Journal of Clinical & Experimental Dermatology Research
Open Access
ISSN: 2155-9554
ISSN: 2155-9554
Research - (2020)Volume 11, Issue 3
Introduction: Large prospective studies evaluating efficacy of narrow band ultraviolet B (NB-UVB) in psoriasis in
terms of PASI75 and PASI90 are scarce in the literature.
Material and methods: A prospective, open and observational study was conducted. Patients treated with narrow
band ultraviolet B (NB-UVB) for psoriasis was included. Treatment target was a reduction of 90% from basal PASI
(PASI90), but if patients did not achieve this response after 20 sessions, treatment was continued until PASI75
clearance was achieved. Patients were followed up and relapses were retreated with the same PASI at the first time.
Relation between PASI before treatment and total doses needed to achieve PASI75 or PASI90 was studied.
Results: Among the 242 patients that received NB-UVB for psoriasis, 102 had guttate psoriasis (GP) and 122 had
plaque psoriasis (PP). PASI90 was achieved in 89.1% of patients with GP and 64,8% of patients with PP. Response
was significantly better (p<0.05) in GP patients. Retreated patients affected of PP needed the same doses as the first
treatment received (p>0.005). Patients with higher PASI need more doses to clear up.
Conclusion: Phototherapy with NB-UVB is significantly more effective in patients with GP than patients with PP.
Patients retreated seems to need the same doses. Initial PASI can predict the total doses needed to achieve PASI75 or
PASI90.
Psoriasis; Phototherapy; Narrow band ultraviolet B (NB-UVB); Psoriasis Area and Severity Index (PASI)
Psoriasis is a skin condition that affects approximately 3% of the population 1. There are several forms of psoriasis, the most frequent is plaque psoriasis, representing approximately 90% of all forms, followed by guttate psoriasis, which accounts for approximately 4% of cases. Most cases of psoriasis are mild and respond to topical treatment, however, 17% are moderate or severe forms [1,2].
The American Academy of Dermatology (AAD) Guidelines [3] and European-S3 Guidelines of the European Academy of Dermatology and Venereology (EADV) [4] recommend phototherapy with narrow band ultraviolet B (NB-UVB) as the first-line treatment in psoriasis with more than 5% of the body surface affected (BSA) without respond to topical treatment [5]. According to the latest Cochrane review, NB-UVB is preferred over PUVA because the administration of an oral treatment prior to treatment is not needed and there are fewer long-term carcinogenic effects [6].
The Psoriasis Area and Severity Index (PASI) is the most used and validated tool to measure the severity of psoriasis and was recently shown to be the optimal method for measuring the severity of the psoriasis [7]. The PASI75 is used to describe the patients who achieve 75% reduction of their initial PASI score with a specific treatment and is becoming a standard for comparing treatments. The PASI75 was used in different reviews that compare systemic and biological treatments [8]. However, the introduction of new biological drugs for psoriasis with high efficacy, has increased expectations, and the PASI90 (patients who achieve 90% reduction from original PASI) has emerged as a new standard for measuring the results of treatments [9]. Phototherapy with NB-UVB can achieve a global PASI75 in 62% of patients (CI 95%, 45-79) [9]. However, in guttate psoriasis, the effectiveness of this treatment is higher [10].
Primary objective
To assess the efficacy of phototherapy with NB-UVB in adult patients with psoriasis.
Secondary objectives
To compare the efficacy of NB-UVB according to the clinical form, guttate or plaque psoriasis.
To study the relation between PASI previous to phototherapy and the doses needed to achieve PASI75 or PASI90.
To assess the time of remission after the treatment and the doses needed in case of retreatment.
A prospective, open and observational study was conducted between November 2011 and February 2019. Patients included were adult (>18 years old) treated with NB-UVB with more than a 5% of body surface area (BSA) affected with psoriasis. Age and sex, clinical form (guttate<3 cm or plaques), PASI previous to treatment, number of sessions and the accumulated dose received were collected. Patients were treated according to guidelines [4,5] following the skin phototype protocol. All patients signed informed consent.
