Journal of Sleep Disorders & Therapy
Open Access
ISSN: 2167-0277
ISSN: 2167-0277
Research Article - (2024)Volume 13, Issue 8
Sleep is important for a variety of conditions treated by Physiotherapists (PTs), who have an imperative role on wellness and health promoting, mobility, and functional independence; yet sleep education is not included in most physiotherapy programs curricula. The purpose of this study was to evaluate the knowledge, attitudes, and perceptions of Brazilian PTs about sleep, sleep education, and their assessment and education of patients about sleep. This cross-sectional study electronically surveyed 224 licensed PTs practicing in Brazil. Descriptive analyses and logistic regressions were conducted. Of the 224 respondents: 98.9% agreed that sleep is important for overall health; 97.8% agreed that sleep disorders may contribute to medical problems; 94.5% agreed that addressing sleep issues may impact on rehabilitation outcomes; 79.4% did not receive education about sleep during entry-level physiotherapy education; 35.6% received education about sleep in continuing education and during advanced degree programs. Patients aged between 40-59 years-old had less chance of having their sleep habits or quality of sleep assessed, and those aged between 15-18 years and 40-59 years had less chances of being educated about the importance of sleep. Younger PTs had increased chance of routinely educating their patients about the importance of sleep. Brazilian PTs acknowledged that sleep impacts rehabilitation and is important for their patients, which requires sleep education. Therefore, entry-level PT education programs should consider incorporating education about sleep in curricula, as the development of continuing education courses in Brazil are urgently needed.
Sleep; Physiotherapy; Rehabilitation; Education; Sleep knowledge; Health promotion
Sleep is an interdisciplinary field in health sciences and promotion. As we face new challenges throughout the world (i.e., global aging population, pandemics, new technologies, ceaseless societies, and the alarming increase of Non-Communicable Diseases (NCDs), clinical competencies in contemporary health care practice demand updates and new points of view. As knowledge advances, new disciplines such as sleep are now shared between fields of neurology, psychiatry, pneumology, orthopedics, etc., all endeavoring to implement sleep education into clinical practice [1]. This paradigm shifting movement is also occurring within the physiotherapy field.
Physiotherapy plays an imperative role in promoting independence, mobility, health, and well-being in many conditions and diseases across the life span. Most (if not all) of these conditions require sleep as part of the rehabilitation process. Not meeting the sleep quality and quantity requirements (sleep disorders and disturbances) for specific age-ranges, increases the risk of NCDs [2]. Therefore, the term “sleep physiotherapy” has been recently coined by Physiotherapists (PTs) seeking to help their patients’ sleep behavior as part of their physical rehabilitation.
PTs are encouraged to promote healthy behaviors [3-8]. Yet, only a few studies relate sleep into physiotherapy practice [9]. Knowledge about sleep interdisciplinary, skills to screen sleep disturbances, promotion of sleep quality and physiotherapeutic treatment of sleep disorders are important components for PTs to promote health and well-being in their patients and in their clinical practice. Several studies have demonstrated the fundamentals and competencies of PTs in the contemporary world directing practices, bringing evidence and new avenue for future research in the sleep area [10-18]. However, in many countries, the basic curricula of physiotherapy undergraduate courses does not include coursework on sleep medicine.
Perceptions and attitudes of PTs in relation to sleep were investigated in only 3 prior studies, all of which pointed to the same direction: Addressing sleep issues may impact physiotherapy and rehabilitation outcomes. Furthermore, those studies agreed that many conditions treated by the PTs occurred along with sleep disturbances; yet, PTs required adequate tools and education to assess and intervene suitably [11-14]. These studies clearly demonstrated the need to include sleep in the entry school physiotherapy curricula.
Physiotherapy as a profession has shifted from a biomedical approach towards a biopsychosocial approach, leaving PTs in a strategic position to address sleep health [2]. The frequent contact with patients-weekly, or even daily-creates opportunities for PTs to triage patients, educate and advocate for sleep health, and alert other healthcare team members.
Addressing sleep health is particularly important in the Brazilian health context, as sleep disorders are highly prevalent in this country. In São Paulo (the most populous city of the Western and Southern hemispheres), the prevalence’s of objectively evaluated sleep diseases has been found as: 33% of people suffering from obstructive sleep apnea, 32% of insomnia, 7.4% of sleep bruxism, and 3% of upper airway syndrome [19-22]. As far as sleep disorders subjectively measured: 42% people suffered from snoring complaints, 39% of excessive daytime sleepiness, 15% of cataplectic-like symptoms, 15% of sleep paralysis, 9% of hypnagogic/hypnopompic hallucinations, and 7.5% of Restless Legs Syndrome (RLS) in São Paulo city, and 6% of RLS in a rural town [23-26]. Therefore, this investigation aimed to assess Brazilian PTs sleep knowledge and attitudes regarding sleep.
