Journal of Women's Health Care
Open Access
ISSN: 2167-0420
ISSN: 2167-0420
Review Article - (2024)Volume 13, Issue 1
Objectives: To determine the frequency of post-natal consultation (PNC) and the socio-demographic and clinical characteristics of women giving birth, to assess the content of PNC in relation to recommended standards and to evaluate maternal and neonatal prognosis.
Patients and methods: This was a retrospective, descriptive and analytical study conducted over a period of 6 months (1 September 2020 and 29 February 2021) and focused on postnatal consultations at the hospital's Department of Gynaecology and Obstetrics (IHS). We studied patients' socio-demographic characteristics, antenatal follow-up data, and mode of delivery, immediate postpartum surveillance and postnatal follow-up data. Data were entered and analyzed using Excel 2010 and Epi info 7.2 software. We conducted 2324 postnatal consultations in 1134 deliveries, i.e. a coverage rate of 68.3% and an average of 2 PNC per patient. All patients had received PNC 1, 68.7% PNC 2 and 36.1% PNC. Only 396 (34.9%) patients had completed all three consultations. The average age of the women in our series was 27 years. The majority of patients lived in the Dakar department (70.55%). Primiparous women were in the majority (39%). Most patients had given birth vaginally (68.9%). Parameters such as blood pressure, pulse, vulvar bleeding and uterine globe were monitored in ¾ of patients. The average length of hospital stay for vaginal deliveries was 24 hours, and 72 hours for caesarean deliveries. Midwives performed 1056 PNC (45.4%) and obstetricians 1268 PNC (54.6%). PNC parameters were assessed in most patients, with the exception of weight, which was assessed in only 1.9% of patients in PNC 1, 27.4% in PNC 2 and 39% in PNC 3. Also in PNC 3, no patient had a speculum examination with VIA/VILI or a cervico-uterine smear. In newborns, measurements were often neglected during PNC 2 (2.1% of cases) and PNC 1 (1.5% of cases), as was the neurological examination (1.5% in PNC 2 and 15.8% in PNC 3. Exclusive breastfeeding was practiced in 78% of cases, while the remainder of the sample (22%) was mixed breastfeeding. 30.5% of patients had benefited from post-partum family planning. These were mainly caesarean patients (76.3%). The progestin-only implant was the most frequently chosen method (73.3%). Post-partum complications accounted for 10.9% of deliveries. High blood pressure was the most common, accounting for 59.6% of complications, followed by post-partum haemorrhage, which accounted for 27.4% of complications and 1.5% of deliveries. We recorded 1103 live births (94.5%), 33 fresh stillbirths (2.8%) and 31 macerated stillbirths (2.6%). One hundred and forty-three newborns (13%) had presented complications. Asphyxia (4.3%) and neonatal infections (4%) were the most frequent complications. Compliance with PNC was higher in patients who had given birth by caesarean section (p<0.01) and those who had performed 4 or more ANC (p<0.01).
Conclusion: PNC coverage could be improved among patients who gave birth at the IHS maternity unit, despite the acceptable rate we recorded. This will require raising the awareness of all those involved in maternal and neonatal care.
Postnatal consultation, Contraception, Breastfeeding, Vaccinations, Complication
The post-partum period is one of psychological and physical upheaval for the mother. It can be fraught with maternal and neonatal complications. Two-thirds of maternal and neonatal deaths occur during this period, particularly in the first 24 hours after delivery [1, 2]. These deaths are most often due to haemorrhagic complications such as immediate post-partum haemorrhage, which is the leading cause of maternal mortality worldwide. The concept of post-natal consultations emerged in the 90s with the aim of reducing maternal and neonatal morbidity and mortality [3]. The WHO recommends three visits in the post-partum period: the first within 24 hours of delivery, the second between the 9th and 16th day post-partum and the last at 6 weeks [4]. For various reasons, these recommendations are not always followed in developing countries, particularly in Senegal, where in 2013, in the Dakar region; only 19% of women who gave birth received three postnatal consultations (PNC) [5]. Given these observations, we decided to conduct this study, the general objective of which was to carry out a situational analysis of our practice in terms of postnatal consultations.
The general aim of the study was to carry out a situational analysis of our post-natal consultation practice. To do this, we specified the frequency with which PNC were carried out and the sociodemographic and clinical characteristics of the women who gave birth, assessed the content of PNC in relation to the recommended standards, and evaluated the maternal and neonatal prognosis.
