Journal of Developing Drugs
Open Access
ISSN: 2329-6631
ISSN: 2329-6631
Research Article - (2019)Volume 8, Issue 2
Background: Multiple sclerosis (MS) is a chronic autoimmune disorder affecting the central nervous system (CNS). Its cause is still unknown but it is connected to certain demyelination of the axons in the brain and spinal cord. Despite the medical advances, in the 21st century, multiple sclerosis remains an incurable disease. In order to stop the MS progression, we should concentrate our efforts on reversing the process of demyelination and on improving the transmission of nerve impulses along CNS.
Methods: The effects of a treatment with a daily intake of an alcohol extract of snowdrop or a snowdrop-derived drug containing nivaline and other biological active substances (BAS), and an alcohol extract of Atropa belladonna or Atropa belladonna-derived drug combined with regular electro-magnetic physiotherapeutic procedures were analysed in patients with MS.
Results: The daily administration of nivaline and atropine in combination with regular electromagnetic physiotherapeutic procedures showed potential to reverse the course of MS manifesting itself with a clinical remission of patients with MS.
Conclusion: Our findings suggest that the treatment regimen proposed here possesses the potential to stop the process of demyelination in the CNS and stimulate the process of remyelination in MS patients thus achieving a state of clinical remission.
Multiple sclerosis; Nivaline; Atropine; Snowdrop; Atropa belladonna; Magnetic therapy; Copper
Multiple sclerosis (MS) is a chronic inflammatory autoimmune disease affecting the central nervous system (CNS) with no effects on the peripheral nervous system (PNS). It belongs to the group of the neurological demyelinating diseases. MS is characterized by a triad of inflammatory reaction, process of demyelination and gliosis (scarring). The latter gives the name of the disease (from the Greek word “skleros” meaning “scars”). Practically, “ multiple sclerosis ” means presence of “ multiple scars” because the foci, which could be disseminated throughout the whole CNS, are structurally denser than the surrounding nervous tissue.
MS was probably first described by Count Jan Van Bieren of Holland in 1395. He wrote a paper about a Dutch woman, named Lidwina of Sheidam, and her “unknown” disease. At the age of 15, Lidwina started suffering from terrible face pain. Until her death in 1433, at the age of 53, she developed leg weakness with a progressive inability to walk, feel her legs and see with one of her eyes. All these symptoms hindered her ability to practice her favourite sport-ice skating. However, as Count Van Bieren mentioned, she continued helping the others her whole life. Because of her merits, Lidwina was canonized and declared a patron saint of all ice-skaters [1].
The first scientists who described the physical changes (almost simultaneously in 1835) were the French professor of pathologic anatomy Jean Cruveilhier from Sorbonne’s Faculty of Medicine in Paris and the Scotsman Robert Carswell who at that time worked at the Parisian Hôpital de la Pitié and later became professor of pathology at the University College in London. However, the first official scientific report on the MS signs and symptoms belonged to Jean-Martin Charcot who called MS la sclérose en plaques and correlated his observations with the autopsy findings of his patients [2]. Charcot taught Sigmund Freud and his scientific work strongly influenced the developing fields of neuropathology and psychology. He was referred as “the Napoleon of the neuroses”.
MS is a widely spread disorder and the most frequently seen demyelinating disease of the nervous system. Approximately 2.5 million people worldwide suffer from MS-about 400,000 people in the US and according to the European Multiple Sclerosis Platform-about 700,000 people in Europe (70% of them being diagnosed in prime working years). The distribution of prevalence of MS shows areas with high prevalence (>30/100,000), like North Europe and North America, with medium prevalence (5-30/100,000), like South Europe, South USA and Central and South America (10-20/100,000), and with low prevalence (<5/100,000), like Asia and South America [3]. It is interesting to mention that its incidence is greater in big industrial and urban areas than in rural areas [4,5].
Multiple Sclerosis affects individuals between 20 and 40 years of age. In Europe the highest prevalence rates are observed between 35-64 years of age. In western societies, MS is the second most common cause of neurologic disability in early to middle adulthood, being dominated only by traumas. There are rare reports on the occurrence of MS in children (as early as 2 years of age) and in octogenarians. Like many other autoimmune disorders, MS is more common in women than in men [6].