A Waldmann® (UV7002, Villingen-Schwenningen, Germany) phototherapy boot with an average emission wavelength of 313 nm was used and three sessions per week were applied. The only concomitant treatment used were emollients. Treatment was applied while improvement continued, with the aim of achieving PASI90. If the patient improved but did not reach PASI90, then PASI75 was set as the objective. The treatment was suspended if after 20 sessions the patient did not improve. Consequently, the response obtained was classified as PASI90, PASI75 or incomplete response (IR).
Patients were followed throughout the study period and advised to visit the clinic if the condition worsened. Those who returned to the initial PASI score previous to the first phototherapy treatment were retreated with the objective of achieving at least the same response as in the first time. The time in remission and the dose received to achieve the same response were recorded.
The statistical analysis was conducted with SPSS® for Windows® 23.0 (IBM®, New York, NY). Descriptive statistics of the sample were obtained. After testing for normality with the Kolmogorov - Smirnov test and homogeneity of variance with the Levene test, we utilized the Wilcoxon test for independent data to compare the descriptive statistics obtained from patients with guttate and plaque psoriasis (median, mode, and interquartile range [IQR]). The Chi square test was used to evaluate differences between the two clinical forms and the PASI75 and PASI90 response; an odd ratio (OR) was used to express the response ratio. Partial correlations between all studied variables were controlled for age, sex and the number of sessions. A linear regression model was used to develop the doseresponse curve for PASI75 or higher depending on the basal PASI. In patients who were retreated after verifying the absence of normality with the Kolmogorov-Smirnov test and homogeneity of variance with the Levene test, we compared the doses received using the Wilcoxon test for paired data. All of the analyses were two-tailed, with a significance level of p<0.05.
A total of 224 patients were recorded (Figure 1 and Table 1). Among the patients with GP, 59 were male (48%) and 53 were female (52%). Among the patients with PP, 58 were male (48%) and 64 female (53%). The average age of patients with GP was 33.6 years (mode 32, median 24, IQR 16), and the mean PASI at the beginning of treatment was 8.3 (mode 8.29, median 8, range 4.85). The patients received an average dose of 14.67 mJ/cm2 (median 12.33, mode 10.10 and IQR 10.91) and underwent an average of 20.1 sessions (median 18.5, mode 20, IQR 13).
