
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Case Report - (2024)Volume 15, Issue 5
Pneumomediastinum and pneumopericardium is defined as the presence of free air in the mediastinum structures and pericardial sac. It is an uncommon condition which requires early recognition to prevent mortality and morbidity associated with it. A 9 year old male, having history of left non-palpable undescended testis since birth was admitted in dept. Patient had history of URTI 1 week ago. We are describing a patient with pneumomediastinum and pneumopericardium and bilateral subcutaneous emphysema associated with post intubation and positive pressure ventilation.
Pneumomediastinum; Pneumopericardium; Perivascular connective tissue; Mediastinum
Pneumomediastinum and pneumopericardium is defined as the presence of free air in the mediastinum structures and pericardial sac. It is an uncommon condition which requires early recognition to prevent mortality and morbidity associated with it. It mainly results from sudden increase in intra-alveolar pressures leading to rupture of perivasucular alveoli. In such conditions, air escapes into perivascular connective tissue with subsequent dissection into the mediastinum. Tension pneumothorax which subsequently causes pneumomediastinum and pneumopericardium post intubation and resulted from positive pressure ventilation are very rare condition. In this case report, we are describing a patient with pneumomediastinum and pneumopericardium and bilateral subcutaneous emphysema associated with post intubation and positive pressure ventilation [1-3].
A 9 year old male, having history of left non-palpable undescended testis since birth was admitted in dept. Of paediatric surgery and was planned for orchidopexy. On preanesthetic check up which was performed one day before surgery, patient’s general condition was good. His body weight was 40 kg with satble vitals [4]. Patient had history of URTI 1 week ago.
But at the time of pre-anesthetic check up there were no symptoms of active URTI and on auscultation chest was clear with equal air entry bilaterally with no added sounds. Patient had normal physical examination without any associated comorbidities [5].
Patient was kept NPO according to standard fasting guidelines. On the day of surgery, all standard monitors (ECG, NIBP and SpO2) were attached. After obtaining intravenous access with 20 gauge iv. cannula, ringer lactate was commenced and premedication was done with midazolam 0.05 mg/kg. His baseline vitals were HR-80/min, BP-130/70 mm Hg (MAP-70 mm Hg) and SpO2-98% on room air. Preoxygenation was started with 100% O2 for 3 minutes. Patient was induced with inj. fentanyl 80 μg, inj. Propofol 80 mg and after the ability to ventilate the lungs using face mask was confirmed inj. Vecuronium 4 mg was administered and trachea was intubated with ETT 5.5 mm ID placed and airway secured. Intermittent positive pressure ventilation was commenced, delivering oxygen and N2O using tidal volume of 250 ml at a frequency of 14 breaths per minute. No PEEP was administered. After ten minutes of induction, SpO2 had decreased from 98% to 90% and there was increase in HR, RR and airway pressures. Patient was taken on 100% oxygen and the position of ETT was again confirmed by inspecting the capnogram and auscultation in both axilla [6].
There was decrease air entry on right hemithorax and SpO2 falls to 60% and HR decreased to 50/min. Injection atropine 0.6 mg was administered and HR came to 90/min but airway pressures were very high with persistent decreased air entry in right hemithorax and subcutaneous emphysema. Tentative diagnosis of tension pneumothorax was made and needle thoracotomy using 16 gauge needle was performed in 5th ICS in midclavicular line. Gush of air was released and HR increased to 120/min and SpO2 also increased to 95% but BP was 80/40 mm Hg for which patient was taken on infusion adrenaline @2 ml/hr. Surgery was postponed and patient shifted to intensive care unit for ventilator support and further management. Patient was ventilated with SIMV/PS mode of ventilation with tidal volume of 300 ml pressure support 10 and at the frequency of 16 and central venous access was secured in right intenaljugular vein. After blood culture, broad spectrum antibiotics were started. Laboratory exams on admission were unremarkable. A 12 lead electrocardiogram showed sinus rhythm. The chest x-ray showed lucent streaks of gas that outlined mediastinal structures and subcutaneous emphysema in the area of both sides of axilla and neck. Ultrasonography of thorax and abdomen was performed which revealed air pockets in mediastinum and pericardium. 2D echocardiography was also performed which also revealed pneumopericardium and pneumomediastinum in posterior part of heart. Computed tomography was performed which confirmed the diagnosis without any other findings (Figure 1) [7,8].