MS affects only the central nervous system, in particular, the brain and the spinal cord, i.e. the myelin sheath of the axons. The morphological basis of MS is the formation of the so-called scars of multiple sclerosis which are foci of myelin damage (demyelination) of the white matter of the brain and the spinal cord. It is believed that T-cells (CD8+ and CD4+) play a central role in the process of demyelination. Antibodies directed against myelin, such as myelin oligodendrocyte glycoprotein (MOG), appear to be an important concomitant pathogenetic factor, together with the pathological T-cell-mediated immune response in MS, and an abnormal humoral immune response.
Microscope slides show that the acute MS lesions are surrounded by inflammatory mononuclear cells (predominantly, T-cells and macrophages) which passed the blood-brain barrier near the site of inflammation (without destroying the wall of the blood vessels). Very often, myelin-specific autoantibodies are also found (for instance, MOG), which promote demyelination and act like stimuli for macrophages and microglial cells that scavenge myelin debris. In the process of evolution of MS plaques, astrocytes start proliferating (gliosis) and the surviving oligodendrocytes (or those differentiating from precursor cells) partially remyelinate the naked axons which survive the MS attacks and produce the so-called shadow plaques. A key role in the process of lesion occurrence is played by interleukin 2 (IL2), tumour necrosis factor alpha (TNF α), and interferon gamma (IFN-γ) [7].
The diversity of the damages on the nervous system, caused by MS, could be explained by the different size of the damaged areas (from 1 mm to several cm), their chaotic distribution among the nerve tracts and their modification within the processes of the disease. Also, in various damaged areas, with the successful treatment the reparation processes take place at different speeds, whereas it is impossible to fully recover the lost functions of the nervous system.
The variety of CNS damages is connected to a great variety of clinical manifestations in time. Among the most common symptoms described by MS patients are fatigue, pain, visual impairment, numbness, bladder of bowel problems, sensory symptoms, weakness, loss of balance and mobility, spasticity, depression, and cognitive impairment [6]. All of the abovementioned determine a poorer health-related quality of life for the MS patients.
Modern neurology categorizes the MS patients into four groups depending on the course of the disease: relapsing-remitting (RRMS, the most common form where symptom flare-ups are followed by periods of asymptomatic remission), secondary progressive MS (SPMS, continuous worsening of disease course with or without remission or leveling off of symptom severity), primary progressive MS (PPMS, gradual and continuous worsening of symptoms since the beginning of the disease without remission, with or without leveling off of symptom severity), and progressive-relapsing (PRMS, a rare progressive form since the beginning with intermittent flare-ups of worsening symptoms and no remission periods) [8].
The basic tool for MS diagnostic is the revised 2017 McDonald Criteria which were published online in The Lancet Neurology on December 21, 2017.
The improvement of the quality of life and the medico-social adaptation extended the life expectancy of the MS patients but in the recent years the number of the MS patients has been increasing, despite the improved diagnostic methods and better treatment.
The cause of MS is still unknown. Currently, the most widely accepted hypothesis is that MS could occur as a result of the interaction of a number of unfavorable external and internal factors. Unfavorable factors are viruses (such as human herpes virus, HHV-6A), and bacterial infections, toxic substances and radiation (including solar radiation), certain eating habits (excessive meat consumption), geo-ecological place of residence (with a very strong influence on children’s organism), traumas, frequent stressful situations, etc. Genetic predisposition to MS is probably connected to the combination, in certain individuals, of several genes determining first and foremost disorders in organism ’ s self-regulation [7,9]. There are proper grounds to claim that MS occurs when there is a shortage of organic gold in human organisms (Kaniskov) [10].
At the end of the 20th century, in the treatment for MS were incorporated medicinal products which can influence the prognosis and slow down its progression, or which can reduce the frequency of the MS attacks. This group of pharmaceutical preparations is called disease-modifying drugs (DMDs). DMDs influence patients’ immune system, one way or another, and belong to the so-called pathogenetic therapy reducing the frequency and duration of the acute MS exacerbations. Unfortunately, they didn ’ t prove to be effective curative or preventive options.