We conducted a retrospective, descriptive and analytical study over a 6-month period from 1 September 2020 to 29 February 2021. Our study population consisted of patients who gave birth at the IHS maternity unit during the study period. We included in the study all women who had their postnatal consultations at the maternity ward of the Institut d'Hygiène Sociale de Dakar hospital during the study period. We did not include patients who had given birth in another facility and who had come for post-natal follow-up.
All patients who gave birth at the maternity unit were recruited. Data were collected from delivery records and the post-natal consultation register. Data were analyzed using Excel 2010 software. Qualitative variables were described in terms of number and frequency, and quantitative variables in terms of mean, standard deviation and extremes. For the analytical part of our study, the chi-square test was used to compare proportions and the difference was statistically significant when the p-value was less than 0.05.
Descriptive Results
Frequency
During the study period, we performed 2324 PNC out of the 3402 expected, i.e. a coverage rate of 68.3% and an average of 2 PNC per patient. PNC 1 was performed in all patients (100%), PNC 2 and PNC 3 were performed in 68.7% and 36.1% of expected patients respectively.
Age
The average age of the patients was 27 years, with extremes of 14 and 46 years.
The 20-30 age group was the most represented (53.1%) [Table 1].
| Age range | Number | Frequency (%) |
|---|---|---|
| Under 20 | 133 | 11,7 |
| 20-29 years old | 602 | 53,1 |
| 30-39 years old | 351 | 31 |
| ≥ 40 years | 48 | 4,2 |
| Total | 1134 | 100 |
Table 1: Age distribution of patients who underwent PNC at the maternity ward of the IHS hospital in Dakar between 1 September 2020 and 29 February 2021 (N=1134)
Address
The majority of patients resided in the department of Dakar (70.55%) and Pikine (16.5%) [Figure 1].
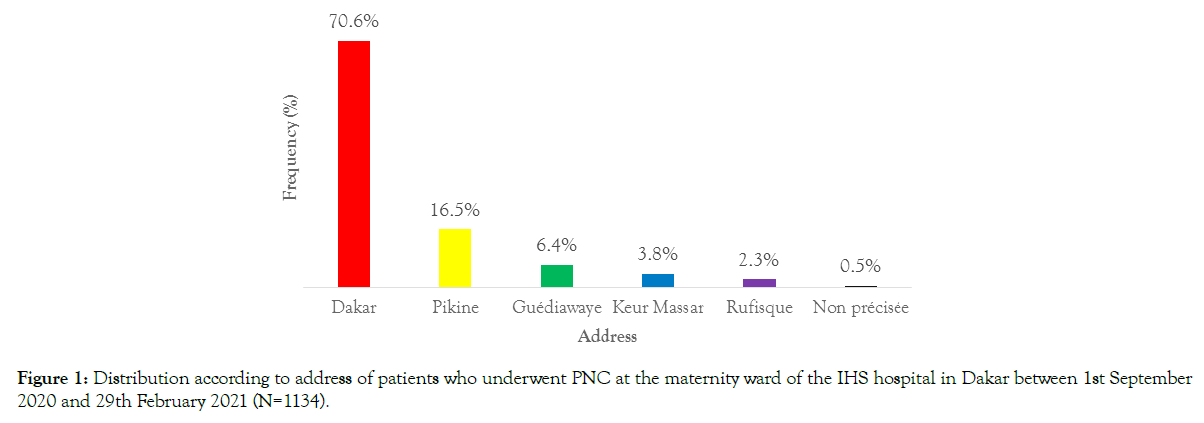
Figure 1. Distribution according to address of patients who underwent PNC at the maternity ward of the IHS hospital in Dakar between 1st September 2020 and 29th February 2021 (N=1134).
Marital status
Most patients were married (98.8%). We recorded 13 single patients (1.1%).
Profession
Occupation was recorded for 209 patients (18%). Of these, 136 were housewives (12%), 57 students (5%) and 16 pupils (1.4%), and 81.1% were unspecified.
History
Gestate
In our study, the average gestational age was 3, with extremes of 1 and 8. Primigravida were in the majority (39%) [Figure 2].
