International Journal of Physical Medicine & Rehabilitation
Open Access
ISSN: 2329-9096
ISSN: 2329-9096
Research Article - (2023)Volume 11, Issue 4
Background: Schizophrenia has disabling effects over mental and physical integrity involving changes in posture and flexibility, which reduce mobility, autonomy, and quality of life. Physical activity has been tested with uncertain effects in schizophrenia, mostly due to trial design, methodology, comparison groups, intervention length, and attrition. Inconsistency led to poor dissemination of active interventions in this population, which may benefit these individuals’ health.
Objective: To evaluate the response of two different protocols: Aerobic and Functional exercises, in two groups of sedentary adult-patients with the diagnosis of schizophrenia and healthy controls.
Methods: A clinical trial of two standardized physical interventions in adults diagnosed with schizophrenia and healthy controls. Posture was assessed by digital photogrammetry with the aid of a software and the flexibility by the Wells Fargo’s Test.
Results: A total of 38 individuals completed the intervention, with 24 in Aerobic group and 14 in Functional group. The groups were homogeneous for gender, weight, and body mass index, with small differences in age and height. Posture and Flexibility changed according to group and intervention. In this study, guided physical activity improved posture and flexibility in both groups, with higher effect of the Functional protocol than the Aerobic protocol in cases and controls.
Conclusions: Despite a preliminary and relatively small sample size, the study evidences the feasibility and clinical utility of physical intervention in schizophrenia. Additional data about specific adaptations in schizophrenia are needed to improve outcomes, such as individualized assistance, support, instructions and intensity.
Schizophrenia; posture; flexibility; physical activity; sedentary lifestyle
AI: Aerobic Intervention; BMI: Body Mass Index; CAPS: Psychosocial Attention Center; DSM: Diagnostic and Statistical Manual of Mental Disorders; FI: Functional Intervention; FHT: Degree Of Forward Head Tilt, Lateral View; GLM: Generalized Linear Model; HATT: Degree Of Horizontal Alignment of The Tibial Tubercle; HCPA: Hospital de Clínicas de Porto Alegre; HPA: Degree Of Horizontal Pelvic Alignment, Lateral View; HPM: Degree of Horizontal Pelvic Tilt; IBGE: Brazilian Institute of Geography and Statistics; KA-LV: Knee Angle, Lateral View; LHT: Degree of Lateral Head Tilt; LTT: Degree of Lateral Trunk Tilt; PRODESQ: Psychiatry Outpatient Clinic of Schizophrenia and Dementia; ReBEC: Brazilian Registry of Clinical Trials; SA: Degree of Horizontal Scapular Asymmetry Toward The Third Thoracic Vertebra; SAPO: Postural Assessment Software; SD: Standard Deviation; SM: Degree of Shoulder Misalignment; SCZ: Schizophrenia; VTA: Degree of Vertical Trunk Alignment, Lateral View; VV-LF: Degree of Varus or Valgus Alignment, Left Foot; VV-LLL: Degree of Varus or Valgus Alignment, Left Lower Limb; VV-RF: Degree of Varus or Valgus Alignment, Right Foot; VV-RLL: Degree of Varus or Valgus Alignment, Right Lower Limb; WB: Well’s Bank
Schizophrenia (SCZ) is classified as a serious mental disorder with disabling symptoms such as visual or auditory hallucinations, loss of emotional and social interaction, and aggressiveness, with accentuated cognitive and emotional impairment that bring social stigma, dependency, and incapacity [1,2]. Usual treatment with antipsychotics is associated with adverse effects such as obesity, metabolic syndrome, and extrapyramidal symptoms, with limited potency over symptoms [3]. The combination of adverse effects and physical inactivity progressively increases due to muscle stiffness, rigidity, and pain [4].
Posture and Flexibility are strongly affected. Posture is defined by the position of the body in the environment in which it is placed and is changed in major mental illnesses (depression, anxiety, and schizophrenia) [4-8]. Flexibility interacts with the posture and is changed by the use of antipsychotic medications that interfere with the musculature and weight [3,4].