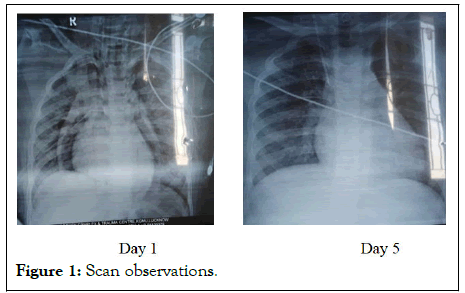
Figure 1: Scan observations.
The patient was managed conservatively with analgesia (acetaminophen) and a course of prophylactic antibiotics. There was spontaneous resolution of pneumomediastinum and pneumopericardium on chest x-ray. Patient was taken off from all vasopressors slowly and was extubated on third day and kept on nasal prongs and on fifth day asymptomatic patient was discharged. He was absolutely normal on follow up examination.
Pneumomediastinum and pneumopericardium following positive pressure ventilation are well described even they are rare and poorly recognized phenomena. The incidence rate is extremely low. Pneumomediastinum is rare and generally benign self limited condition first reported in literature in 1939 by Hamman. Pneumpericardium can be a complication of pneumothorax and pneumomediastinum and is defined as air or gas in pericardial cavity and was first described by Brischeteau in 18443.
Cardiac tamponade is dreadful complication of pneumpericardium which can increases mortality by 58%. Pneumomediastinum and pneumopericardium is very rare but can happen after positive pressure ventilation especially in paediatric patients. Positive pressure ventilation raise intrathoracic pressure which subsequently leads to raise intrabronchial pressure. There is a site of potential weakness where the parietal pericardium is reflected on to visceral pericardium ear the ostia of pulmonary veins. The pericardial collagenous tissue is not continuous around the point of reflection but tends to pass peripherally, contributing to the perivascular sheath. Air could enter the pericardial sac with relative ease at the site of reflection [9].
An association of pneumomediatinum, pneumopericardium and pneumothorax with subcutaneous emphysema is extremely rare in children. In our case, all of the three (pneumomediastinum, pneumopericardium and pneumothorax with subcutaneous emphysema) were present. These pathological changes could resolved spontaneously but sometimes it may cause cardiac tamponade and cardiac herniation which eventually leads to significant cardiac dysfunction.
Patient should be managed in intensive cardiopulmonary monitoring. Rule out any associated complications. Uncomplicated pneumomediastinum can be managed conservatively with analgesia, prophylactic antibiotics and avoidance of maneuvers that increase pulmonary pressures. We managed our patient by giving symptomatic treatment and was kept on mechanical ventilation for three days only discharged on fifth day [10].
Pneumomediastinum, pneumopericardium is rare and generally benign condition. Chest x-ray is usually sufficient to diagnose this condition but patient should be monitored carefully for any complications. Treatment comprises of displacing the trigger, rest and administration of oxygen, antibiotics. In extreme cases chest tube can be placed.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Rawat J (2024) Positive Pressure Ventilation Related Pneumopericardium and Pneumomediastinum- A Case Report. J Anesth Clin Res. 15:1151.
Received: 17-Jun-2020, Manuscript No. JACR-24-4983; Editor assigned: 22-Jun-2020, Pre QC No. JACR-24-4983 (PQ); Reviewed: 06-Jul-2020, QC No. JACR-24-4983; Revised: 03-Jun-2024, Manuscript No. JACR-24-4983 (R); Published: 28-Oct-2024 , DOI: 10.35248/2155-6148.24.15.1163
Copyright: © 2024 Rawat J. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.