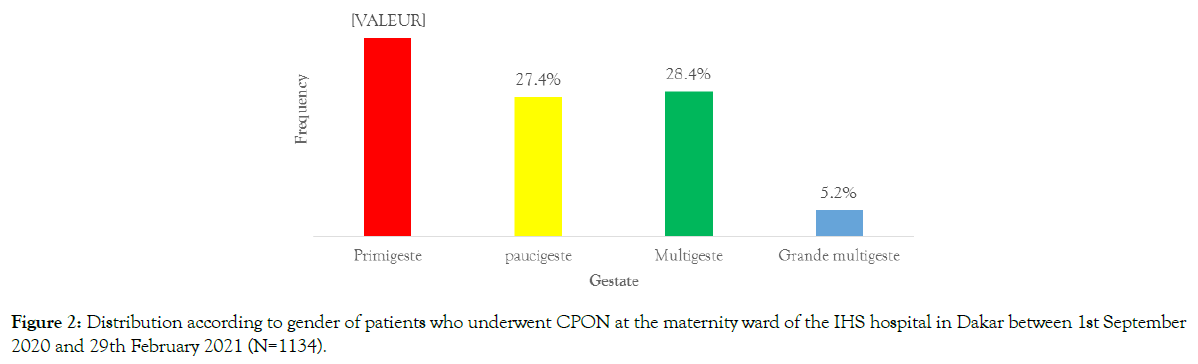
Figure 2. Distribution according to gender of patients who underwent CPON at the maternity ward of the IHS hospital in Dakar between 1st September 2020 and 29th February 2021 (N=1134).
Parity
In our series, primiparous women were the most represented (47.9%), followed by multiparous women (27.6%) and pauciparous women (21.8%) [Figure 3].
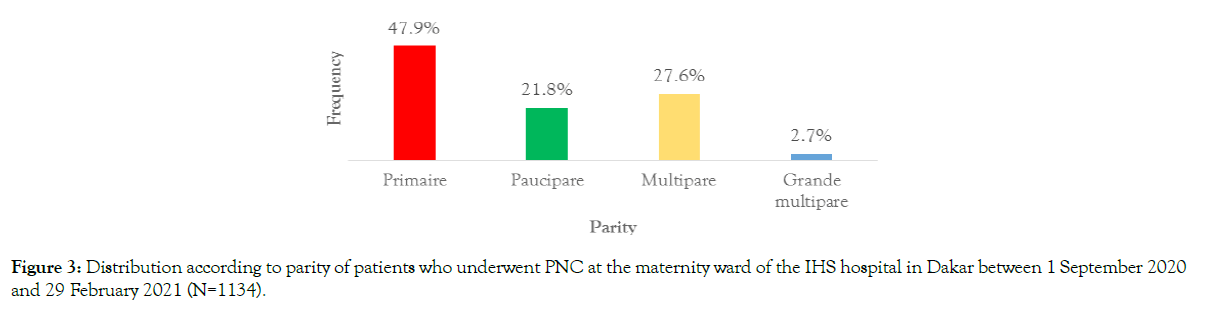
Figure 3. Distribution according to parity of patients who underwent PNC at the maternity ward of the IHS hospital in Dakar between 1 September 2020 and 29 February 2021 (N=1134).
In our series, 24 patients (2.1%) had a medical history. These were mostly cases of chronic hypertension (0.6%) and diabetes (0.6%).
Surgical history was noted in 111 patients (9.8%). These were cases of caesarean section (9.4%), myomectomy (0.2%) and appendectomy (0.2%).
Antenatal, delivery and post-partum monitoring data
Antenatal follow-up data
In our study, 782 patients (69%) had undergone at least 4 ANC. A total of 352 (31%) had undergone less than 4 ANC.
Pregnancy monitoring was carried out in most patients by a state midwife (88.3%) and the remainder by obstetricians.
