Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Research Article - (2023)Volume 14, Issue 3
Purpose: To evaluate the use of silicone sphere orbital implants for volume augmentation in management of post-traumatic enophthalmos and enophthalmic socket.
Materials and methods: This was a retrospective interventional case series for evaluation of use of silicone sphere orbital implants for volume augmentation in 14 patients with post-traumatic enophthalmos and enophthalmic socket that were operated in Mansoura Ophthalmic Center from May 2016 to October 2020.
Results: The study included 14 cases with enophthalmos; 9 cases (64.3%) post-traumatic and 5 cases (35.7%) with enophthalmic socket. The median degree of enophthalmos had improved from 4.0 mm (preoperative) to1.0 mm (postoperative). 85.7% of patients were satisfied with the results however, 14.3% were not satisfied. Surgery was not complicated in 78.6% of patients however, 21.4% showed orbital hemorrhage, hypertropia and overcorrection.
Conclusion: The use of silicone sphere orbital implant for volume augmentation in cases of enophthalmos is cheap, easily available and effective.
Post-traumatic enophthalmos; Enophthalmic socket; Orbital implants for enophthalmos; Silicone sphere orbital implants
Enophthalmos may result from orbital blowout fractures and can lead to obvious cosmetic defects. Functional impairment may occur secondary to muscle entrapment leading to diplopia. Early repair of fractures avoids muscle scaring, fat atrophy and disfiguring enophthalmos [1,2].
Post-traumatic enophthalmos is defined as a discrepancy between the orbital volume and its contents that can be altered by many factors; entrapment of the orbital contents at the fracture site, orbital fat necrosis, scaring of the retrobulbar tissue, loss of the eyeball suspension system and increase in orbital volume. However, the most accepted theory is the enlargement of the orbital cavity due to orbital fractures and bone displacement. Generally, a 1 cm3 increase in orbital volume causes 0.8 mm of enophthalmos. Two to three millimeters of enophthalmos is clinically detectable, and more than 5 mm is disfiguring and orbital augmentation is the most appropriate surgery for management of enophthalmos [3-8].
Different materials for volume augmentation had been used, election of the implant either synthetic or autologous are still controversial and depends on many factors including; surgeon’s preference, chosen technique, morbidities of donor site and price and availability of the implant. The ideal material would be one that restores anatomical form and volume, easily placed, with minimal or non-inflammatory reaction and minimal absorption. Titanium meshes, porous polyethylene implants, prolene mesh, med-pore enophthalmos wedge and absorbable plates have been used with a high success rate.
Autogenous implants including fat, cranial bone and cartilage need a second surgery to harvest and carry a risk for the donor site [9].
In this study we apply the use of silicone sphere orbital implants in volume augmentation for cases with post-traumatic enophthalmos and enophthalmic socket as a new application of these implants.
This was a retrospective interventional case series that included 14 cases with enophthalmos; 9 cases with post-traumatic enophthalmos and 5 cases with enophthalmic socket that attended Mansoura Ophthalmic Center from May 2016 to October 2020.
For all cases full ophthalmological examination was done including; history about the cause of trauma, date of trauma, epistaxis, diplopia, loss of sensation on the cheek, fainting and any surgical intervention. Visual acuity testing using Landolt’s broken rings was done, examination of the anterior segment using a slit lamp and posterior segment using an indirect ophthalmoscope was done. Examination of ocular motility in all directions of the gaze to detect any limitations of ocular motility. Detection of enophthalmos was done using Hertel’s exophthalmometer and a difference of 2 mm between both eyes was considered significant. Measurements in cases of enophthalmic socket were taken with the artificial shell in place. Computed Tomography (CT), thin coronal cuts (2 mm-3 mm) were performed for all cases. Axial cuts were also performed to exclude associated medial wall fracture. Entrapment of the inferior rectus or surrounding tissues through the defect in the fracture site was noted. Displacement of orbital walls with subsequent increase in orbital volume was also noted and detection of the orbital implant in enophthalmic socket was detected.
Operative techniques
After getting the ethical approaval from Mansoura Institutional Review Board (IRB), a written consent was obtained from all patients. The study was adherent to the tenets of the Declaration of Helsinki.
All patients were operated under general anesthesia. A sub-ciliary incision was done in all cases for a wide exposure; the periosteum was incised 2 mm below the inferior orbital rim and elevated with a periosteal elevator and reduction of any entrapped contents in the fracture site if present was performed. Silicone sphere orbital implants (FCI Ophthalmics) which are usually used after enucleation and evisceration were divided into two halves so as to have a flat lower surface that lies on the floor of the orbit and a convex upper surface facing the globe or previous implant in cases of enophthalmic socket. The size of the sphere used and the size of the two divided parts depend up on the degree of enophthalmos as shown in Figure1.