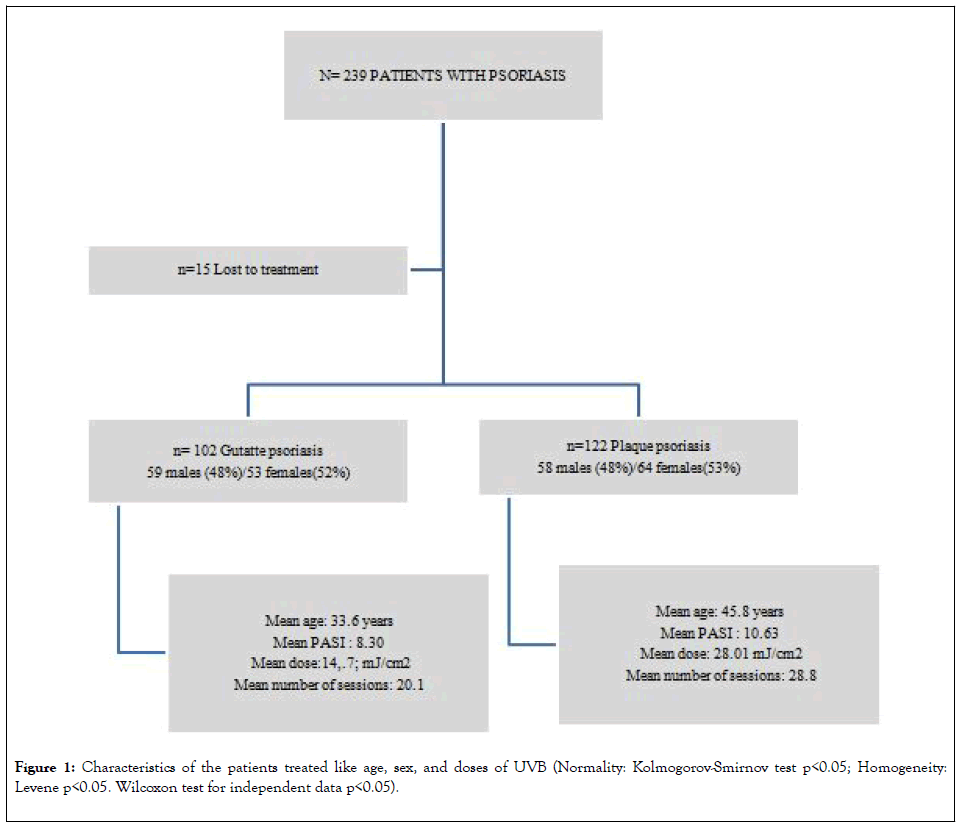
Figure 1: Characteristics of the patients treated like age, sex, and doses of UVB (Normality: Kolmogorov-Smirnov test p<0.05; Homogeneity: Levene p<0.05. Wilcoxon test for independent data p<0.05).
| Guttate psoriasis (N=102) | Plaque psoriasis (N=122) | Chi-square test/OR |
|---|---|---|
| PASI90 89.2% (n=91) | PASI90 64.8% (n=79) | p<0.00; OR 4,50 |
| PASI75 95.1% (n=97) | PASI75 82.7% (n=101) | p<0.05; OR 4,03 |
Table 1: Descriptive data of the study sample.
The patients with PP had an average age of 45.8 years (median 45, mode 45, IQR 21) and a mean PASI at the beginning of treatment of 10.63 (median 9, mode 10, IQR 4). These patients received an average dose of 28.01 mJ/cm2 (median 22, mode 13.40, IQR 16.29) and underwent an average of 28.82 sessions (median 26, mode 20, IQR 13.21). The descriptive data for the sample are summarized in Table 1. The Kolmogorov - Smirnov test (p<0.05) showed an absence of normality in all variables measured in both groups, and the Levene test showed the absence of homogeneity of variance (p<0.05). Therefore, the Wilcoxon test for independent data was used, and significant differences were found in the variables measured in the two groups (p<0.05).
Among the 102 patients with GP, 89.2% (91 patients) achieved PASI90, 5.9% (6 patients) reached PASI75 and 4.9% (5 patients) had an IR (Table 2). Among the 122 patients with PP, 64.8% (a total of 79 out of 122) achieved PASI90, 22.2% (75 patients) achieved PASI75 and 17.2% had an IR (21 patients). Using the Chi-squared test, the proportion of patients who achieved PASI90 was found to be significantly different between the GP and PP groups (p<0.05), with an OR of 4.50. The same comparison was conducted with the patients who reached PASI75, and a significant effect was again observed (p<0.05), with an OR of 4.03.
| Guttate psoriasis, N=102 | Plaque psoriasis, N=122 | |||||||
|---|---|---|---|---|---|---|---|---|
| Age | PASI | Doses | Sessions | Age | PASI | Doses | Sessions | |
| Mean | 33.63 | 8.29 | 14.67 | 20.10 | 45.80 | 10.63 | 28.01 | 28.82 |
| Median | 32.00 | 8.00 | 12.33 | 18.50 | 45.00 | 9.00 | 22.01 | 26.00 |
| Mode | 24.00 | 8.00 | 10.10 | 20.00 | 45.00 | 10.00 | 13.40 | 20 |
| IQR | 16.00 | 4.85 | 10.91 | 13 | 21.00 | 4.00 | 16.29 | 13.25 |
Table 2: Response to treatment with narrow band ultraviolet B (*p<0.05 Wilcoxon test).