On the other hand, guided physical activity has been essential to treat mental disorders, such as depression, anxiety, and schizophrenia [9-12]. The preferred protocol of physical activity works at a submaximal level, from 65-80% of the total capacity, to correctly stimulate the oxidative process (aerobics). On the other hand, postural exercise is based on body consciousness and motor control. One unanswered question is if flexibility and posture deficits are consequences of physical inactivity and sedentary lifestyle, part of the natural course of the disease, or consequence of medication. Additional knowledge is needed about positive effects of different types of physical activity.
Based on previous data about postural changes in schizophrenia, such as head anteriorization, scoliosis, pelvic anteversion, and flexibility deficits [4], this study assessed the effects of two physical exercise protocols over the posture and flexibility of individuals with schizophrenia compared to people without major mental illness, but with similar sedentary lifestyles.
This is a clinical trial of physical intervention (aerobic physical intervention [AI] and functional physical intervention [FI]) in two groups of stable outpatients with diagnosis of SCZ. The AI group received regular care at a public health facility (Psychosocial Attention Center [CAPS]) in a mid-sized municipality of Southern Brazil. FI group received regular care at a public health facility (Psychiatry outpatient clinic of schizophrenia and dementia [PRODESQ] in the Hospital de Clínicas de Porto Alegre [HCPA]), in the capital of the state of Rio Grande do Sul, in the Southern Brazil.
Patients were compared with a control group paired by gender, age, and social class (following classification of the Brazilian Institute of Geography and Statistics), and allocated into two different protocols (AI and FI).
Participants
Stable outpatients under regular treatment in two different health care services: AI group at the Psychosocial Clinic-CAPS, in Camaquã and FI group in Outpatient PRODESQ at the HCPA in Porto Alegre. All individuals received a psychiatric diagnosis after a three-step procedure: (1) clinical interview and observation over at least three evaluations; (2) family interview; and (3) medical record review by a trained psychiatrist. Inclusion criteria were: a) Diagnostic and Statistical Manual of Mental Disorders (DSM-5) (American Psychiatric Association 2013) diagnosis of SCZ; b) individuals aged 18-65 years; c) the patients were under stable drug treatment adjusted to their clinical state for at least three months; and d) no involvement in other physical activity programs during the intervention. Exclusion criteria were: a) alcohol or other drug abuse in the last month; b) major systemic or neurological diseases; c) physical disability contraindicating physical activity; d) risk of suicide confirmed by direct contact with the patient and family; e) pregnancy or women of reproductive age not using a contraception method; and f) patients who did not agree to participate in the study after full explanation of the program.
Control group was recruited with the aid of specific social networks paired by gender, age (3 years older or younger); social class. Absence of any major mental illness was defined by enrollment interview directly questioning experiences of memory loss, psychosis (delusions and/or hallucinations), depression, mania, generalized anxiety disorder, or obsessive–compulsive disorder. Exclusion criteria were the same as those applied for patients with SCZ.
Clinical assessment
After recruiting patients and controls, the subjects were clinically and physically evaluated by a group of trained professionals. This evaluation was conducted before the intervention and three months after the treatment.
Postural analysis
The postural evaluation was performed by a postural photogrammetry and the protocol that was applied was previously described in patients with schizophrenia [1]. To take the pictures in three different plans (anterior, posterior, and right side), the individuals were marked with extended polystyrene foam balls (3 cm diameter) attached to the skin with double sided tape. The anatomical points marked were: tragus, acromion, anterior superior iliac spine, greater trochanter of the femur, joint line of the knee, medial aspect of the patella, tibial tubercle, lateral malleolus, medial malleolus, midpoint between the heads of the second and third metatarsals, spinous process of C7, spinous process of T3, interior angle of the scapula, posterior superior iliac spines, midline of calf, point over the calcaneal tendon at the mid-height level of the malleolus, and calcaneus. The same evaluator made all markings.
A postural evaluation software (SAPO 0.67) was used for the analysis and interpretation of the images [13]. In total, 14 postural angles were described and evaluated by it: LHT (Lateral Head Tilt), FHT (Front Head Tilt, Lateral View), SM (Shoulder Misalignment), HPM (Horizontal Pelvic Misalignment), LTT (Lateral Trunk Tilt), SA (Scapular Asymmetry), VTA (Vertical Trunk Alignment, Lateral View), HPA (Horizontal Pelvic Alignment, Lateral View), VV-RLL (Varus, Valgus Right Lower Limb), VV-LLL (Varus, Valgus Left Lower Limb), HATT(Horizontal Alignment Tibial Tubercle), VV-RF (Varus, Valgus Right Foot), VV-LF (varus, Valgus Left Foot), KA-LV (Knee Angle, Lateral View). Previous protocols described in the literature were followed to interpret these angles, in which the positive angles are counterclockwise, thus, showing that the left side is higher than the right side and the reference value for all angles is zero [4,13]. The measures were expressed in degrees or percentages, according to what was appropriate for each variable.