Study design and ethics
This cross-sectional study involved electronically surveying PTs practicing in Brazil. The survey was voluntary and anonymous. This study followed CHERRIES checklist [27]. The Ethics Research Committee of Federal University of São Paulo (UNIFESP, #4.017.766, CAAE #30482519.4.0000.5505, May/2020) and International Review Board of Kansas University Medical Center (KUMC, STUDY00145910) approved this study. Electronic informed consent was obtained from each participant prior to study participation. No identifying information was collected.
Sample
The convenience sample was composed of licensed PTs working in Brazil, using snowball sampling technique.
Survey instrument
The survey was originally developed by Siengsukon et al., from the KUMC [13]. The survey was translated into Brazilian Portuguese by 2 Portuguese native speakers and applied to 10 health professionals for pilot testing to ensure accuracy of meanings, adaptation to cultural terms and validity. After testing, minor terms were adjusted.
A 5-part structured survey with multiple-choice test questions assessed PTs knowledge and attitudes regarding sleep, which included: 1) 8 demographic questions such as Gender, age, degree, years since graduation at PT school, employment status, state(s) of practice, range of patients, employment setting; 2) 10 questions regarding perceptions of the PTs about sleep, including the importance of sleep, the association with function, sleep problems and medical problems, and attitudes about sleep as a professional. Responses were collected on a 4-point Likert scale: Strongly agree, neither agree nor disagree, strongly disagree, and unsure; 3) 4 questions of PTs sleep education, including education in sleep in PT school or after, which topics should be covered about sleep in PT education; 4) 3 to 8 questions concerning the assessment of patients’ sleep, including subjective and objective information, referring patients to a specialist, most typical diagnosis having sleep issues, and if not assessing their patient’s sleep, why not; and 5) 2 to 7 questions concerning the education on sleep to the patients provided by the PTs, including type of education, if education improves sleep outcomes, or why education was not offered. The survey consisted of 23 to 35 questions. The total number of questions presented depended on the answers provided, which drove different questions to follow.The estimated time for completion was about 10 minutes.
Data collection
Study data were collected and managed using Research Electronic Data Capture (REDCap) electronic data capture tools hosted at KUMC secure network [28,29]. REDCap is a secure, webbased software platform designed to support data capture for research studies. Recruitment took part between September and December of 2020. A link provided in the electronic messages took participants to the REDCap survey.
Statistical analysis
Data analysis was performed using SPSS 23 software (Chicago, IL). Descriptive analysis was conducted: Data are presented as mean ± Standard Deviation (SD) (continuous variables) or percentage (categorical variables). Two binary stepwise logistic regressions were conducted to determine which factors best predicted the positive response “yes” to the questions “Do you routinely assess your patient’s sleep habits or quality of sleep?”, and “Do you routinely educate your patients about the importance of sleep?” Five predictor demographic variables were chosen for the models (as 72.2% of the cases can be classified correctly for the first question and 75.2% for the second model): Gender, age, degree, years since graduation at physiotherapy school, and age range of patients. The statistical significance was set as p<0.05.
Demographics
A total of 224 responses were received. The mean age of respondents was 36.4 years-old (SD ± 8.13), with 70.5% declaring female gender, 13.4% declaring male gender, and 16.1% not declaring gender. Regarding scholarity, 35.5% completed an entry-level physiotherapy program (bachelor), 29% completed continuing education programs (i.e., after bachelor, called latu sensu or specializations courses in Brazil), 12.1% held a master’s degree, 5.4% held a doctorate degree, and 1.8% had post-doctoral training, and 16.5% did not declare. For information on years since graduation, 21% had 1-5 years since graduation, 20.5% had 6-10, 23.7% had 11-15, 10.7% had 16-20, 3.6% had 21-25, 2.7% had 26-30 and 1.3% had more than 30 years of graduation.
Employment status were as follows: 44.6% worked full time (40 h/week), 28.6% part time (20 h/week) and 10.3% were not in contact with patients. The age range of patients attended were: 4.5% of PTs attended patients from 0-18 months, 6.5% form 19 months-9 years old, 7.1% from 10-14 years, 8% from 15-18 years, 38.4% from 19-39 years, 59.8% from 40-59 years and 58% attended patients with 60 years old or more. Many PTs attended more than one age range. The setting of the current primary work were acute care/hospital (32.1%), ambulatory (20.5%), wellness, prevention, sports and fitness (15.6%), home care (7.6%), and not practicing as a clinician (6.3%).
