Journal of Clinical & Experimental Dermatology Research
Open Access
ISSN: 2155-9554
ISSN: 2155-9554
Case Report - (2024)Volume 15, Issue 4
In the past few years, PRP (Platelet Rich Plasma), as a treatment, became the new shining star. Almost every week there is a new kit appearing on the market (even if they are only copies of 2 generation and outdated) and the number of medical studies published is increasing exponentially. But what is PRP? Why such an interest now? Is it the correct name? And why is it so interesting in dermatology?
Platelet rich plasma; Growth factors; Aging process; Collagen; Elastin
PRP stand for Platelet Rich Plasma. It defines a high concentration of blood platelets in a small volume of plasma. More precisely according to Pr. R. Marx, who published the first study on PRP in the early 90s, platelets concentration should be at least the double of the concentration in the native blood.
So when we spin the blood we obtain 3 different fractions (depending on their weight): The lowest one, at the bottom is composed of the red cells (heavier), then the Platelet Rich Plasma (PRP) and finally the Platelet Poor Plasma (PPP) [1].
But PRP is not a new discovery. In 1953, 2 researchers, Rita Levi- Montalcini and Stanley Cohen discovered the 2 first growth factors in the plasma (epidermal and neural GF) and were subsequently awarded a nobel prize in 1986 by the nobel assembly at the Karolinska institute.
Today, not only we know more than 300 growth factors (PDGFaa, PDGFbb, PDGFab, TGF-b1, TGF-b2, VEGF, EGF just to name a few) and they are all important. So today, we are aware of the very high concentration of growth factors in the plasma, but even more: Stem cells (CD44+, CD90+…) and other factors: Fibrin fibronectin, vitronectin, epinephrine, SDF-1 and SC [2].
Why such an interest now?
More and more patients are asking for natural treatments and nothing can be more natural and safer than the patient's own blood. No risk of allergy, granuloma, asymmetry, no risk of transmitting disease.
Is it the correct name?
When doing research on line (PubMed, Wiley, Google Scholar) we come across different names:
• Platelet leukocyte gel
• Platelet rich plasma gel
• Platelet concentrate
• Plasma rich fibrin
• Blood plasma therapy
The preparations could (and should) differ depending on the indication, but more important are the latest discoveries.
In the study, the effects of activated Platelet-Rich Plasma (aPRP) and activated Platelet-Poor Plasma (aPPP) have been investigated on the remodelling of the extracellular matrix, a process that requires activation of dermal fibroblasts, which is essential for rejuvenation of aged skin. aPRP and aPPP both stimulated cell proliferation, with peak proliferation occurring in cells grown in 5% aPRP. Levels of PIP were highest in cells grown in the presence of 5% aPRP. Additionally, aPRP and aPPP increased the expression of type I collagen, MMP-1 protein and mRNA in human dermal fibroblasts.
Platelet-rich plasma (PRP) has been established as an autologous source for therapeutic angiogenesis. The purpose of this study was to evaluate PRP angiogenic effects compared to Platelet-Poor Plasma (PPP) in vitro and in vivo. The effects of PRP on Vascular Endothelial Growth Factor Receptor-2 (VEGFR2) and CD34 expression were evaluated using real-time PCR, flow cytometry, western blot, immunocytochemistry and pathological study, as were carried out in both human umbilical endothelial cell culture and rat skin. Our findings indicated significant effect of PRP and PPP on VEGFR2 and CD34 expression by human umbilical vein endothelial cells, which was greater in latter. These effects, however, were confirmed by demonstrating an earlier angiogenic effect of PPP in vivo when compared to PRP [3].
So obviously the term PRP is wrong and we should be using the whole of the plasma (PRP and PPP).
What is the aging process on the face?