Stretching: well’s bank (WB)
Wells sit and reach tests are easy to apply and to reproduce. It evaluates the upper chain flexibility of lower limbs, which is composed by muscles (hamstring and triceps surae) and fascias, and it also receives the interference of the spine. To perform the test, the individual must sit on the floor or on a mat with the legs totally outstretched and the feet flat against the front of the test box, leaning against the bench (specially developed for this test), leaning forward, keeping knees straight, sliding the hands as far as the participant can reach. The results are recorded in cm, repeating three times [14].
Physical interventions
The patients and controls were subjected to two types of interventions: aerobic and functional (Figures 1 and 2). Both interventions lasted one hour and happened twice a week for 12 weeks.
Figure 1: Aerobic physical intervention.
Figure 2: Functional physical intervention.
Aerobic interventions
5-minute warm-up of comfortable intensity, 45-minute aerobic exercise of increasing intensity using any of the 3 modalities: a stationary bicycle (Embreex 367C, Brazil), a treadmill (Embreex 566BX, Brazil), or an elliptical trainer (Embreex 219, Brazil), 10-minute global stretching of large muscle groups shown in Figure 1.
Functional interventions
(a) 5-minute warm-up with stationary walk; (b) 15-minute muscle and joint mobility exercises; (c) 25-minuteglobal muscle resistance exercises (paravertebrals, abs, extenders, flexors, adductors, hip adductors, shoulders, knees and elbows flexors and extenders); (d) 15-minute breathing body awareness work shown in Figure 2.
Both cases and controls needed 80% frequency to avoid exclusion from the study. The patients kept receiving regular clinical treatment besides a standardized physical intervention. Most individuals from both genders had never practiced any physical exercise. Therefore, the participants had to adapt to the first appointments. The participants who performed the aerobic intervention were monitored by a heart rate digital monitor that should go up to 70-80% of the maximum heart rate calculated by the Karvonem equation [15]. These individuals were followed by a professional all the time, with guidances, adjustment of equipments and encouragement. On the other hand, the participants who performed the functional intervention were divided in trios and quartets to perform the exercises. For each exercise, three sets of 10 to 15 reps were performed, according to the individuals’ endurance. Balls, dumbbells, and elastic bands were used and were evaluated by a professional, according to the individuals’ progress and their preferences.
Statistical analysis
Kolmogorov-Smirnov test was used to evaluate the normality of data distribution. Quantitative variables with a normal distribution were presented as means and standard deviations, whereas variables with an asymmetric distribution were presented as medians and interquartile ranges. Student’s paired t-test/independent t-test or the Wilcoxon test/Mann-Whitney test were used to compare normal and asymmetric variables, respectively. Three or more groups were compared by the analysis of variance (ANOVA) test followed by Bonferroni correction. Categorical variables were presented as frequencies and analyzed using the Pearson’s chi-square test or the Fisher’s exact test. The major outcome measure was assessed using the Generalized Linear Model (GLM) analysis (gamma distribution) and confounding factors were determined based on statistical criteria (association with the study factor and the outcome with a p significance level ≤ 0.2). The significance level was p ≤ 0.05. The analysis of effect size was used to evaluate the magnitude of the difference derived from GLM. The data were processed and analyzed in SPSS Statistics 22.0.