PT’s attitudes regarding sleep
About PT’s attitudes regarding sleep, 98.9% of the respondents agreed that sleep is important for overall health, 92.9% thought that poor sleep is associated with impaired function, 91.8% agreed that PTs should routinely ask patients about sleep problems, 97.8% agreed that sleep disorders may contribute to medical problems, 96.7% answered that PTs should ask about patient’s sleep habits and quality, 71.6% thought that PTs should perform subjective assessment of sleep, 88% agreed that they should counsel patients regarding improvement of sleep quality, 87.4% on sleep position, 92.9% thought that assessing patient’s sleep habits and quality is important, and 94.5% responded that addressing sleep issues impacts PT and rehabilitation outcomes. Disagreement with statements on PTs’ attitudes regarding sleep was not frequent (n=4). For more details on PTs responses, see Table 1.
| Sleep quality | Agree | Neither | Disagree | Unsure |
|---|---|---|---|---|
| Sleep is important to people’s health | 98.9 (181) | 0 (0) | 0 (0) | 1.1 (2) |
| Poor sleep is associated with impaired function | 92.9 (170) | 4. (9) | 0 (0) | 2.2 (4) |
| I should routinely ask patients about sleep problems | 91.8 (168) | 5.5 (10) | 0.5 (1) | 2.2 (4) |
| Sleep disorders may contribute to medical problems | 97.8 (179) | 0.5 (1) | 0 (0) | 1.6 (3) |
| PTs should ask their patients about their sleep habits and sleep quality | 97.6 (177) | 2.2 (4) | 0 (0) | 1.1 (2) |
| PTs should perform subjective assessment to assess sleep habits and quality | 71.6 (131) | 19.1 (35) | 0.5 (1) | 8.7 (16) |
| PTs should counsel patients regarding improvement of sleep quality | 88.0 (161) | 9.8 (18) | 0 (0) | 2.2 (4) |
| PTs should counsel patients on sleep position | 87.4 (160) | 10.4 (19) | 1.1 (2) | 1.1 (2) |
| Assessing my patients sleep habits and quality is important | 92.9 (170) | 4.4 (8) | 0 (0) | 2.7 (5) |
| Addressing sleep issues may impact physiotherapy outcomes | 94.5 (173) | 2.2 (4) | 0 (0) | 3.3 (6) |
Note: n=183
Table 1: Physiotherapist's attitudes regarding sleep % (n).
PT’s education on sleep and their perception of the need for sleep education
The majority of PTs (79.4%, n=143) did not receive education about sleep during entry-level physiotherapy education. However, 35.6% (n=64) received it for continuing education and advanced degrees, other than physiotherapy school. Table 2, shows respondent’s opinions on where specific sleep education topics should be taught (if at physiotherapy school, at post-graduation or continuing education, or if these should not be taught at all).
| Information on sleep and sleep disorders should be taught | Physiotherapy school | Continuing education | Post-graduation courses | Should not be taught |
|---|---|---|---|---|
| Basic physiology of sleep | 70.5 (158) | 2.7 (6) | 5.4 (12) | 0.4 (1) |
| Advanced physiology of sleepd | 18.3 (41) | 17.9 (40) | 42.0 (94) | 0.4 (1) |
| Common causes of sleep issuesa | 69.9 (156) | 4.0 (9) | 4.9 (11) | 21.4 (48) |
| Epidemiology and causes of common sleep disordersd | 65.6 (147) | 2.7 (6) | 9.4 (21) | 0.9 (2) |
| Common medical treatments of sleep disorders | 51.8 (116) | 6.7 (15) | 19.2 (43) | 1.3 (3) |
| Prevention of common sleep disorders | 68.8 (154) | 3.6 (8) | 6.7 (15) | 0 (0) |
| Assessment of sleep quality | 62.9 (141) | 5.8 (13) | 10.3 (23) | 0 (0) |
| Assessment of sleepiness | 45.1 (101) | 9.8 (22) | 23.2 (52) | 0.9 (2) |
| Screening for potential sleep disordersb | 47.8 (107) | 10.3 (23) | 20.5 (46) | 0.4 (1) |
| Interventions to address patient's sleep issues | 46.9 (105) | 8.5 (19) | 23.2 (52) | 0.4 (1) |
| Promotion of healthy sleep habits and quality of sleep | 54.0 (121) | 5.8 (13) | 19.2 (43) | 0 (0) |
| Impact of sleep on cardiovascular disease | 65.6 (147) | 5.8 (13) | 7.6 (17) | 0 (0) |
| Impact of sleep on diabetesd | 51.8 (116) | 6.7 (15) | 20.1 (45) | 0 (0) |
| Impact of sleep on dementiad | 51.8 (116) | 6.7 (15) | 20.1 (45) | 0 (0) |
| Impact of sleep on stroke riskd | 52.7 (118) | 7.1 (16) | 18.8 (42) | 0 (0) |
| Impact of sleep on cognitive functione | 51.8 (116) | 7.1 (16) | 19.2 (43) | 0 (0) |
| Impact of sleep on learningd | 52.7 (118) | 7.1 (16) | 18.8 (42) | 0 (0) |
| Impact of sleep on painc | 56.7 (127) | 5.4 (12) | 16.1 (36) | 0 (0) |
Note: Post-graduation courses: Strictu sensu courses, such as Master and Doctorate (Ph.D.), Continuing education: Latu sensu or specialization courses. n=177, except where stated: an =224, bn=180, cn=178, dn=176 and en=175.