In patients with PASI75 and PASI90 responses, partial correlations controlled for age, sex and the number of sessions showed a linear relationship between PASI and the doses for each form of psoriasis and overall. Figure 2 shows the scatterplot of the dependent variable "dose" relative to the variable "PASI" (p<0.000) in patients who reach PASI75 or higher, showing the following linear equation: "DOSE=13.510+0.624* PASI at the beginning of treatment”. The regression analysis for each type of psoriasis showed the following linear relationships: "DOSE guttate: 9.01+0.45* PASI at the beginning of treatment" and "DOSE plaques 10.94+0.46* PASI at the beginning of treatment”.
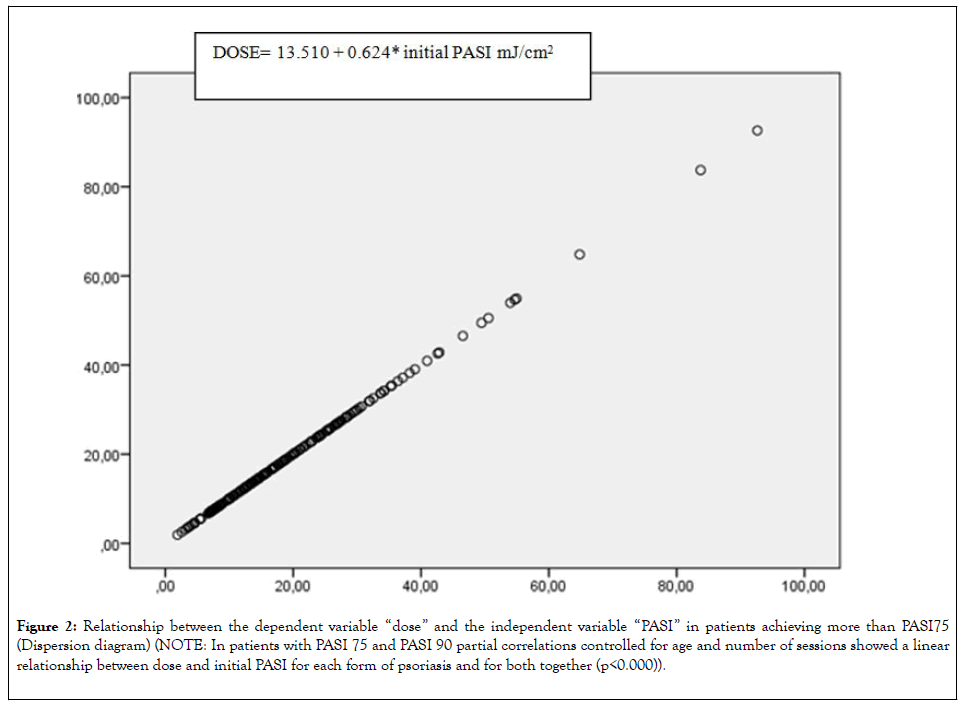
Figure 2: Relationship between the dependent variable “dose” and the independent variable “PASI” in patients achieving more than PASI75 (Dispersion diagram) (NOTE: In patients with PASI 75 and PASI 90 partial correlations controlled for age and number of sessions showed a linear relationship between dose and initial PASI for each form of psoriasis and for both together (p<0.000)).
A total of 38 patients sought treatment for worsening psoriasis during follow up and were considered candidates for retreatment; all of these patients had PP. The Kolmogorov- Smirnov test (p<0.05) showed an absence of normality in all variables measured in both groups, and the Levene test showed the absence of homogeneity of variance (p<0.05) (Figure 3). In this group of patients, the average dose and number of sessions in the first treatment were 23.15 mJ/cm2 (median 17.77, mode 12.24, IQR 16.20) and 26.18 (median 22.00, mode 20.00, IQR 12.25), respectively. The average remission time until returning for retreatment was 14.47 months (median 12.00, mode 12.00, IQR 6). In the second treatment, the patients received an average dose of 21.95 mJ/cm2 (median 16.73, mode 12.24, IQR 17.16) and an average of 24.10 sessions (median 22, mode 15, IQR 16.76). The Wilcoxon test for paired data showed no statistically significant differences with respect to dose and session number between the first and second treatments (p>0.05) (Figure 4).