Table 1 shows the socio-demographic and clinical data. Out of 43 individuals with SCZ in the study, five were excluded due to insufficient frequency; out of 49 controls, 11 were excluded for the same reason.
| Characteristic/Group | Cases | Controls | p-value |
|---|---|---|---|
| Gender n (%) | - | ||
| Men | 32 (84.2) | 32 (84.2) | - |
| Women | 6 (15.8) | 6 (15.8) | |
| Schooling n (%) | - | ||
| Basic education | 38 (100) | 27 (71.1) | - |
| Higher education | - | 11 (28.9) | - |
| Marital status (%) | - | ||
| Single | 37 (97.4) | 11 (28.9) | - |
| Married | 1 (2.6) | 27 (71.1) | |
| Smoking n (%) | - | ||
| Yes | 14 (36.8) | - | - |
| No | 24 (63.2) | 38 (100) | - |
| Years of illness n (%) | - | ||
| <7 years | 4 (10.5) | - | - |
| >7 years | 34 (89.5) | - | - |
| Antipsychotic medication n (%) | |||
| Typical antipsychotic | 13 (34.2) | - | - |
| Atypical antipsychotic | 17 (44.7) | - | - |
| Combination of typical and atypical | 8 (21.1) | - | - |
| Age (years, mean ± SD) | 40.95 ± 11.37 | 41.68 ± 11.22 | 0.039* |
| Weight (Kg, mean ± SD) | 83.77 ± 23.56 | 88.66 ± 18.51 | 0.274 |
| Height (m, mean ± SD) | 1.69 ± 0.080 | 1.73 ± 0.070 | 0.011* |
| BMI (mean ± SD) | 29.23 ± 7.96 | 29.55 ± 5.88 | 0.829 |
| Median of psychiatric hospitalizations (p25-p75) | 2.00 (0.75-4.00) | - | - |
Note: BMI=body mass index; SD=Standard Deviation; *p ≤ 0.05.
Table 1: Baseline sample characteristics.
The final sample comprised 38 subjects in two groups: AI (N=24) and FI (N=14). The groups were homogeneous for gender, weight, and body mass index (BMI), with statistical difference in age and height.
Table 2 shows postural data from AI and FI from cases and controls pre and post intervention.
| Patients (mean ± SD) | Controls (mean ± SD) | |||||||
|---|---|---|---|---|---|---|---|---|
| Intervention | Aerobic (n=24) | Functional (n=14) | Aerobic (n=24) | Functional (n=14) | ||||
| Time | Before | After | Before | After | Before | After | Before | After |
| Characteristic | ||||||||
| SM | 2.00 ±1.33 | 3.14 ±2.15 µ | 3.17 ±2.21 | 2.09 ±1.81 π | 2.62 ±2.57 | 2.97 ±2.24 πµ | 2.19 ± 1.51 | 1.72 ±0.93π |
| HPM | 2.33 ±1.75 | 4.15 ±3.52 πµ | 2.81 ±2.40 | 2.57 ±2.73 µ | 2.99 ±1.57 | 1.68 ±1.96 Ωπµ | 1.77 ±1.29 | 1.00 ±0.65Ωπµ |
| LTT | 2.78 ±1.75 | 3.33 ±2.99 | 4.02 ±2.74 | 2.44 ±2.43 π | 3.20 ±2.13 | 2.63 ±2.19 Ω | 2.98 ±2.25 | 1.85 ±1.62Ωπ |
| VV-LLL | 3.63 ±2.47 | 4.43 ±2.94 | 3.41 ±2.35 | 2.95 ±2.74 | 4.30 ±3.12 | 4.04 ±2.82 π | 3.98 ±3.34 | 3.77 ±3.51 |
| LHT | 2.57 ±1.82 | 4.00 ±3.16 π | 4.48 ±4.89 | 3.52 ±3.12 | 3.05 ±2.76 | 2.76 ±3.07 | 3.00 ±1.84 | 4.26 ±4.61 |