Table 2: PTs responses to where (at physiotherapy school, at post-graduation or continuing education, or should not be taught) specific sleep education topics should be taught % (n).
PT’s assessment of patient’s sleep
In clinical practice, 56.8% of respondents routinely assessed their patient’s sleep habits and quality. Headache, acute and chronic neck pain, acute and chronic back pain, and fibromyalgia were the most common diagnoses that patients presented alongside sleep issues (Figure 1). The majority of PTs (82.3%) asked their patients for subjective information about their patient’s sleep habits or quality of sleep. Only 19.8% of respondents routinely administered sleep questionnaires in their clinical practice. These respondents indicated using the following questionnaires: Sleepiness- Epworth Sleepiness Scale (ESS, 41.2%, n=7), and Karolinska Sleepiness Scale (KSS, 5.9%, n=1); Quality of sleep- Pittsburgh Sleep Quality Index (PSQI, 5.9%, n=1); Insomnia severity-Insomnia Severity Index (ISI, 11.8%, n=2); and sleep apnea-berlin questionnaire (5.9%, n=1), Neck, Obesity, Snoring, Age, Gender (NOSAS) score (5.9%, n=1), and Stop-Bang Questionnaire (SBQ, 5.9%, n=1). Combined use of questionnaires was reported by all respondents as: Berlin+stop-bang (5.9%, n=1), Berlin+KSS (5.9%, n=1), ESS+Berlin+stop-bang (5.9%, n=1), ESS+PSQI+stop-bang (5.9%, n=1), ESS+PSQI+ISI (5.9%, n=1), ESS+PSQI+Berlin+NOSAS (5.9%, n=1), and ESS+stopbang+ PSQI+ISI (5.9%, n=1). When asked about other methods to assess their patient’s sleep, 16.7% (n=16) of the respondents informed to have access to objective sleep information, but only 15 participants answered which device or questionnaire was used, such as: Polysomnography (26.7%, n=4), Actigraphy (6.7%, n=1), and app/smart watches/wearable devices (6.7%, n=1); and to detailed and specific questions about sleep (40%, n=6), and sleep diaries (6.7%, n=1). 37.5% of respondents routinely referred their patients for additional evaluation by a sleep specialist.
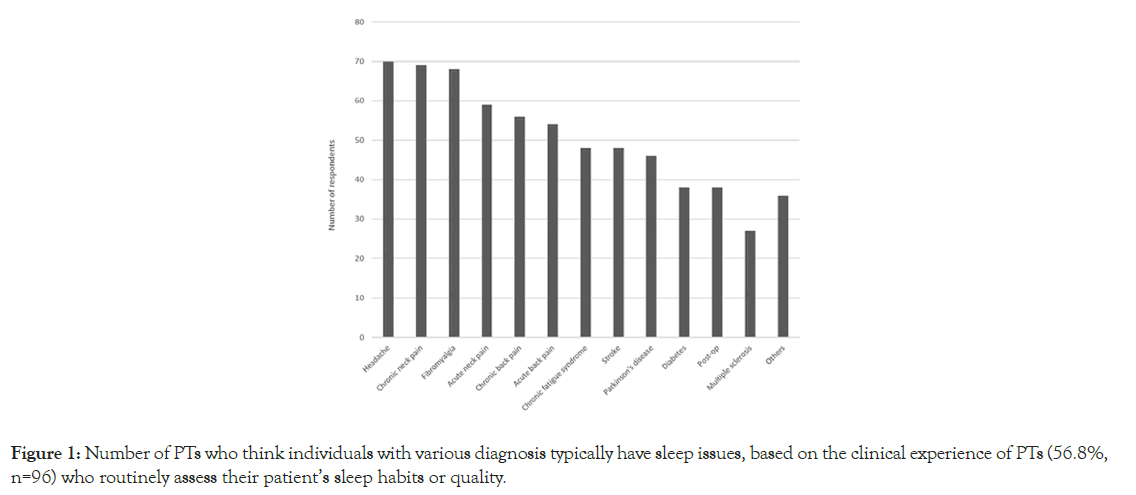
Figure 1:Number of PTs who think individuals with various diagnosis typically have sleep issues, based on the clinical experience of PTs (56.8%, n=96) who routinely assess their patient’s sleep habits or quality.