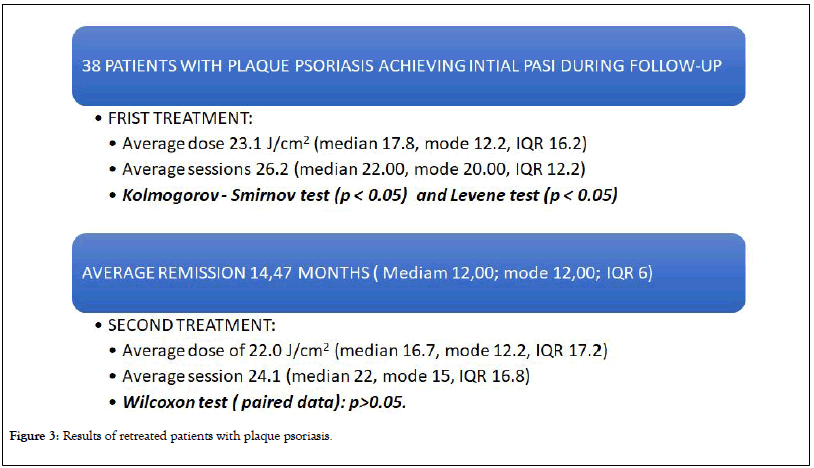
Figure 3: Results of retreated patients with plaque psoriasis.
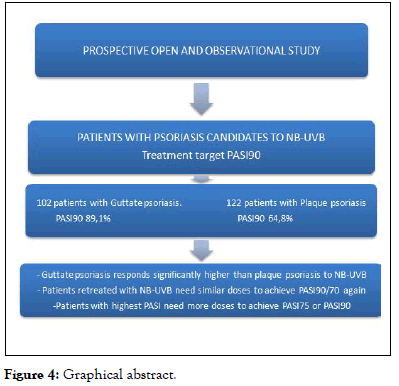
Figure 4: Graphical abstract.
Phototherapy with NB-UVB is considered a first-line treatment in psoriasis with BSA greater than 5% [3-5]. The PASI is the most studied and validated tool to measure the severity of psoriasis. PASI75, a reduction in the prior PASI of 75%, is the standard objective for effectiveness in most studies [4,8]. However, with the introduction of biological drugs with high efficacy, PASI90 has also been established as a measure of effectiveness [9].
Patients in the present study were divided according to their clinical form, GP or PP, using 3 cm as the size limit for plaques, which is similar to other studies 10. This separation of groups was performed because GP has a better prognosis, usually affects younger people and usually responds better to phototherapy [10,11]. Some studies reviewed did not specify the type of psoriasis when evaluating effectiveness; therefore, the reader assumes plaques, but the inclusion of GP with PP improves the results because GP shows better responses [12-14].
The treatment protocol used for patients was based on skin phototype, according to the guidelines of the American Academy of Dermatology [3] and the European Academy of Dermatology and Venereology [4]. Some authors use the manufacturer's protocol, which is a slightly lower dose, which may explain why 30 to 50 sessions may be needed 11 versus 18-24 sessions in most studies [5]. The patients received concomitant treatment with emollients, which have been shown to increase the penetration of ultraviolet radiation B5.
In addition to the classic objective of PASI75, this study includes PASI90. To our knowledge, there are only two recent studies published assessing the efficacy of phototherapy in psoriasis with the PASI90 metric [4].
Twenty sessions were arbitrarily set as the limit for suspending the treatment if the patient did not improve, but the consulted guidelines do not contain any recommendation in this issue. The PASI90 was attempted in all patients, but when patients stopped improving, PASI75 was set as the target. This treatment protocol was used in the study design and follows our usual practice. Nevertheless, there is a loss of information in patients who exceeded PASI75 but did not reach PASI90 when the data were analysed. The measurement of the basal and final PASI of all patients would have avoid this limitation in the study.