• Damages in dermis and epidermis layers
• Decrease in collagen and elastin
• Disappearance of skin fatty layers
• Damages to the extra cellular matrix which lead to changes in:
Skin texture, firmness, radiance, volume, flexibility, hydration
and wrinkles formation
In order to completely understand the skin we must understand the extra cellular matrix. The extra cellular matrix is what is found between cells, holding them together and helping their correct functions. Rather than being made up of tightly packed cells, living tissues also contain extracellular space and this space is filled with the extra cellular matrix [4].
This cellular matrix is constantly changing, evolving and beside being found in all tissues it provides the necessary structural scaffolding for the cells. And active component of all living tissues. As well as providing structural support for the cells that are embedded within a tissue. It is mandatory for the cell’s correct mitosis, growth and functioning. So put simply, the extra cellular matrix is responsible for how a tissue both looks and functions.
What is the ECM made of? Water, minerals, fibrous proteins and proteoglycans. The last one is a specific form of protein surrounded by 2 long starch like chains of molecules: Glycos-amininoglycans. All ECM and it’s specific components are manufactured and organised by the cells where they live. In regard of the skin, the fibroblasts are responsible for the ECM, but not in a finished form. T is more a “precursor”. The fibroblasts will be in charge of their incorporation into the ECM based on each tissue particular need at a specific time.
Other fibrous proteins can be found in the ECM. That includes collagen, elastin, fibronectin and laminin. Depending on which tissue they are found it will be in different amounts. These proteins are produced by fibroblasts, but not in their finished form. They're released as ‘precursor' molecules; their subsequent incorporation into the extracellular matrix is guided by the fibroblasts in accordance with the functional needs of a particular tissue [5].
Collagen is a stretch resistant fibre, very strong and it provides strength and tensile effect. Not only that but it is also the number 1 protein in the body. It provides support for the skin but is also the main part of tendons and ligaments. Like when a rubber band is pulled and released, elastin permits tissues to return to their original state after being pulled. Ultra Violet (UV) light can impair the quality of elastin fibres as well as their reconstruction. That is why skin overexposed to sunlight is damaged.
Fibroblasts are also responsible for fibronectin but originally released in a water soluble form they will quickly be re-organised into an insoluble mesh. One of its function is to place cells in their correct position in the ECM. Laminin, not as well known, is a sheet like network that acts like glue between dissimilar tissue. Also a protein it is essential for membranes wherever connective tissue is in contact with muscle, nervous, or epithelial tissue [6].
The ageing process is a complex interaction between varieties of facial elements, which occurs like a domino effect. The process can be described as a cascade effect, which happens in four main facial layers: Bone, muscle, fat and skin. One of the most important and obvious change happens in the deepest layers at bone level where the facial apertures increase by 20% as we get older. As well as the mandibula which is thinning (Figure 1).
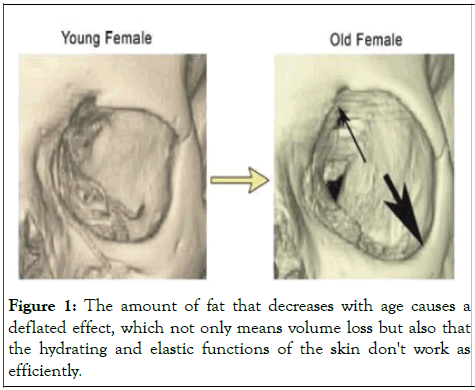
Figure 1: The amount of fat that decreases with age causes a deflated effect, which not only means volume loss but also that the hydrating and elastic functions of the skin don't work as efficiently.
Above the muscles, the amount of fat that decreases with age causes a deflated effect, which not only means volume loss but also that the hydrating and elastic functions of the skin don't work as efficiently. The fibroblast cells in the skin that produce elastin, collagen and Hyaluronic Acid (HA) work best when they are under a degree of stretch. When the fat depletes, this stretch is lessened and the skin is not functioning as well, which causes it to sag [7].