Figure 1: Silicone spheres divided into two halves.
Figure 2 show the suitable segment was implanted under the periosteum behind the equator of the globe in order to push the globe or the old implant anteriorly and avoid hypertropia (Figures 1 and 2).
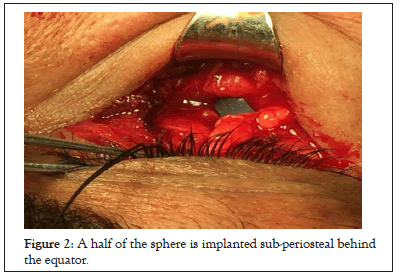
Figure 2: A half of the sphere is implanted sub-periosteal behind the equator.
We measured the degree of enophthalmos after application of the proposed implant using a ruler and observation of both eyes at the head of the patient with the brow as a reference line was done and accordingly as shown in Figures 3A and 3B and Figures 4A-4C, we may implant another part of the sphere or not and we may shave the implanted part to get the suitable size. So, intraoperative assessment of improvement of enophthalmos in comparison to the normal side is the guide for either increasing or decreasing the size of the implant or adding a segment. During implantation in post-traumatic cases (Seeing Eye), we keep an eye on the pupillary reaction as an indicator of optic nerve compression. However, in enophthalmic socket cases we freely push the implant posteriorly. After getting a satisfactory degree of correction of enophthalmos we closed the periosteum with polygalactin 5/0 sutures and the skin with black silk 5/0 sutures (Figures 3A and 3B).
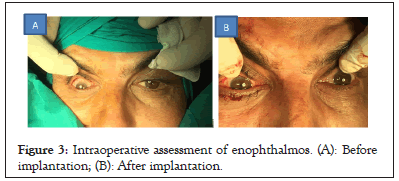
Figure 3: Intraoperative assessment of enophthalmos. (A): Before implantation; (B): After implantation.
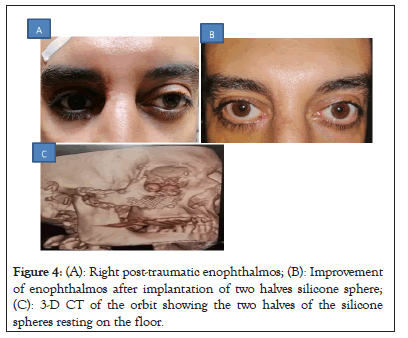
Figure 4: (A): Right post-traumatic enophthalmos; (B): Improvement of enophthalmos after implantation of two halves silicone sphere; (C): 3-D CT of the orbit showing the two halves of the silicone spheres resting on the floor.
Figures 4A-4C in Postoperative systemic antibiotics was used for one week and silk sutures were removed after five days. Cases were followed as regard improvement of enophthalmos and any associated complications for one week, one month, three months and six months after surgery.
Statistical analysis
Data were analyzed using the Statistical Package of Social Science (SPSS) program for Windows (Standard version 21). The normality of data was first tested with Shapiro test. Qualitative data were described using number and percent. Continuous variables were presented as mean ± Standard Deviation (SD) for normally distributed data and median (min-max) for non-normal data. The following tests were used.
Fischer exact test: Compare qualitative variables when expected count less than 5.
Independent t test: Compare quantitative data for two different groups (parametric).
Mann Whitney test: Compare quantitative data for two different groups (non-parametric).
Wilcoxon signed rank test: Compare quantitative data pre and post in the same group (non-parametric).
For all above mentioned statistical tests done, the threshold of significance is fixed at 5% level. The results was considered significant when p ≤ 0.05. The smaller the p-value obtained, the more significant are the results.
This was a retrospective interventional case series that was performed in Mansoura ophthalmic center, Mansoura University, Egypt from May 2016 to October 2020. The study included 14 cases; 9 cases (64.3%) with post-traumatic enophthalmos and 5 cases (35.7%) with enophthalmic socket. They included 12 males (85.7%) and 2 females (14.3%) with Mean age 27.14 ± 10.29 years (Table 1).
| Characteristics | The study group (n=14) |
|---|---|
| Age (Years) | |
| Mean ± SD | 27.14 ± 10.29 |
| Min-Max | 14-45 |
| Sex | |
| Male | 12(85.7%) |
| Female | 2(14.3%) |
| Presentations | |
| Post-traumatic enophthalmos | 9(64.3%) |
| Enopthalmic implant | 5(35.7%) |
| Complications | |
| No | 11(78.6%) |
| Orbital hemorrhage | 1(7.1%) |
| Hypertropia | 1(7.1%) |
| Slight overcorrection | 1(7.1%) |
| Satisfaction | |
| Satisfied | 12(85.7%) |
| Unsatisfied | 2(14.3%) |
Note: SD: Standard Deviation; Min: Minimum; Max: Maximum
Table 1: Patients’ characteristics, presentation, complications and satisfaction.