Furthermore, in our group of patients, some remained at a very low global PASI, corresponding to PASI75, and yet showed a good response.
Patients with relapses to at least the previous PASI were identified as candidates for retreatment with the aim of achieve the same result as the first time. This design was selected to compare the doses received in the first and second treatment. In our practice, patients treated previosly, were familiar with the treatment and often returned to the clinic.
The described variables were not normally distributed, based on the Kolmogorov-Smirnov and Levene tests, and tended to a more common repeated value (mode). Thus, the variables were described as not described as the mean, mode, median and interquartile range (IQR). For the same reason, the statistical test used was the Wilcoxon test for paired data in the case of retreatment assessment. To calculate the regression line between PASI75/PASI90 and doses, partial correlations to control the variables sex, age and the number of sessions were applied.
Nearly all patients (95.1%) with GP and 82.8% of patients with PP reached PASI75 or higher (Figure 2). These percentages are higher than those published in the literature reviewed 8 but are close to the two most recently published studies. In 2010, Dayal [15] treated 30 patients with PP, and 100% of patients reached PASI75 or higher. In 2011, Chauhan [16] treated 21 patients and found the same response in 81% in patients with high PASIs (approximately 16). In our group of patients, the PASIs were 8.3 in the GP and 10.6 in the PP. Interestingly, the studies of Dayal [15] and Chahuan [16] used, as in our study the treatment protocol guided by skin phototype (three sessions per week with 20% increases in dose in each session). Most of the previously described studies with less efficacy protocols were based on 70% of the minimal erythemal dose (MED) [8] and further studies are necessary to confirm this fact.
In both forms of psoriasis, women slightly predominated in our study, although this difference was not significant. The rest of the variables (Table 1) were not distributed equally across both groups (Wilcoxon, p<0.05). Specifically, patients with GP were younger, had lower initial PASI and required a lower dose to achieve a better response. The probability of achieve PASI75 with a GP on our patients, compared to PP, was 4 times higher. For PASI90, the chance was 4.5-fold higher.
The "cost-PASI", in relation to doses used, was calculated for phototherapy with NB-UVB (Figure 3). This analysis showed a linear relationship for both forms of psoriasis and when the initial PASI was more severe, in our patients, more doses were required for clearance. This finding provides guidance to calculate the time and/or the number of doses required when scheduling treatment. The global formula in our patients was “Total dose=13.510+0.624* initial PASI”.
A total of 38 patients, all with PP, need to be retreated in an average time of 14.47 months (mode 12 months, IQR 6). To our knowledge, this study found for the first time that patients needed the same dose (p>0.005) to obtain the same response for the same initial PASI. This result could implies that each patient requires a specific total dose. Previous studies have found relapse rates at 12 months of approximately 30% [17]. The evidences if the relapses are more frequent in GP or in PP are not clear [10,18]. Relapses seem to be related to the initial PASI [19]. Guidelines suggest [3,4] maintenance protocols, with a gradual reduction of sessions over 4-6 weeks after response, to increase the time of the response to phototherapy. We did not assess this particular question and patients stop treatment when response was obtained.
Phototherapy with NB-UVB in adult psoriasis is a high effective treatment for psoriasis achieving more than PASI75 in 80% of our patients treated. Patients with GP showed a significant better response to NB-UVB than patients with plaque psoriasis. Patients with highest initial PASIs need more doses for clearance and relapses tend to need the same doses.
Citation: Fernández-Guarino M, Aboin González S, Gonzalez-Cantero A, Arsuaga C, Lázaro P (2020) Phototherapy with Narrow-Band Ultraviolet B in Adult Psoriasis: A Study in Clinical Practice. J Clin Exp Dermatol Res. 11:521. DOI: 10.35248/2155-9554.20.11.521
Received: 04-May-2020 Accepted: 18-May-2020 Published: 25-May-2020 , DOI: 10.35248/2155-9554.20.11.521
Copyright: ©2020 Fernández-Guarino M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.