PTs educating patient’s regarding sleep
More than a half (56.4%) of the PTs responded routinely educating their patients regarding sleep importance, and 75.3% responded thinking that their patients follow the education they have provided. 59.4% of respondents indicated educating their patients on how to improve their sleep quality.
Participants who responded “yes” to any of these three previous questions were further asked if they think patient education improves their sleep quality and impacts rehabilitation outcomes, to which 96.9% responded “yes”. 54.2% of PTs educated their patients on positioning strategies for optimal sleep. From those who do not educate their patients about sleep, the reasons are: Lack of knowledge on how to educate patients about sleep or sleep hygiene techniques (22.8%), lack of time (3.6%), think most patients do not need sleep education (1.8%), and having the opinion that providing education about sleep or sleep hygiene is beyond scope of practice of physiotherapy (1.3%) (Table 3).
| Do you routinely assess your patient's sleep habits or quality of sleep? a | No | Why do you not routinely assess your patient's sleep habits or quality of sleep? b | I do not have time | 4.0 (9) |
| I do not know how to assess sleep habits or quality | 24.1 (54) | |||
| I do not think sleep is important to assess | 0.0 (0) | |||
| I think assessing sleep is beyond PTs scope of practice | 0.9 (2) | |||
| Other | 6.3 (14) | |||
| Yes | Of those who answered "yes" : c | - | ||
| Do you routinely ask subjective information about your patient's sleep habits or quality of sleep? | No | - | - | 17.7 (17) |
| Yes | 82.3 (79) | |||
| Do you routinely administer a sleep questionnaire? | No | - | - | 80.2 (77) |
| Yes | 19.8 (19) | |||
| Do you use other methods to assess your patient's sleep not already listed or described in this survey? | No | - | - | 83.3 (80) |
| Yes | 16.7 (16) | |||
| Do you routinely refer your patients to a sleep specialist for additional assessment? | No | - | - | 62.5 (60) |
| Yes | 37.5 (36) |
Note: a n=169, b n=224 and c n=96
Table 3: PTs’ assessment of patient’s sleep.
Factors impacting physiotherapy assessment and treatment of sleep
The logistic regression showed that female PTs have a 2.6-fold increased chance of assessing their patient’s sleep habits and quality of sleep (p<0.05). In addition, patients aged between 40- 59 years-old presented less chance of having their sleep habits or quality of sleep assessed (p<0.05). Younger PTs had a 1.1- fold increase of routinely educating their patients about the importance of sleep. Patients aged between 15-18 years and 40-59 years had less chances of being educated about the importance of sleep (Table 4).