The median preoperative degree of enophthalmos was 4.0 mm (from 3 mm to 6 mm) and median postoperative degree of enophthalmos was 1.0 mm (from 0 mm to 2 mm) and this difference was statistically significant (p<0.001) (Table 2).
| Degree | Pre-operative degree of enophthalmos (mm) | Post-operative residual enophthalmos (mm) | Wilcoxon signed rank test | P value |
|---|---|---|---|---|
| Median (Min-Max) | 4.0(3-6) | 1(0-2) | 3.35 | 0.001 |
Note: Min: Minimum; Max: Maximum
Table 2: Median degree of enophthalmos.
12 cases (85.7%) were satisfied with the results however, 2 cases (14.3%) were not satisfied. Surgery was not complicated in 11 cases (78.6%) however, 3 cases (21.4%) showed complications in the form of; orbital hemorrhage in 1 case (7.1%), hypertropia in 1 case (7.1%) and overcorrection in 1 case (7.1%) (Figures 5A-5C).
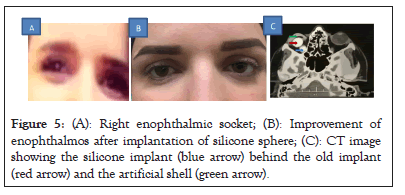
Figure 5: (A): Right enophthalmic socket; (B): Improvement of enophthalmos after implantation of silicone sphere; (C): CT image showing the silicone implant (blue arrow) behind the old implant (red arrow) and the artificial shell (green arrow).
As regard the patient’s satisfaction in relation to their characteristics; males were more satisfied than females (91.7% vs. 50%), patients with enophthalmic socket were more satisfied than those with post-traumatic enophthalmos (100% vs. 77.8%), patients with preoperative enophthalmos ≤ 4.0 mm were more satisfied than those >4.0 mm and patients with residual postoperative enophthalmos ≤ 1.0 mm were more satisfied than those >1.0 mm however, those differences were not statistically significant (Table 3).
| Characteristics | Satisfied (n=12) | Unsatisfied (n=2) | P value |
|---|---|---|---|
| Age (Years) | |||
| Mean ± SD | 27.25 ± 9.83 | 26.50 ± 17.67 | 0.926 |
| Sex | |||
| Male | 11(91.7%) | 1(8.3%) | 0.275 |
| Female | 1(50.0%) | 1(50.0%) | |
| Presentations | |||
| Post-traumatic enophthalmos | 7(77.8%) | 2(22.2%) | 0.505 |
| Enopthalmic implant | 5(100%) | 0(0%) | |
| Complications | |||
| Complicated | 1(33.3%) | 2(66.7%) | 0.033* |
| No complication | 11(100%) | 0(0%) | |
| Pre-operative degree of enophthalmos (mm) | 4 (3-6) | 4.5 (4-5) | 0.847 |
| Post-operative residual enophthalmos (mm) | 1 (0-2) | 1.5 (1-2) | 0.203 |
Note: SD: Standard Deviation; *: p<0.05
Table 3: Association between satisfaction and patients’ characteristics.
Traumatic enophthalmos is usually associated with inferior wall fracture. It was reported that delayed (more than 2 months) management of orbital floor fracture led to inferior outcomes when compared with early intervention. Dulley and Fells noted that 20% of the patients who had surgery within 2 weeks of trauma had enophthalmos while those who underwent surgery 6 months later, the percentage was 72% [10].
Current guidelines in management of traumatic enophthalmos recommended repair of patients with early enophthalmos or hypoglobus and those with fracture involving more than half of the floor as early as possible.
Enophthalmos associated with the anophthalmic socket is probably the most common form of enophthalmos encountered by the oculoplastic surgeons, it results from continuous fat atrophy after evisceration and enucleation and treatment is usually directed toward orbital volume augmentation using autogenous or alloplastic materials [11].
Orbital implants that are used for volume augmentation may are either autogenous (cartilage, bone, dermis fat graft) or alloplastic (med-pore, prolene, titanium mesh) each of these materials has advantages and disadvantages or the choice depends on several factors including; the availability, price and surgeon experience.
In this study we had used the silicone sphere orbital implants that are used for volume replacement after evisceration and enucleation in volume augmentation in traumatic enophthalmos associated with orbital wall fracture and enophthalmic socket.it has the advantages of being easily available, easily fashioned to suite the volume deficit and cheap.