Pathologies encountered during follow-up
In our series, 633 patients (55.8%) had presented with at least one pathology during pregnancy. Moderate anaemia was most common in 456 cases (40.2%) [Table 2].
| Pathology during pregnancy | Number | Frequency (%) |
|---|---|---|
| No pathology | 501 | 44,2 |
| Severe pre-eclampsia | 32 | 2,8 |
| Moderate anaemia | 456 | 40,2 |
| Severe anaemia | 5 | 0,4 |
| Hydramnios | 10 | 0,9 |
| Oligohydramnios | 20 | 1,8 |
| Gestational hypertension | 21 | 1,9 |
| Excessive uterine height | 26 | 2,3 |
| Infectious syndrome | 12 | 1,1 |
| Gestational diabetes | 51 | 4,5 |
| Total | 1134 | 100 |
Table 2: Distribution according to pathologies found during pregnancy in patients who underwent PNC at the maternity ward of the IHS hospital in Dakar between 1st September 2020 and 29th February 2021 (N=1134)
Delivery data
Most patients had a vaginal delivery (68.9%). Caesarean sections were performed on 352 pregnant women (31.1%). Among those who had given birth vaginally, there were 206 episiotomies (26.3%), 98 perineal tears (12.5%) and 48 abrasions (6.13%) [Table 3].
| Perineal lesions | Number | Frequency (%) |
|---|---|---|
| None | 430 | 55,1 |
| Episiotomy | 206 | 26,3 |
| Perineal tear | 98 | 12,5 |
| Scrape | 48 | 6,1 |
| Total | 782 | 100 |
Table 3: Distribution according to the existence of perineal lesions of patients who underwent CPON at the maternity ward of the IHS hospital in Dakar between 1st September 2020 and 29th February 2021 (N=1134)
Post-partum monitoring data
During the first two hours after delivery, 872 patients (76.9%) had regular documented monitoring. The most frequently monitored parameters were blood pressure (83.7%), pulse (83.6%) and lochia (72.9%) [Table 4].
| Monitoring parameter | Vaginal delivery | Caesarean section | Total |
|---|---|---|---|
| Pulse | 377(72.5%) | 352(100%) | 729 (83.6%) |
| Temperature | 324(62.3%) | 352(100%) | 676 (77.5%) |
| Blood pressure | 378(72.6%) | 352(100%) | 730 (83.7%) |
| Uterine retraction | 371(71.3%) | 263(74, 7%) | 634 (72.7%) |
| Lochia | 371(71.3%) | 265(75, 3%) | 636 (72. 9%) |
| Diuresis | 6(1.1%) | 350(99,4) | 356 (40.8%) |
Table 4: Distribution according to completeness of immediate postpartum monitoring parameters in patients who underwent PNC at the maternity ward of the IHS hospital in Dakar between 1st September 2020 and 29th February 2021 (N=872)
The average length of hospital stay after vaginal delivery was 24 hours. For caesarean patients, this was 72 hours [Table 5].
| Number of days in hospital | Vaginal delivery | Caesarean section |
|---|---|---|
| [24 to 48 hours | 743(95, 1%) | 0(0%) |
| [48 to 120 hours | 38(4, 8%) | 346(98, 2%) |
| >120 hours | 1(0, 1%) | 6(1, 7%) |
| Total | 782(100%) | 352(100%) |
Table 5: Distribution according to the number of days of hospitalisation for patients who underwent PNC at the IHS maternity hospital in Dakar between 1st September 2020 and 29th February 2021 (N=1134)
Neonatal data
We recorded 1103 live births (94.5%), 33 fresh stillbirths (2.8%) and 31 macerated stillbirths (2.6%). The Apgar score at five minutes was mostly normal (90.1%) [Table 6].
| Apgar score at five minutes | Number | Frequency (%) |
|---|---|---|
| ≤ 3 | 64 | 5,5 |
| 4-6 | 51 | 4,3 |
| 7-10 | 1052 | 90,1 |
| Total | 1167 | 100 |
Table 6: Distribution according to Apgar score at the fifth minute of newborns born to mothers who underwent PNC at the maternity unit of the IHS hospital in Dakar between 1st September 2020 and 29th February 2021 (N=1167)
In our series, most newborns weighed between 2500 and 3999 (81.1%). Hypotrophic and macrosomic babies accounted for 16.2% and 2.7% respectively [Table 7].
| Weight in grams | Number | Frequency (%) |
|---|---|---|
| <2500 | 189 | 16,2 |
| 2500 a 3999 | 946 | 81,1 |
| ≥4000 | 29 | 2,7 |
| Total | 1167 | 100 |
Table 7: Distribution according to birth weight of newborns born to mothers who underwent CPON at the maternity unit of the IHS hospital in Dakar between 1 September 2020 and 29 February 2021 (N=1167)
In our series, all newborns received vaccinations and essential care.