In 2015, I conducted a study over 338 patients (none of them were asked to come for more treatments), but we can see the number of sessions per patient double each time, therefore objective proof of the efficacy of the treatment. Cho, et al. found that the appearance of wrinkles in the PRP injected group in their study were significantly reduced and dermal thickness was improved. Dr S. Zencker conducted interesting investigations into the impact of PRP on dermal augmentation. She found that dermal intensities increased following treatment using meso-and filling methodologies for full facial rejuvenation to objectively evaluate the effects of three PRFM treatments spaced one month apart, then analysed the effects of superficial dermal stimulation and augmentation using 20 MHz ultrasound measurements. Treatments were administered to the nasolabial folds, tear troughs and cheeks, with significant preliminary results in skin thickness and neo collagenesis after only one treatment.
She also assessed hyper vascularisation in patients following treatment with PRP/PRFM. In this instance, Confocal Laser Microscopy (CLM) was used to assess the results, comprising a laser beam in the near infrared range with a lens system and bean splitter on the area of the skin to be examined. Light is reflected by the different components of the tissue and captured by the microscope to generate an image. The patient received one PRFM treatment using the meso technique (i.e., micro papular intradermal injections) to the marionette line and was analysed with CLM immediately after treatment. Blood flow is immediately increased, resulting in the hyper vascularisation of the injected dermal tissue, which in turn increases blood supply and consecutively the supply of growth factors [8].
Growth factors from the plasma are important to improve vascularisation, to stimulate the fibroblasts, increase the dermal/ epidermal layer, improve the pigmentation, to reduce or stop the bone resorption and to maintain the fat in the right compartments. All in one safe and natural treatment, but there are other indications for skin.
It is common knowledge that the wound healing and regeneration starts with the clot formation which is also due to platelet degranulation. The subsequent events will be the release of a multitude of chemical messengers (cytokines and chemokines) and coagulation factors.
As of today (and knowledge is increasing) we know over 300 of those factors within the platelets. Just to name a few: Platelet Derived Growth Factors (PDGFs), Transforming Growth Factors (TGFs), Vascular Endothelial Growth Factor (VEGF) (EGF) and Insulin-like Growth Factor, Epidermal Growth Factor (IGF). They are all known to improve cell’s multiplication and migration as well as generating neo angiogenesis. That explains the process of wound healing (Figures 2-5).
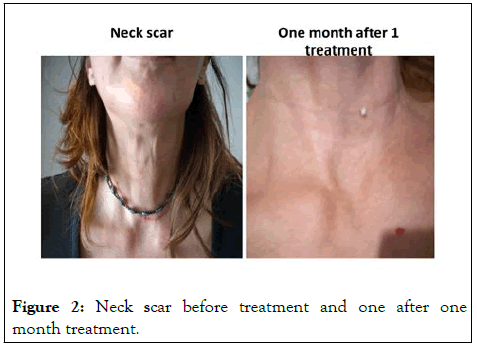
Figure 2: Neck scar before treatment and one after one month treatment.
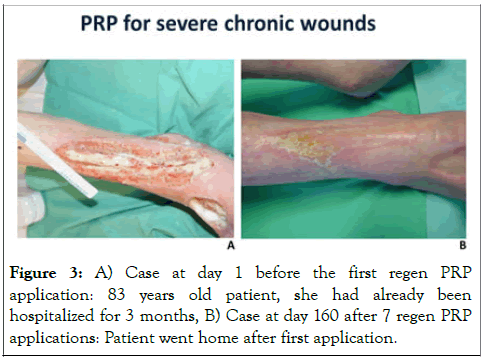
Figure 3: A) Case at day 1 before the first regen PRP application: 83 years old patient, she had already been hospitalized for 3 months, B) Case at day 160 after 7 regen PRP applications: Patient went home after first application.
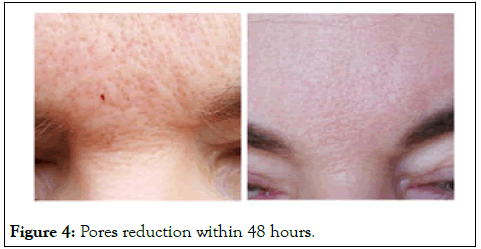
Figure 4: Pores reduction within 48 hours.