We included 9 patients with traumatic enophthalmos that had orbital floor fracture with enophthalmos more than 2 mm and 5 patients with enophthalmic socket that had previous orbital implant after previous evisceration or enucleation.
The median of enophthalmos had improved from 4.0 mm preoperative to 1.0 mm postoperative. 85.7% of patients were satisfied with the results and 14.3% were not satisfied.
As regard the complications, it was minimal and did not affect the final outcome or affected the visual acuity in seeing eyes. These complications included; one case of orbital hemorrhage, one case of hypertropia and one case of overcorrection in the form of proptosis of 1.0 mm in one of the cases of enophthalmic socket and all complicated cases did not need a second interference.
Our believe is that the concept of management of traumatic enophthalmos include reduction of prolapsed contents into the orbit and covering the defect with an implant to restore nearly the pre-traumatic anatomical condition. However, anatomical alignment using the traditional implants is usually insufficient to treat enophthalmos completely and orbital volume augmentation is usually needed to correct the residual enophthalmos.
Several implants with a wedge shape were used for correction of enophthalmos where the thicker portion is oriented posteriorly behind the equator under the periosteum to produce forward protrusion. However, these implants are not easily available and are expensive. Allen, et al. [11] preferred the use of donor cartilage which is available in donor banks and they used more than one piece until getting a satisfactory protrusion of the globe guided by intraoperative observation.
In this study we have used the idea of Allen, et al. [11] but we implanted the pieces of silicone spheres that are divided into two halves one of them is implanted under the periosteum behind the equator and a second half is used if needed guided by observation of both eyes intra-operative using the brow as a reference line.
Gustavo, et al. [10] in a case report used the titanium mesh with buccal fat graft for correction of late post traumatic enophthalmos. They said that the use of titanium mesh will not completely correct large degrees of enophthalmos and volume augmentation using the buccal fat graft is needed.
Chien-Tzung, et al. [3] reported that one of the complications of repair of orbital floor fracture by restoration of anatomical alignment only is the residual enophthalmos that usually need a second intervention for volume augmentation.
Fouad, et al. [12] reported that traumatic enophthalmos occurs due to either increase of the total orbital volume by the fracture or displacement of fat through fascial ligament lacerations and restoration of orbital volume is mandatory to treat these cases and inadequate management of orbital fractures and restoration of orbital volume leads to periocular fibrosis and affects negatively the operative results.
Zhang, et al. [13] reported the use of computed tomography-based mirroring-reconstruction images of the orbit in 22 patients with late traumatic enophthalmos. They were able to fabricate an adaptive titanium mesh by computer-aided design and computer-aided manufacturing techniques. Application of these implants reduced the trauma induced orbital volume deficit by 65% and corrected 50% of cases of late enophthalmos.
However, Zhang, et al. [13] in spite of being more precise than our technique it needs an advanced more complicated coasty procedure which is not available for all surgeons especially in developing countries.
Valentin, et al. [14] reported a satisfactory cosmetic and functional outcome by using a custom-made Knitted TiNi-based Mesh (KTNM) endograft in management of orbital wall defects with enophthalmos.
Malagon, et al. [15] in a comparative study reported that costo-chondral graft applied to large defects of orbital floor is superior to the combination of two alloplastic materials (titanium mesh+Lactosorb) in restoring orbital volume and correcting enophthalmos with no recurrence or orbital complications.
We think that the use of fashioned silicone spheres in orbital volume augmentation in cases of post-traumatic enophthalmos and enophthalmic socket presents a cheap and easily available alternative to the more advanced manufactured implants especially in developing countries. It is biocompatible, easily fashioned and efficient in restoration of orbital volume and to our knowledge it is the first time to be used for this indication. However, we need more comparative studies on a larger number of patients for evaluation of these implants and we need a more precise way to calculate the needed implant volume preoperatively.
The study was approved by Mansoura IRB.
All participants gave their written consent.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Ghafar El AEA (2023) Piggyback Orbital Implant for Volume Augmentation in Management Post-Traumatic Enophthalmos and Enophthalmic Socket. J Clin Exp Ophthalmol. 14:946.
Received: 01-May-2023, Manuscript No. JCEO-23-22016; Editor assigned: 03-May-2023, Pre QC No. JCEO-23-22016 (PQ); Reviewed: 17-May-2023, QC No. JCEO-23-22016; Revised: 24-May-2023, Manuscript No. JCEO-23-22016 (R); Published: 02-Jun-2023 , DOI: 10.35248/2155-9570.23.14.946
Copyright: © 2023 Ghafar El AEA. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.