| Predictors | B | Wald | df | Significance | Exp (B) | 95% C.I. for Exp (B) | ||
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
| Dependent variable: “YES” response to: "Do you routinely assess your patients’ sleep habits or quality of sleep?"** | ||||||||
| Sex | ||||||||
| Women | 0.97 | 3.892 | 1 | 0.048* | 2.634 | 1.006 | 6.897 | |
| 0.41 | 1.993 | 1 | 0.158 | 1.042 | 0.984 | 1.103 | ||
| Degree | ||||||||
| Continuing education | 1.48 | 0.753 | 1 | 0.386 | 4.41 | 0.154 | 125.996 | |
| Bachelor | 0.82 | 0.243 | 1 | 0.622 | 2.277 | 0.086 | 60.11 | |
| Master | 2.665 | 2.178 | 1 | 0.14 | 14.367 | 0.417 | 494.854 | |
| Doctorate | 2.096 | 1.286 | 1 | 0.257 | 8.134 | 0.217 | 304.439 | |
| Years since graduation | ||||||||
| 1-5 | -19.118 | 0 | 1 | 0.999 | 0 | 0 | 0 | |
| 6-10 | -19.859 | 0 | 1 | 0.999 | 0 | 0 | 0 | |
| 11-15 | -20.944 | 0 | 1 | 0.999 | 0 | 0 | 0 | |
| 16-20 | -19.548 | 0 | 1 | 0.999 | 0 | 0 | 0 | |
| 21-25 | -19.084 | 0 | 1 | 0.999 | 0 | 0 | 0 | |
| 26-30 | -17.95 | 0 | 1 | 0.999 | 0 | 0 | 0 | |
| Age range of patients | ||||||||
| 0-18 months | -1.389 | 1.551 | 1 | 0.213 | 0.249 | 0.028 | 2.219 | |
| 19 months-9 yrs | 1.34 | 1.55 | 1 | 0.213 | 3.819 | 0.463 | 31.476 | |
| 10 yrs-14 yrs | -0.175 | 0.046 | 1 | 0.83 | 0.84 | 0.17 | 4.146 | |
| 15 yrs-18 yrs | -1.27 | 2.338 | 1 | 0.126 | 0.281 | 0.055 | 1.431 | |
| 19 yrs-39 yrs | 0.222 | 0.291 | 1 | 0.59 | 1.248 | 0.558 | 2.794 | |
| 40 yrs-59 yrs | -1.36 | 9.482 | 1 | 0.002* | 0.257 | 0.109 | 0.611 | |
| > 60 yrs | 0.248 | 0.382 | 1 | 0.537 | 1.282 | 0.584 | 2.814 | |
| Constant | 18.136 | 0 | 1 | 0.999 | 75227855 | |||
| Dependent variable: “YES” response to: "Do you routinely educate your patients about the importance of sleep?"# | ||||||||
| Sex | ||||||||
| Women | 1.073 | 2.946 | 1 | 0.086 | 2.924 | 0.859 | 9.956 | |
| 0.095 | 6.006 | 1 | 0.014* | 1.1 | 1.019 | 1.187 | ||
| Degree | ||||||||
| Bachelor | -0.043 | 0 | 1 | 0.985 | 0.958 | 0.012 | 73.701 | |
| Continuing education | 1.257 | 0.317 | 1 | 0.573 | 3.514 | 0.044 | 279.095 | |
| Master | 1.061 | 0.213 | 1 | 0.645 | 2.89 | 0.032 | 262.985 | |
| Doctorate | 2.371 | 0.912 | 1 | 0.34 | 10.705 | 0.082 | 1389.812 | |
| Years since graduation | ||||||||
| 1-5 | -18.236 | 0 | 1 | 0.999 | 0 | 0 | 0 | |
| 6-10 | -19.363 | 0 | 1 | 0.999 | 0 | 0 | 0 | |
| 11-15 | -19.662 | 0 | 1 | 0.999 | 0 | 0 | 0 | |
| 16-20 | -20.669 | 0 | 1 | 0.999 | 0 | 0 | 0 | |
| 21-25 | -19.879 | 0 | 1 | 0.999 | 0 | 0 | 0 | |
| 26-30 | -20.409 | 0 | 1 | 0.999 | 0 | 0 | 0 | |
| Age range of patients | ||||||||
| 0-18 months | 0.087 | 0.005 | 1 | 0.942 | 1.091 | 0.106 | 11.247 | |
| 19 months-9 yrs | -0.349 | 0.072 | 1 | 0.789 | 0.706 | 0.055 | 9.058 | |
| 10 yrs-14 yrs | 1.109 | 1.136 | 1 | 0.287 | 3.031 | 0.394 | 23.302 | |
| 15 yrs-18 yrs | -2.284 | 4.746 | 1 | 0.029* | 0.102 | 0.013 | 0.795 | |
| 19 yrs-39 yrs | 0.356 | 0.561 | 1 | 0.454 | 1.428 | 0.562 | 3.624 | |
| 40 yrs-59 yrs | -1.109 | 4.553 | 1 | 0.033* | 0.33 | 0.119 | 0.914 | |
| > 60 yrs | 0.71 | 2.347 | 1 | 0.125 | 2.035 | 0.82 | 5.049 | |
| Constant | 0 | 1 | 0.999 | 9.16E+15 | ||||
Note: *p<0.05; **pseudo R2=0.395 (Hosmer and Lemeshow); 2.227 (Cox and Snell); 0.305 (Nagelkerke). X2= 43.52, df=19, p<0.001; #pseudo R2=0.436 (Hosmer and Lemeshow); 0.349 (Cox and Snell); 0.468 (Nagelkerke). X2= 43.52, df=19 and p<0.001
Table 4: Predictor variables.