| HATT | 3.29 ±3.87 | 3.44 ±3.25 | 4.36 ±3.38 β | 3.87 ±3.21 | 2.44 ±2.16 | 2.80 ±2.02 | 2.37 ±1.98 β | 1.86 ±2.86 |
| SA | 16.66 ±15.74 | 20.38 ±18.73 ∑ | 20.56± 16.13 | 21.17 ±14.71 ∑ | 16.64± 12.50 | 11.82 ±10.98 ∑ | 18.75± 15.07 | 22.07 ±13.97∑ |
| VV-LF | 8.83 ±5.60 | 9.59 ±5.85 µ | 6.86 ±7.01 | 4.91 ±4.84 πµ | 6.01 ±4.80 | 8.29 ±5.54 µ | 9.55 ±6.54 | 7.70 ±6.28πµ |
| FHT | 26.18±18.83 α | 27.94 ±17.36 πµ | 25.78±16.64 α | 23.09 ±17.02 πµ | 15.77±9.80 α | 12.00 ±8.34 Ωµ | 14.63±7.65 α | 12.46 ± 9.82Ωπµ |
| VTA | 3.21 ±4.89 | 5.52 ±4.27 ∑ | 5.24 ±3.93 | 4.81 ±4.29 | 4.04 ±2.90 | 3.18 ±2.84 ∑ | 4.16 ±2.71 | 3.26 ±2.07 |
| HPA | 14.45± 9.40 α | 14.42 ±8.48 | 14.74± 7.38 α | 14.66 ±7.75 µ∑ | 17.73±6.36 α | 13.92 ±5.28 Ωπµ | 10.62±3.55 α | 9.01 ±4.25Ωµ |
| KA-LV | 8.32 ±5.54 | 6.08 ±4.98 Ω | 12.75± 20.96 | 8.81 ±13.77 Ω | 4.70 ±2.98 | 4.86 ±3.58 | 3.84 ±2.81 | 4.11 ±2.76 |
| VV-RL | 4.25 ±3.32 | 4.10 ±2.98 | 3.19 ±3.18 | 2.96 ±2.92 | 3.83 ±243 | 3.29 ±2.42 | 4.09 ±3.40 | 3.93 ±3.76 |
| VV-RF | 8.39 ±5.04 | 6.13 ±4.65 | 7.46 ±6.57 | 8.63 ±5.89 | 6.58 ±5.83 | 7.90 ±6.65 | 8.01 ±5.09 | 6.47 ±5.29 |
Note: SD=Standard Deviation; α p ≤ 0.05 intergroup before intervention; β p ≤ 0.05 intragroup before intervention; π p ≤ 0.05 intergroup before X after; Ω p ≤ 0.05 intragroup before X after; µ p ≤ 0.05 intergroup after; ∑ p ≤ 0.05 intragroup after.
Table 2: Measurements of postural angles, according to the intervention.
Figure 3 shows 12 statistical differences out of the 14 angles evaluated. We observed that the groups were homogeneous in the first moment and showed differences in only three angles (HPA, HATT, and FHT). The results were better for the control group post intervention, which show that even people with a sedentary lifestyle evolved in contrast with the cases. On the other hand, the difference between the interventions is clear when comparing the initial moment with the ending moment, in which people who performed the functional protocol (both cases and controls) improved in a higher number of angulations. Thus, the cases who performed the aerobic protocol had worsened in the posture changes.
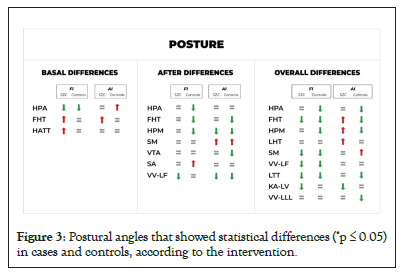
Figure 3: Postural angles that showed statistical differences (*p ≤ 0.05) in cases and controls, according to the intervention.
Figure 4 shows changes in flexibility, with relevant changes in those receiving FI (p=0.003) and higher changes in controls (mean change of 3 points) compared to cases (mean change of 1.93 points).
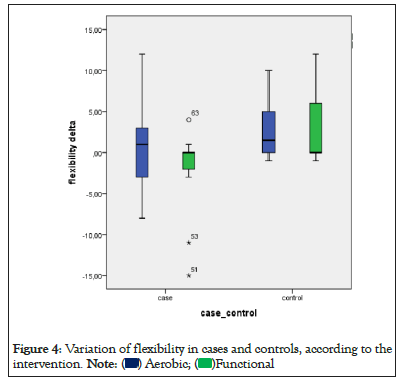
Figure 4: Variation of flexibility in cases and controls, according to the
intervention. 