Post-natal consultation (PNC)
Rank of PNC
In our study, the 2324 PNC performed were distributed as follows: 1134 PNC 1 (48.8%), 780 PNC 2 (33.6%), and 410 PNC 3 (17.6%) [Figure 4].
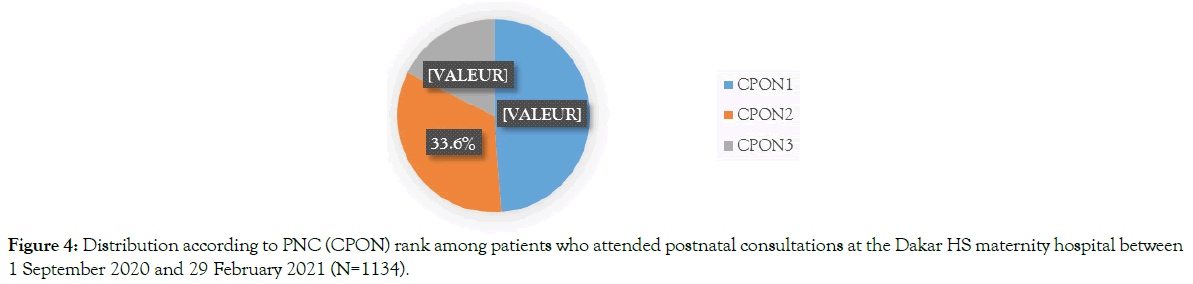
Figure 4. Distribution according to PNC (CPON) rank among patients who attended postnatal consultations at the Dakar HS maternity hospital between 1 September 2020 and 29 February 2021 (N=1134).
Provider qualification
Midwives carried out 1056 PNC (45.4%). These were exclusively vaginal deliveries. Gynaecologists-obstetricians performed 1268 PNC (54.6%), including 464 (30.5%) for women with vaginal deliveries [Table 8].
| PNC | Midwives | Gynaecologists-obstetricians | ||
|---|---|---|---|---|
| Vaginal delivery | Caesarean section | Vaginal delivery | Caesarean section | |
| PNC1 | 323(41, 3%) | - | 459(58, 7%) | 352(100%) |
| PNC2 | 507(99%) | - | 5(1%) | 268(100%) |
| PNC3 | 226(100%) | - | - | 184(100%) |
| Total | 1056(69, 4%) | - | 464(30, 5%) | 804(100%) |
Table 8: Distribution according to the qualification of the provider in charge of PNC of patients in the maternity ward of the IHS hospital in Dakar between 1st September 2020 and 29th February 2021 (N=1134)
PNC Parameters
Maternal parameters
During PNC, the general examination parameters were generally well assessed, with the exception of weight and height. During PNC 1, 2 and 3, weight was reported in 1.9%, 25.4% and 39% of patients respectively. However, height was only sought in 12% of cases at PCN 1 [Table 9].
| Parameters | PNC1 | PNC2 | PNC3 |
|---|---|---|---|
| General condition | 1134(100%) | 780(100%) | 410(100%) |
| Blood pressure | 1134(100%) | 771(98, 8%) | 404(98, 5%) |
| Temperature | 1134(100%) | 748(95, 9%) | 384(93, 6%) |
| Pulse | 1134(100%) | 769(98, 5%) | 398(97%) |
| Weight | 22(1, 9%) | 214(27, 4%) | 160(39%) |
| Height | 12(1%) | - | - |
| Examination of calves | 1133(99, 9%) | 231(29,6) | 161(39, 2%) |
| Conjunctival mucous membranes | 1134(100%) | 777(99, 6%) | 410(100%) |
| Check for oedema | 1134(100%) | 777(99, 6%) | 410(100%) |
Table 9: Distribution according to completeness of PNC parameters (general examination) in patients who underwent their post-natal consultation at the maternity ward of the IHS hospital in Dakar between 1st September 2020 and 29th February 2021 (N=1134)
In our series, most of the physical examination parameters were assessed during PNC [Table 10].
| Parameters | PNC1 | PNC2 | PNC3 |
|---|---|---|---|
| Breasts | 1134(100%) | 777(99,6%) | 410(100%) |
| Uterine Globe | 1134(100%) | 778(99,7%) | 409(99,7%) |
| Parietal wound | 352 (100%) | 268(100%) | 184(100%) |
| Vaginal touch and lochia | 1134(100%) | 772(98,9%) | 401(97,8%) |
Table 10: Distribution according to completeness of PNC parameters (physical examination) in patients who had their postnatal consultation at the maternity ward of the IHS hospital in Dakar between 1st September 2020 and 29th February 2021 (N=1134)
In our series, during PNC 3, no patient underwent a speculum examination with VIA or cervico-uterine smear.