The US Food and Drug Administration (FDA) approved several disease-modifying treatments for the pathogenetic therapy of MS. Four of them belong to the group of the beta interferon drugs (Biogen ’ s Avonex®, INN-Interferon Beta-1a, Merck Serono’s Rebif®, INN-interferon beta-1a, Bayer’s Betaferon®, INN-recombinant interferon beta-1b, and Novartis ’ Extavia®, INN-recombinant interferon beta-1b). Interferon beta (IFN-β) is a natural cytokine typically produced by fibroblasts and interferon alpha (IFN-α) by plasmacytoid dendritic cells. They belong to the Type I interferon which are tissue- and genespecific and play an important role in antiviral immunity, cell proliferation, immune regulation, cytoprotection, and possibly fertility. The exact mechanism of action of IFNs remains unknown and depends on the time of exposure, interactions with other drugs, and environmental factors [11].
The following DMDs are also approved by FDA for the MS treatment: Glatiramer acetate (Teva ’ s COPAXONE®)-a synthesized copolymer of four naturally occurring amino acids (L-glutamic acid, L-lysine, L-alanine, and L-tyrosine); Mitoxantrone (EMD Serono ’ s Novantrone®) -a cytostatic immunosuppressive drug, suppressing the activity of the T-and B-cells, as well as the macrophages attacking myelin sheaths; Natalizumab (Biogen ’ s Tysabri®)-a recombinant humanized IgG4 monoclonal antibody that acts as an α4-integrin antagonist to prevent leukocyte trafficking into the central nervous system; and Fingolimod (Novartis ’ Gilenya)-a sphingosine-1-phosphate receptor modulator which after being metabolized to its active metabolite blocks the lymphocytic migration from the lymph nodes. In randomized controlled trials (RCTs), all of the above-mentioned pharmaceuticals showed efficacy in shortening the duration and decreasing the frequency of the MS relapse rates. Moreover, Betaferon and Mitoxantrone proved to reduce patients ’ disability scores in secondary progressive multiple sclerosis (SPMS) [8]. However, none of these drugs influences significantly patients with primary progressive multiple sclerosis (PPMS).
Numerous other therapies are used for the symptomatic treatment for MS and as off-label treatment options. Some papers report a positive effect of low-dose naltrexone (LDN) with doses up to 5 mg/24 h. Naltrexone is an opioid receptor antagonist which is used to reduce muscle cramps and subsequent fatigue and depression. One RCT showed no serious drug events in LDN and decreased spasticity in patients with PPMS. Another RCT reported an improved quality of life (QoL), indicated by health-related quality of life (HRQoL) assessment tools [12].
As far as pathogenesis is concerned, it is justifiable to use angioprotectors, antiaggregants, antioxidants, inhibitors of proteolytic enzymes, and enhancers of brain metabolism (in particular, vitamins, amino acids, nootropics) in the treatment for MS [13].
In 2011, in the Russian Federation, the Ministry of Health and Social Development approved the Alemtuzumab (Кэмпас®, Campath®) humanized monoclonal antibody against CD52 for the treatment for MS. In September 2013, it was also approved by the European Medicines Agency (EMA). In patients with relapsing-remitting multiple sclerosis (RRMS), in the early stages, Alemtuzumab proved to be superior to Interferon Beta-1a. However, it is often associated with serious autoimmune adverse events, such as immune thrombocytopenic purpura (ITP), thyroid disorders, nephropathy and infections [14].
The US National Multiple Sclerosis Society (NMSS) publishes regularly on its website reports on clinical trials and their results. Since 2005 bone marrow transplantation (BMT) has effectively been used for the treatment for MS. Patients firstly undergo chemotherapy in order to destroy their own bone marrow and after that donor’s bone marrow is transplanted. Donor’s blood passes through a specially designed separator that separates erythrocytes.
In so far as the actual cause of the disease remains unknown, it is not possible to develop an etiotropic treatment for MS. To date, there are no reliable reports on full recovery from MS.