This survey provides a “snapshot” of perceptions and attitudes about sleep from PTs practicing in Brazil in their daily clinical practice at the end of 2020. These perceptions and attitudes are important to understand, as they may develop more opportunities for focusing physiotherapy sleep education on behalf of patients and the community. Physiotherapy, as a profession, is continuously growing and changing. PTs have been spending longer time with their patients (due to the nature of the profession-weekly, sometimes daily), which creates a familiar opportunity to understand lifestyle and sleep. In addition, sleep impairments impact rehabilitation and physiotherapy outcomes, therefore knowledge and education about sleep could directly impact patients. As sleep is a relatively “new” area in medicine and is influencing new professions to open new venues, evaluating PTs knowledge and views on sleep is imperative.
Our sample was representative of the currently practicing Brazilian PTs, as 70% of PTs are women (60% of PTs in Brazil are women, about 36 years old, and commonly have completed entry-level physiotherapy school (i.e., bachelor’s degree) and continuing education [30]. The majority of PTs who responded to the survey have less than 20 years of practice, almost all worked full time at primary acute care, hospitals and ambulatory, and the majority worked in São Paulo, the most populous state in the country.
The overwhelmingly majority of PTs agreed that sleep is important for health that poor sleep is associated with impaired function that poor sleep negatively contributes to medical problems and that addressing these issues may impact rehabilitation and physiotherapy outcomes. Respondent PTs indicated that they should ask their patients about sleep habits, quality, and issues, as well as assess and counsel them about improvement of sleep quality, including sleep positioning. These findings are in accordance with previous investigations on PTs perception and attitude about sleep in the United States of America (USA) Pakistan and Jordan [13,11,14]. About 9% of the sample was unsure if PTs should perform subjective assessment of sleep, and 24% of the sample showed lack of knowledge on evaluating sleep and the instruments used.
The vast majority of PTs did not receive education about sleep in PT entry-level school. Fortunately, PTs seem to be receiving sleep education in continuing education programs and advanced degrees. PTs indicated that basic sleep physiology, common causes and epidemiology of sleep disorders, prevention and assessment of sleep disorders should be taught in entry-level physiotherapy school. PTs also indicated that advanced physiology of sleep, specific assessments (i.e., for sleepiness) and interventions to address sleep issues should be taught at post-graduation (both lactu and strictu sensu) programs. Surprisingly, one fifth of the sample responded that common causes of sleep should not be taught in physiotherapy programs at all. A recent meta-analysis demonstrated that health practitioners, including PTs, would respond positively to evaluation and promotion of sleep health if they had the relevant knowledge and skills [9]. Sleep evaluation and basic sleep recommendations need to be considered as fundamental clinical competency in contemporary physical therapy practice [31].
Despite the lack of education on sleep, more than a half of respondents routinely assess their patient’s sleep habits and quality of sleep. However, only one fifth of the sample used validated questionnaires in their sleep assessments. Those PTs who assessed sleep from their patients, seem to do it mainly while working with patients with pain syndromes, such as headache, acute and chronic neck and low back pain and fibromyalgia. This could be due to continuing education and post-graduation after entry-level PT in Brazil. After physiotherapy school, almost all PTs choose an area of specialization, for which they will study for an extra year to pass an exam and get a post-graduation (latu sensu) degree. The Brazilian Federal Council of Physiotherapy and Occupational Therapy (COFFITO) requires this continuing education for the PTs to have a recognition of expertise/specialization title. In pain education curricula, there has been special attention to sleep issues, as some Brazilian research groups are considered leaders on animal and human research models about pain-sleep relationship [32]. Furthermore, pain has been studied by several research groups in Brazil, with findings associating lack of sleep or impaired sleep with enhanced pain perception, which disrupts the sleep cycle [19,33-36]. From respondents who do not assess their patient’s sleep, almost one fourth was because they did not know how to perform the assessment, indicating lack of knowledge of physiotherapy sleep education. In addition, 1% indicated that sleep education is beyond the scope of physiotherapy practice again. Indicating that more information is needed and that entrylevel physiotherapy schools should consider incorporating sleep topics in their curricula. In addition, from those who did not educate their patients about sleep, more than a fifth of the sample does not know how to educate them on quality and sleep hygiene tips. More than one third referred their patient for additional assessment of sleep. These findings are in line with the survey in the USA, and contrary to the survey in Jordan, probably due to cultural and historical aspects of the profession [13,14].