Newborn parameters
Measurements were not usually taken during PNC 2 and 3. In fact, only 2.1 and 1.5% of newborns had had their measurements taken during PNC 2 and 3 respectively. Most of the other parameters were well assessed [Table 11].
| Parameters | PNC1 | PNC2 | PNC3 |
|---|---|---|---|
| Weight | 1103(100%) | 678(89,4%) | 366(89,2%) |
| Measurements | 082(98, 1%) | 16(2, 1%) | 6(1,5%) |
| Temperature | 1015(92%) | 717(94, 6%) | 377(92%) |
| General condition | 1103(100%) | 758(100%) | 410(100%) |
Table 11: Distribution according to completeness of PNC parameters (general examination) in newborns born to mothers who underwent postnatal consultations at the maternity unit of the IHS hospital in Dakar between 1 September 2020 and 29 February 2021 (N=1103)
In the physical examination, neurological status (56.4% in PNC 1, 1.5% in PNC 2 and 15.8% in PNC 3) and the search for malformations (15.3% in PNC 1, 3% in PNC 2 and 3.1% in PNC 3) were the least evaluated parameters [Table 12].
| Parameters | PNC1 | PNC2 | PNC3 |
|---|---|---|---|
| Neurological status | 622(56,4) | 150(1,5%) | 65(15,8%) |
| Umbilical wound | 810(73,4) | 726(95,8%) | 377(92%) |
| Ocular status | 774(70,2) | 147(19,4%) | 65(15,8%) |
| Search for malformations | 169(15,3) | 23(3%) | 13(3,1%) |
Table 12: Distribution according to completeness of PNC parameters (physical examination) in newborns born to mothers who attended postnatal consultations at the maternity unit of the IHS hospital in Dakar between 1st September 2020 and 29th February 2021 (N=1134)
Complications
Maternal complications
In our study, 124 patients (10.9%) had complications. These were often cases of hypertension (6.5% of patients and 59.6% of complications) or post-partum haemorrhage (1.5% of patients and 27.4% of complications) [Table 13].
| Complications | Number | Frequency (%) |
|---|---|---|
| None | 1010 | 89,1 |
| Hypertension | 74 | 6,5 |
| Post-partum haemorrhage | 17 | 1,5 |
| Constipation | 12 | 1,1 |
| Eclampsia | 7 | 0,6 |
| Breast engorgement | 10 | 0,8 |
| Other | 4 | 0,35 |
| Total | 1134 | 100 |
Table 13: Distribution according to complications in patients who underwent PNC at the maternity ward of the IHS hospital in Dakar between 1st September 2020 and 29th February 2021 (N=1134)
Other: one case of parietal suppuration, one case of perineal suppuration, one case of vaginal thrombus and one case of suspected chorioamniotitis.
Complications in newborns
In our study, 143 newborns (13%) had complications. Asphyxia (4.3%) and infections (4%) were the most frequent [Table 14].
| Complications | Number | Frequency (%) |
|---|---|---|
| None | 958 | 87 |
| Asphyxia | 47 | 4,3 |
| Infections | 44 | 4 |
| Constipation | 29 | 2,6 |
| Myoclonus | 2 | 0,18 |
Table 14: Distribution according to complications of newborns born to mothers who underwent CPON at the maternity ward of the IHS hospital in Dakar between 1st September 2020 and 29th February 2021 (N=1103)
Breastfeeding
In our series, exclusive breastfeeding was practiced in 78% of cases and mixed breastfeeding in the remaining 22%.