Based on the analysis of the existing MS treatment regimens of the Bulgarian herbal medicine, the modern advances in phytotherapy related to the latest quantum mechanisms [15], the profound with a scientific research in this area and the established treatment in conventional medicine, the main objective of this paper is to develop and practically implement a successful treatment regimen for MS patients relying on phytotherapy and physiotherapy methods. An additional objective would be to combine (most of all, in acute MS relapses) the contemporary scientific medical methods with phytotherapy and physiotherapy.
In order to realize the objective of this scientific research, the following main tasks are being set: to investigate the current state of MS, the essence and the development of the problems associated with the implementation of phytotherapy (as a basic treatment) and physiotherapy (as an additional treatment) for the therapy of MS in the methodic of modern medicine; to develop a reasonable scientific-practical methodology for phytotherapy and physiotherapy in MS, and to realize an experimental research of the methodology proposed for phytotherapy and physiotherapy in MS and its coherence with the modern medical methods.
The main object of this paper is the biological form of matter in motion-human’s physical body in its unnatural state of disease (in particular, multiple sclerosis). The subject of the paper comprises the theoretical, methodology and practically applicable matters related to the treatment for MS in the human body with the application of the methods of phytotherapy and physiotherapy in accordance with the data from the experience and knowledge of phytotherapy, collected up to this moment as a main part of the so-called natural scientific methods for treatment and prevention.
Myelin is a complex membranous structure which wraps around axons in the central (CNS) and peripheral nervous system (PNS) forming the so-called myelin sheath of nerve axons. Myelin was first described by the Dutch Antony van Leeuwenhoek in 1717 but received its name from the German pathologist Rudolf Ludwig Virchow [16]. Myelin sheath is extended and modified plasma membrane ensheathing nerve axons in a spiral fashion acting as an electrical isolating coating. It is formed by glial cells-Schwann cells in PNS and oligodendrocytes in CNS. Myelin sheath is constructed by the flat processes of the glial cells (lamellipodia) which ensheathe repeatedly the axons like an isolating band. In actual fact, lamellipodia contain no cytoplasm. As a result, myelin sheath itself represents multiple cell membrane layers. Approximately 70%-75% of myelin consists of lipids, and 25%-30% represent proteins [17,18]. The high lipid contents distinguish myelin from the other biological membranes.
Although myelin acts as an insulating agent in the nervous system its function of facilitating conductivity is not analogues to the one in electrical circuits. Myelin increases the axonal diameter and the axonal resistance and decreases the axonal capacitance (the ability to store an electric charge). According to laws of physics, higher resistance and lower capacitance translate into higher speed of transmission [19]. Propagation of nerve impulses shows some differences in myelinated and unmyelinated fibers. In unmyelinated fibers, signals are propagated by local circuits of ionic currents that flow into the active region of axonal membrane, through the axon and out through adjacent sections of nerve membrane, so that the local circuits depolarize the adjacent membrane section sequentially. On the other side, in myelinated axons, excitable axonal membrane is exposed to the extracellular space only at the nodes of Ranvier (the nodal gaps between the isolated segments) where sodium channels are located. When the membrane at the node is excited, the local circuit generated cannot flow through the high-resistance sheath and, therefore, flows out through and depolarizes the membrane at the next node. The low capacitance of the sheath means that little energy is required to depolarize the remaining membrane between the nodes which results in local circuit spreading at an increased speed. Active excitation (nerve impulses) of the axonal membrane jumps from node to node and this form of impulse propagation is called salutatory conduction (from the Latin word “saltare” meaning “to jump”) [20,21].
When a MS scar appears inflammatory cells (lymphocytes and macrophages) migrate to and gather along the damaged segment. As a result, a swelling appears in this area of the neuron and myelin is destroyed. Inflammatory cells enter the myelin, disintegrate it and “break it to pieces”. The function of the myelin sheath is compromised and the process of transmission of electrical impulses (signals) along the nerve axons is altered. Subsequently, functional disorders appear which manifest as MS symptoms.