Female PTs presented more chances of assessing the patient’s sleep habits and quality of sleep. This result might be due to the fact that physiotherapy is a profession dominated by women worldwide, deeply rooted in sociological context of the profession development [37,38]. Interestingly, and showing an updated and modern physiotherapy as a profession, younger PTs presented 1.1- fold increased chance of routinely educating their patients about the importance of sleep. This can be due to sleep science gaining space in medical fields, media, research, newly published books and courses on the subject. This data foresaw a step forward in Brazilian physiotherapy one year after this study. In August 2021, the Brazilian Federal Council of Physiotherapy and Occupational Therapy (COFFITO) approved a law recognizing the exercise of “Physiotherapy in Sleep Disorders” by PTs in Brazil [39]. In Brazil, PTs work as respiratory therapists, using positive pressure devices to treat patients with respiratory dysfunctions. Our survey showed that patients between 40-59 years old had less chance of being assessed for their sleep habits or quality of sleep, and that patients between 15-18 and 40-59 years old had less chances of being educated about the importance of sleep. Although, statistically significant, present with no clinical importance, some factors not collected in our survey would influence these findings, such as time spent with patients in a physiotherapy session, physiotherapy modalities used (massage, kinesiotherapy, aquatics), and physiotherapy setting. Our findings contradict the findings from the USA study, possibly due to cultural facts and the split physiotherapy and respiratory therapy professions in the USA [13].
Our survey contributes to the body of knowledge on sleep care provided by PTs in Brazil. In 2022 the Brazilian association of sleep published a sleep physiotherapy guideline. This guideline was published by researchers and clinical PTs working in Brazil, both in English, and in Portuguese languages, so that PTs practicing Brazil who do not speak English could also be reached [10]. The clinical guideline brings latest evidence on non-pharmacological treatment of sleep breathing disorders (e.g., obstructive sleep apnea, central sleep apnea, upper airway resistance syndrome, hypoventilation syndromes, overlap syndrome, and pediatric sleep breathing disorders); sleep bruxism; circadian rhythms disturbances; insomnia; and Willis-Ekbom disease/periodic limb movement disorder. Future research should investigate whether this clinical guideline is being implemented in physiotherapy practice by Brazilian PTs.
This study supports the need for education about sleep health and its disorders to better manage the demands of physiotherapy practices in Brazil, and identifies a knowledge gap for PTs in Brazil. Appropriate sleep training programs must be implemented to empower PTs in Brazil with knowledge, skills, tools, and confidence needed to recognize and treat sleep disorders within their scope of practice.
This survey has some limitations. The small sample size and the snowball sampling will not allow researchers to calculate the response rate for the survey. In addition, São Paulo-the state where most respondents worked at-holds two of the biggest sleep groups in research and practice in Brazil, which could have skewed responses to our survey.
• Sleep impairments impact rehabilitation and physiotherapy outcomes, therefore knowledge and education about sleep could directly impact patients.
• Knowledge about sleep interdisciplinary, skills to screen sleep disturbances, promotion of sleep quality and physiotherapeutic treatment of sleep disorders are important components for PTs to promote health and well-being in their patients and in their clinical practice.
• Entry-level PT education programs should consider incorporating education about sleep in curricula, as the development of continuing education courses are urgently needed.
The data that supported the findings of this study are available upon request from the correspondent author.
São Paulo Research Foundation (Grant No. #2018/18952- 1 to CF), and Kansas University Medical Center. The authors acknowledge Michael Sateia MD, for granting permission to use portions of the Dartmouth Sleep Knowledge and Attitude Survey; Klara Papp, PhD, for granting permission to use portions of their survey; and Thomas Heffron from the American Academy of Sleep Medicine for granting permission to use questions from the ASKME survey.
Author declares no conflict of interests.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Frange C (2024). Physiotherapist’s Attitudes and Knowledge Regarding Sleep in Brazil: A Survey Study. J Sleep Disord Ther. 13:573.
Received: 31-Jul-2024, Manuscript No. JSDT-24-33465; Editor assigned: 02-Aug-2024, Pre QC No. JSDT-24-33465 (PQ); Reviewed: 16-Aug-2024, QC No. JSDT-24-33465; Revised: 23-Aug-2024, Manuscript No. JSDT-24-33465 (R); Published: 30-Aug-2024 , DOI: 10.35248/2167-0277.24.13.573
Copyright: © 2024 Frange C. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.