Guided physical activity induced significant changes in both groups. The type of protocol significantly affected the posture and flexibility, suggesting that FI had better results than AI. The groups were firstly homogeneous in most variables, being the group case with a major gravity in the three posture angles (HATT, HPA, and FHT) and in the flexibility. When we put these individuals under two different types of intervention, the results showed that the functional protocol was superior to the aerobics in the improvement in many posture angles and in the flexibility, both in cases and controls. The studies that suggest the practice of physical activities for this population are mostly aerobic exercises, which makes our findings relevant, since we suggest that more complex exercises and in groups, such as functional training, might be more efficient and able to benefit more of this population. The AI worsened the posture change in the cases in some angles, which raises a major concern and doubts. What could be generating this worsening in some posture changes? Could it be the type of exercise or the way the practice is oriented? More studies are necessary to answer this question.
In the final moments, the controls presented better results regardless of the protocol, even if having a sedentary lifestyle, and the answers in their bodies were totally different from the cases. This emphasizes the deleterious physical effects of schizophrenia.
Regarding flexibility, similar to the posture angles, the group case presented a major gravity in the beginning, and those who performed the functional protocol significantly improved, regardless of the group they were in.
A better flexibility interferes in the posture angles because it allows a major extent of movement and mobility, helping in the performance of the exercises and decreasing possible restrictions, thus, creating a better posture [14]. There are no previous studies on flexibility in SCZ, which makes this study more relevant.
Since posture is the position the individual assumes in an environment and is influenced by it, the posture is, therefore, related to psychobiological mechanisms [4,5]. Although posture has been already observed in depression and SCZ, our study is the first to propose specific intervention to improve posture control [6-8].
Since chronic SCZ has a high level of sedentarism and associated features (obesity, muscle atrophy, and physical shortening), we selected controls by similar levels of sedentarism to control the changes from a sedentary lifestyle. Cases had poorer posture before participating in the program, which improved their posture, but only FI had statistically significant changes [16]. We expected the difference among AI if these changes were not only due to a sedentary lifestyle. Subjects who received AI had to stay alone in the treadmill, stationary bike, or elliptical with the evaluator watching them closely without interacting to avoid distractions and accidents [17]. The individuals with FI had strong interaction, with about four subjects interacting with the tutor, who always guided them during the exercises. This difference of behavior possibly reflected in the outcomes, favoring the individuals who received FI [18].
This study's limitations were the lack of randomization, small sample size, and high degree of chronicity. Future studies should control nutritional status and chronic diseases in the control group.
The study evidenced the effectiveness of guided physical activity in patients with severe mental disorders, such as SCZ, which improved posture and flexibility. Posture induced more changes than aerobic intervention. Although preliminary, the results had clinical relevance and can help additional studies.
Ethics approval and consent to participate
The study was registered in the Brazilian Research Registry under No. 43408615.7.0000.5327, registered in the Brazilian Registry of Clinical Trials (ReBEC) under No. RBR-2h2hjy and approved (150066) by the Research Ethics Committee of the Hospital de Clínicas de Porto Alegre (HCPA). Patients and their legal guardians provided written informed consent form after reading and understanding the intervention program and their rights.
Not applicable.
The datasets used and/or analyzed during our study are available from the corresponding author on reasonable request.
The authors state that this study is part of the results from the doctorate degree dissertation of the authors VBC and MFS.
This study was partially financed by the Coordination for the Improvement of Higher Education Personnel-Brazil (CAPES, number 88887.653567/2021-00) and data collection and processing was supported by the Research Incentive Fund (FIPE) - HCPA (number 150066).
VBC and MFS evaluated the cases and controls and supervised the application of the interventions. VBC and PBA were the main contributors in the manuscript elaboration. All authors read and approved the final manuscript.
We thank all patients who participated in the research, and CAPES and FIPE-HCPA for their financial support.
Citation: Cristiano VB, Szortyka MF, Belmonte-de-Abreu P (2023) Physical Therapy Interventions in Schizophrenia Compared to Normal Sedentary Adults: Different Effects of Aerobic and Functional Programs over Posture and Flexibility-Controlled Trial. Int J Phys Med Rehabil. 11:669.
Received: 31-Mar-2023, Manuscript No. JPMR-23-22730; Editor assigned: 04-Apr-2023, Pre QC No. JPMR-23-22730 (PQ); Reviewed: 18-Apr-2023, QC No. JPMR-23-22730; Revised: 25-Apr-2023, Manuscript No. JPMR-23-22730 (R); Published: 02-May-2023 , DOI: 10.35248/2329-9096.23.11.669
Copyright: © 2023 Cristiano VB, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.