Simultaneously to or following demyelination, another important process takes place-the process of myelin recovery (remyelination). Remyelination possesses the potential to restore the lost conductivity and plays a neuroprotective role. Remyelination occurs extensively but due to unknown reasons could not be adequately completed or fails. Experiments showed that the process of myelin recovery has two phases. During the first phase oligodendrocyte progenitor cells (OPS) migrate to and colonise the MS lesions. Subsequently, they differentiate into myelinating oligodendrocytes which contact the damaged axons and envelope them (second phase) [22]. Several hypotheses have been suggested in order to explain the failure of the process of remyelination. According to some authors, this is due to a loss and destruction of oligodendrocyte progenitor cells within the lesions in the course of repeated de- and remyelination or (in lesions with an abundance of OPS) because axons are not permissive for remyelination, or due to inhibition of progenitor cells’ maturation [23].
Biophysics and bioelectronics in neurons
Electricity comprises all phenomena driven by the existence, interaction and motion of electrically charged particles. Such particles are electrons (in metals) and ions (cations and anions in electrolyte solutions). The human body is a complex collection of electrons and ions. Current flows along the surface and inside nerve cells and fibers. The average velocity at which electrons travel in a conductor (drift velocity) when subjected to an electric filed is ca. 1 mm/s. The electromagnetic wave rippling through the electrons propagates at a speed approximating 90% of the speed of light (ca. 270,000 m/s). However, nerve impulses travel along nerve tracts much slower with a maximal speed of approximately 120 m/s (Data is taken from The Discovery Magazine, 2011).
The electric current changes its medium. It generates heat energy in conductors (this effect is not observed in superconductors) and changes the chemical composition of its conductor (especially in electrolyte solutions-in human organism and in particular in nerve fibers) creating a magnetic field (in all conductors without exception, in human organism and in particular in nerve fibers) which can be measured [24].
Magnetism is a form of interaction between electrical charges in motion which is realized at a distance with the means of the (electromagnetic) field. Along with electricity, magnetism represents a form of manifestation of electromagnetic interactions. As far as quantum theories are concerned, electromagnetic interactions are transmitted by bosons-photons (particles which could be represented as quantum excitation of electromagnetic fields) [25].
Conductors are substances with a high electrical conductivity. Usually, in nature metals and electrolyte solutions are conductors. Bioelectricity is performed by means of ionic flows (cations and anions-with a removed or gained electron) along living structures and plays an essential role in all vital processes. It creates a biopotential between both sides of cell membranes. The transmission of nerve impulses is executed with the help of electrochemical signals (action potentials) which have already been scientifically investigated in detail [26].
The processes of transmission of electrical impulses could be damaged by changes in the electrical conductivity of fluids, electrolyte solutions and conductors (respectively, tissue fluids in human organism) and changes in the magnitude of a magnetic field in or around a conductor (respectively, nerve fibers and neurons). Numerous studies show that the most sensitive systems in human physical body are the nervous, immune, endocrine and reproductive system which are of decisive importance for its correct functioning.
In order to overcome MS, we need to promote the transmission of nerve impulses through electrochemical signals and to increase the quality of ionic motion/current (cations and anions) and electrons in all vital processes-intracellularly, as well as in the different parts of human organism and its organs. We should improve the nerve impulse conduction and stability, restore the integrity of the nerve complexes (nerve fibres, neurons, etc.), and maintain the steadiness of the positive results achieved in the process of recovery.
In the treatment for MS, the following practical methods for natural therapy (phyto- and physiotherapy) are introduced.
Improvement of nerve impulse conduction and stability through intake of biological active substances (BAS) isolated from medicinal plants
Galantus nivalis (common snowdrop):
Botanical description: The common snowdrop (Galantus nivalis) is the most popular representative of a small genus consisting of approximately 20 species of the Amaryllidaceae Family and is among the first bulbs to bloom in spring. They are perennial, herbaceous plants whose stem reaches around 20 cm. The leaves are flat and elongated (ca. 15 cm long and 15 cm wide). The flower is white and single, and consists of 6 tepals (segments), as the inner flower segments are half as small as the outer ones and merge with the small sinus (notch) at the tip (Figure 1). They bloom between January and April (in the north temperature zone) and between January and May (in the wild). Galantus nivalis grow in Central Europe and on the Balkan peninsular. They usually grow in brushwood areas, woodlands and meadows up to 1800 m above sea level [27-30].