Family planning
In our study, of the 1134 patients, 346 (30.5%) had benefited from post-partum family planning during PNC. Most of these patients had given birth by caesarean section (76.3%). The contraceptive methods chosen were dominated by progestogen implants (73.4%), followed by copper intrauterine devices (18.1%) and oestroprogestogen or progestogen pills (5.2%) [Table 15]. For the women who had not chosen a contraceptive method during the PNC, the reasons given were:
| Contraceptive methods | Number | Frequency (%) |
|---|---|---|
| Implants | 254 | 73,4 |
| Intrauterine devices | 63 | 18,2 |
| Pills | 18 | 5,2 |
| Tubal ligation | 2 | 0,6 |
| Injectables | 9 | 2,6 |
| Total | 346 | 100 |
Table 15: Distribution according to contraceptive method among patients who underwent PNC at the maternity ward of the IHS hospital in Dakar between 1 September 2020 and 29 February 2021 (N=346)
• Absence of the husband (25.4%)
• Need for time to think (13%)
• Refusal for no reason given (61.7%)
Analytical results
Compliance with recommended PNC and age (p =0.92), parity (p =0.68), place of residence (p = 0.16) and marital status (p = 0.50) were not significant.
Compliance with ONCs and number of ANCs performed
Compliance with the ONCs was greater the more the patient had undergone 4 or more ANCs. In fact, 48.5% of patients who had undergone 4 or more PNC complied with the PNC, compared with only 4.5% of those who had undergone less than 4 PNC. There was a statistically significant relationship between the number of ANC performed and compliance with the recommended ONC with p < 0.01 [Table 16].
| Compliance with recommended PNC | |||
|---|---|---|---|
| Number of PNCs performed | Yes | No | Total |
| 4 ANC or more | 380(48,5%) | 402 (51,5%) | 782 (100%) |
| Less than 4 ANC | 16 (4,5%) | 336 (95,5%) | 352 (100%) |
| Total | 396 | 738 | 1134 (100%) |
Table 16: Compliance with recommended PNC according to the performance of antenatal consultation (ANC) in patients at the IHS maternity hospital in Dakar between 1st September 2020 and 29th February 2021 (N=1134)
Compliance with recommended ONCs and route of delivery
In our series, women who had given birth by caesarean section were more likely to follow the recommended PNC. In fact, 50.5% of women who had a caesarean section complied with the recommendations compared with only 27.9% of those who had a vaginal delivery, with a statistically significant link between the mode of delivery and compliance with the recommended PNC (p < 0.01) [Table 17].
| Compliance with recommended PNC | |||
|---|---|---|---|
| Delivery route | Yes | No | Total |
| Vaginal delivery | 218(27,9%) | 564(72,1%) | 782(100%) |
| Caesarean section | 178(50,5%) | 174(49,4%) | 352(100%) |
| Total | 396 | 738 | 1134(100%) |
Table 17: Compliance with recommended PNC according to mode of delivery at the IHS maternity hospital in Dakar between 1st September 2020 and 29th February 2021 (N=1134)
Frequency
In our study, we carried out 2324 post-natal consultations out of the 3402 expected, i.e. a coverage rate of 68.3% and an average of 2 PNC per patient. Only 396 patients (34.9%) had completed all three consultations. Our results differ from those presented in the SR review of the Dakar medical region in the first quarter of 2010. These data show that only 14.9% of women in Pikine department attended the three required postnatal consultations [6]. Similarly, in Ann's study [6], the coverage rate for post-natal consultations was 23.2%, which is much lower than our result. Our high rate of PNC compared with the literature could be explained by the counseling on the benefits of PNC carried out during antenatal care and also during hospitalization in the post-partum period.
The first postnatal consultation (PNC 1) was carried out in all patients in our series. Our rate was much higher than those obtained by Kanté [7] in Tanzania and Kassambara [8] who found 43.5% and 61.5% PNC 1 respectively. In Morocco, a study on the determinants of the use of postnatal consultation in the prefecture of Skhirat-Temara in 2013 showed that 87% of women giving birth had completed their PNC [9]. Also, according to the report of the 2018 multiple indicator demographic and health survey in Senegal, 9% of patients who gave birth in the facilities had not completed their first postnatal consultation [10]. In our practice, we systematically carry it out before discharge from the maternity unit, which would explain the 100% coverage rate we recorded.
Regarding PNC 2, 68.7% of patients had undergone it. Our result was lower than that of Koné [11], which was 89.2%, and higher than that of Ann [6], who reported 20.7% PNC 2. The third postnatal consultation was carried out in only 36.1% of patients. Our result is comparable to that of Koné [11] which was 43.3%. There are various reasons for this low rate of PNC 3:
• The fact that in the absence of complaints, many women think that it is not necessary to come for a consultation,
• Most women giving birth prefer to continue with PNC close to home,
• During the COVID 19 pandemic, to reduce the risk of contact linked to travel, we reduced the number of PNC to two and advised patients to have PNC in the health facilities closest to their place of residence.
