomaly and hyperpigmentation of the angle.
A variety of other signs or symptoms have been reported in individual cases of PPV (e.g., primary lymphedema, renal angiomas, moyamoya disease, scoliosis, malignant colonic polyposis, hypoplastic larynx, multiple granular cell tumors, and selective IgA deficiency) [9]. In our series we, did not get such association so far.
If Phacomatosis Pigmentovascularis (PPV) is not associated with systemic complications (e.g., Sturge-Weber Syndrome, Klippel- Trenaunay syndrome, neurological problems or eye conditions) it typically does not require treatment. However, because large skin lesions may cause problems with body image and self-esteem, parents of children with PPV, or adults with PPV, may consider laser treatments to improve the appearance of skin lesions [5,6].
Glaucoma in such cases is usually refractory to medicine and also standard trabeculectomy. So trabeculectomy with antimetabolites is comparatively better option. But there is no published report over it. But in the Sturge Weber Syndrome, trabeculectomy with mitomycin-C yields good result. In our series four cases were doing good with trabeculectomy with mitomycin-C but in other cases IOP was raised again and we did Ahmed valve implantation in two cases and two cases we have planned to do so.
We are now following those cases for final outcome of the surgery. Phacomatosis Pigmentovascularis is a rare entity. Combined management from dermatologist, neurologist and ophthalmologist are needed to handle those multisystem complex cases. Uncontrolled intraocular pressure may cause blindness. Early diagnosis and appropriate medical and surgical management is mandatory to save the eye from blindness.
The authors thank the parent of the child patient for allowing the case to be published.
[Crossref] [GoogleScholar] [PubMed]
[GoogleScholar] [PubMed].
[Crossref] [GoogleScholar] [PubMed].
[Crossref] [GoogleScholar] [PubMed]
[Crossref] [GoogleScholar] [PubMed]
[Crossref] [GoogleScholar].
[Crossref] [GoogleScholar] [PubMed].
Citation: Noman SM, Akbar US, Haque M, Islam M, Sarkar D, Kaoser S (2022) Phacomatosis Pigmentovascularis: A Case Report. J Clin Exp Ophthalmol. 13:921.
Received: 05-Apr-2022, Manuscript No. JCEO-22-15890; Editor assigned: 07-Apr-2022, Pre QC No. JCEO-22-15890 (PQ); Reviewed: 21-Apr-2022, QC No. JCEO-22-15890; Revised: 28-Apr-2022, Manuscript No. JCEO-22-15890 (R); Published: 09-May-2022 , DOI: 10.35248/2155-9570.22.13.921
Copyright: © 2022 Noman SM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.