Figure 1. Galantus nivalis.
Chemical composition:The whole plant (flower, leaves, bulb) contains tanning substances (nivaline, galantamine, lycorine, tacetine, nivalidine) which improve the transmission of nerve impulses, increase the skeletal and smooth muscle tone, have a peripheral vasodilating effect, reduce blood pressure and promote the function of different organs. In Bulgaria, nivaline (galantamine hydrobromide) was first isolated by one of the founders of modern Bulgarian pharmacology Prof. Dimitar Paskov and Lilia Bubeva-Ivanova (research assistant and master of pharmacy) in 1956. Two years later, in 1958, the Bulgarian Sopharma Pharmaceutical Company initiated the production of Nivalin®, a drug being famous worldwide for its effectiveness in the treatment of poliomyelitis and infantile cerebral palsy which is now produced in 10 other countries, too. Nivaline is a tertiary amine and anticholinesterase agent with positive effects on reflex arcs in CNS and PNS, central synapses of vegetative ganglia, myoneural junctions, sensory receptors etc. [31,32]. To a certain extent, the chemical structure and pharmacological effects of the other BAS of Galantus nivalis, have already been investigated [33-36].
Preparation and usage: An alcohol extract of Galantus nivalis is prepared as follows: 200 ml of 40% alcohol solution should be added to 4 table spoons of chopped bulbs. The mixture is allowed to stay for 14 days and should be well stirred every day. After 14 days, the solution should be filtered. Intake: 10-30 drops tid or qid, 3-5 minutes before meals. One could also use Sopharma’s Nivalin® 5 mg. Dosage depends on the severity of the disease (usually, 5 mg bid before meals) [37].
Contraindications:Snowdrop extracts are contraindicated in angina pectoris, heart failure, epilepsy and bronchial asthma.
Restoration of the integrity of the nerve complexes (nerve fibres, neurons, etc.) through intake of BAS from Atropa belladonna:
Atropa belladonna:
Botanical description: Atropa belladonna, also known as belladonna and deadly nightshade, is a perennial herbaceous plant from the Solanaceae Family. They have ovate green leaves and bell-shaped, dull purple flowers. Fruits are berries and shiny black, with a diameter of approximately 1 cm (Figure 2). Atropa belladonna can grow up to 1 m. They grow in Europe, North Africa and West Asia and are naturalised in some parts of North America [38].

Figure 2. Atropa belladonna.
Chemical compositions: All parts of the plants contain atropine. Atropine is an alkaloid which was first isolated by the German pharmacist Heinrich Mein in 1831 but its structure was established in the 20th century. It could be artificially synthesized but it is considerably cheaper to extract it from plants. According to modern medicine, the treatment with atropine from belladonna is safer than the usage of the pure alkaloid. Atropine is an actual BAS to treat the symptoms of the Parkinson ’ s disease, meningitis, different types of muscle spasms, etc., [39,40].
Preparation and usage: An alcohol extract of Atropa belladonna is prepared as follows: 200 ml 40% alcohol solution should be added to 4 table spoons of chopped leaves (stalks, flowers). The mixture is allowed to stay for 14 days and should be well stirred every day. After 14 days the solution should be filtered. Intake: 5-15 drops tid or qid, 3-5 minutes before meals [37]. One could also use Sopharma ’ s Bellergamin® 0,1 mg/0,3 mg/20 mg. Dosage depends on the severity of the disease (usually, 1 tbl. bid or tid before meals).
Contraindications: N.B. Atropa belladonna is a very toxic plant and should not be used without medical supervision!
Maintenance of the stability of the phytotherapeutic results achieved through physiotherapy-strengthening of the magnetic field of human body by means of intensive conduction of regulated electrical impulses (method with a copper plate)
Usage: Only in the morning until 10 am. The patient should stand barefoot on a copper plate (35 × 35 cm) between 5 and 30 minutes. The first procedure should be performed for only 5 minutes and every subsequent procedure should be 5 minutes longer than the previous one until reaching 30 minutes (Figure 3).