Figure 5: Pigmentation reduction after 1 treatment.
Vitiligo is a chronic medical skin condition where white patches will appears and develop on the skin because there is a lack of melanin. That chemical is normally produced by specific and specialised cells, melanocytes. They are responsible for the skin colour (normal pigment) and the protection from the sun. The cause of vitiligo is not yet fully known but many think that it is a disease in which the body makes antibodies to its own melanocytes and in doing so destroys them.
Even though it can affect any area of the skin, The lack of melanocytes and subsequently protection against the sun explains why it appears more often on sun exposed areas like face, neck and hands. published at the end of 2015 their study over 60 patients with stable vitiligo with overall symmetrical lesions. Each patient had the left side treated with NB-UV alone (control side) while the right side was treated with NB-UVB plus intradermal PRP injections every 2 weeks for 4 months. The results showed a highly statistically improvement in the re- pigmentation in the combination group compared to the NBUVB alone. And they concluded that PRP injections in combination with NB-UVB were a simple, safe and tolerable technique for vitiligo treatment. It shortens the duration of NBUVB therapy and increase patient compliance. But now, we also have fantastic results with CO2 laser and PRP (Figure 6).
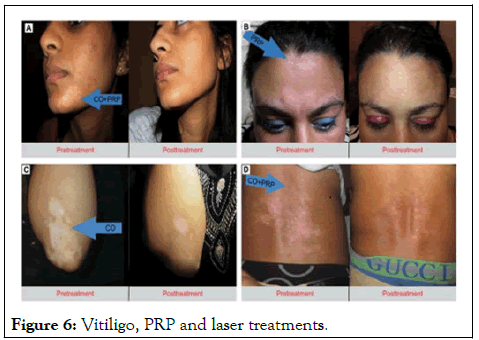
Figure 6: Vitiligo, PRP and laser treatments.
Rosacea is another skin condition extremely difficult to treat and control, but plasma and growth factors give excellent results (Figure 7).

Figure 7: Rosacea.
Plasma treatment for hair. Uebel, et al. have shown that storing hair grafts in PRP can enhance graft survival, improve hair density and stimulate growth of transplanted follicular units. Following this published their results on the use of PRP as a potential therapeutic tool for promoting hair growth. Takikawa proved that PRP improved the density of hair by 165 at 12 weeks and wrote: “Activated PRP increased the proliferation of DP (Dermal Papilla) cells and stimulated Extracellular Signal- Regulated Kinase (ERK) and Akt signalling. Giordano S, et al. conducted a meta analysis on evidence of platelet-rich plasma for androgenetic alopecia by comparing local injection of PRP versus control to investigate the efficacy of local PRP injections in AGA (Figure 8).

Figure 8: Hair before and after PRP treatment.
The PRP injections in combination with NB-UVB were a simple, safe and tolerable technique for vitiligo treatment. It shortens the duration of NB-UVB therapy and increase patient compliance. A single treatment of platelet-rich stroma injected in the scalp of patients with AGA significantly increased hair density within 6 weeks to 12 weeks. Local injection of PRP for androgenic alopecia might be associated with an increased number of hairs in the treated areas with minimal morbidity.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Sister D (2024) Platelet's Growth Factors and their Interest in Dermatology. J Clin Exp Dermatol Res. 15:667.
Received: 07-Jan-2020, Manuscript No. JCEDR-24-3070; Editor assigned: 10-Jan-2020, Pre QC No. JCEDR-24-3070 (PQ); Reviewed: 24-Jan-2020, QC No. JCEDR-24-3070; Revised: 29-May-2024, Manuscript No. JCEDR-24-3070 (R); Published: 26-Jun-2024 , DOI: 10.35841/2329-9509.23.15.667
Copyright: © 2024 Sister D. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.