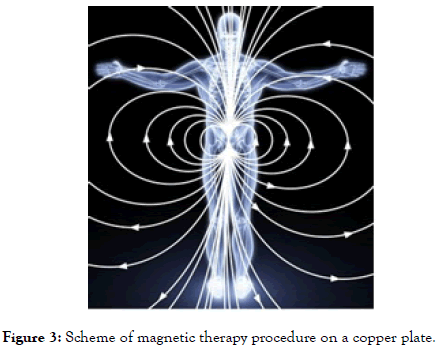
Figure 3. Scheme of magnetic therapy procedure on a copper plate.
Magnet therapy proved in RCTs its favourable effects on patients with MS producing a dramatic and sustained improvement in patients’ disability. The exact mechanism remains unknown but it is hypothesised that it is mediated by the pineal gland [41,42].
Copper (Cu) has been known to take part in myelin synthesis, therefore its deficiency could cause myelinopathy. Experiments showed that copper influences the course of autoimmune disorders through the process of prostaglandin catalysation [43]. Copper bracelets, combined with magnetic therapy, proved to provide pain relief to patients with rheumatoid arthritis which supports the theory that copper could leach through human skin [44]. In mouse and rat models of amyotrophic lateral sclerosis (ALS) with copper deficiency in the spinal cord, copper was delivered in the CNS by means of the positron emission tomography imaging agent CuATSM (an orally bioavailable, blood-brain barrier permeable complex) which prevented their early mortality and extended their survival [45].
Probably the magnetic field enhances the hypothesised penetration of copper in the human body and in particular, in CNS. In order to prove or negate this, we need more extensive trials.
Vassil Kaniskov, together with Prof. Vladimir Feodorovich Korsun and Assoc. Prof. Elena Vladimirovna Korsun, patented a treatment regimen based on the oral administration of alcohol extracts from Galantus nivalis and Atropa belladonna (Pat. No. RU2629385C1 from the Russian Patent Office, also available in English). It utilises the above-mentioned tinctures (from Galantus nivalis and Atropa belladonna) which should be taken (10-30 drops Galantus nivalis and 5-15 drops Atropa belladonna) 3-4 times a day before meals for 3-6 months. After a two-week washout period, the course of treatment should be repeated 2-3 times. The application of a magnetic therapy with a copper plate is a natural complementation to these treatment regimens.
In order to obtain the patent, the inventors provided the results from the therapy and follow-up (16 years) of 46 patients (38 female and 8 male subjects). Twenty-four patients suffered from a severe MS, 20-from a mild form of MS, and 2 were at an early stage of the disease. The duration of the treatment was between 6 and 18 months. All patients had a permanent maintenance treatment. Remission was achieved by all patients. No patient was completely cured. The above-mentioned data are based on biochemical results, imaging diagnostics (computed tomography, ultrasound, X-ray, magnetic resonance imaging, etc.), as well as objective and subjective results from the treatment.
Note: Two female patients got pregnant during treatment and gave birth to children who have no MS symptoms! All patients were able to work (with some limitations).
The scientific-practical methodology proposed combining phytotherapy and physiotherapy in MS showed its effectiveness and continuity. The MS treatment related to an intake of medicinal plants proved to be a successful and patient-friendly approach. The intake of phytotherapeutic substances and the concomitant physiotherapy could effectively be combined with the contemporary MS drugs. The existing medical theories and practices, and the phytotherapy and physiotherapeutic schemes are successfully applied as a scientific method for a single and/or combined treatment for MS.
The authors of this article express their willingness to cooperate with medical specialists and scientists all over the world and perform extensive RCTs with MS patients who will be treated with the methods described in this article.
Citation: Kaniskov VL, Iliev IE (2019) Phytotherapy and Physiotherapy in Multiple Sclerosis. J Develop Drugs 8:194.
Received: 04-Jul-2019 Accepted: 19-Jul-2019 Published: 31-Jul-2019
Copyright: © 2019 Kaniskov VL, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.