Patient characteristics
The average age of the women in our series was 27 years, with extremes of 14 and 46 years. The 20-29 age group was the most represented with 53.1% of patients. Our results are comparable with those of Ann [6] who found a mean age of 28.1 years and a predominance of women in the 20-29 age group (55%), which corresponds to the optimal period for childbearing. Primigravida were in the majority in our series (39%) whereas in the study by Koné [11], paucigravida were the most represented with 44.6% of cases. In terms of clinical characteristics, most of the patients (68.9%) had given birth vaginally. There were 26.3% episiotomies, which is relatively high́ if compared with the figures of 3.4%, 7.7%, 10.2% and 16.75% found respectively by Eckman [12] in France, Harrison [13] and Badji [14] in Senegal. The caesarean section rate was 31.1% in our study. Within healthcare institutions, this rate varies considerably according to the profile of the patients they care for, their reception capacity, and the human and material resources at their disposal. For all these reasons, the caesarean section rate recommended for the general population, which is 5 to 15% of deliveries [15], cannot be considered the ideal rate for referral hospitals such as the Institut d'Hygiène Sociale, which often receive pathological cases requiring a caesarean section.
Immediate post-partum monitoring and follow-up during hospitalization
Monitoring of the new-born baby was generally well practiced, but it should be noted that diuresis was monitored in only 1.1% of patients with vaginal deliveries. Parameters such as blood pressure, pulse, monitoring of vulvar bleeding and safety globe should normally be checked every 15 minutes. In our study, this was done in 3/4 of the patients, unlike the Siby studies [16], where these parameters were monitored in only 48 of the patients. In our study, the average length of hospital stay after vaginal delivery was 24 hours and after caesarean delivery 72 hours. Compared with the data in the literature, this average length of stay was lower than that reported by other authors. In France, the average length of hospital stay for vaginal deliveries fell from 5.3 to 4.3 days between 1997 and 2010, according to data from the Programme de Médicalisation des Systèmes d'Information (PMSI) [17]. Coulibaly [18] and Teguete [19] found that the average length of hospital stay after a caesarean delivery was 192 and 216 hours respectively. This short length of stay in our practice is explained by the limited number of hospital beds. Discharge is authorized after 24 hours for vaginal deliveries, and after 48 to 72 hours for caesarean deliveries, if the post-natal period is normal. This is the early discharge from the maternity unit that we have adapted to our practice out of necessity. However, it requires certain conditions to be met.
Post-natal consultation
Gynaecologists and obstetricians carried out 1,268 PNC (54.6%), including 464 (30.5%) in women with vaginal deliveries. Midwives, on the other hand, performed 1056 PNC (45.4%), exclusively in women with vaginal deliveries. In the Koné study [11], midwives performed PNC in both vaginal and caesarean births.
Postnatal consultation parameters were assessed in most patients, but it should be remembered that weight was taken in only 1.9% of patients at PNC 1, 27.4% at PNC 2 and 39% at PNC. Similarly, during PNC 3, no patient underwent a speculum examination with VIA/VILI or cervical smear, even though these examinations are recommended during PNC to detect precancerous and cancerous lesions of the uterine cervix. This is therefore a gap that we need to fill in our PNC practice. Indeed, Sy [20] made the same observation in her thesis on cervical cancer, with 82.1% of patients surveyed never having undergone a post-partum cervico-uterine smear. It would therefore be important to carry out opportunistic screening whenever the opportunity arises. In newborns, measurements were often neglected at PNC 2 (2.1% of cases) and PNC 3 (1.5% of cases), as was the neurological examination (1.5% at PNC 2 and 15.8% at PNC 3). The taking of measurements in newborns is of vital importance and is compulsory in every PNC. This is because it enables the early detection of a delay in weight and height, and the search for the cause, so that appropriate treatment can be given at an early stage. Similarly, the neurological examination should be repeated at each PNC to ensure that the newborn is adapting well to life outside the womb, particularly its psychomotor development.
Our study showed that only 34.9% of patients had complied with the recommendations for adequate post-natal follow-up. This result is comparable to that of Chemgne [21] with 34.5% and much higher than those recorded by Koné [11] and Ann [6] which was 15.1% and 5.8% respectively. If we consider the route of delivery of the patients, it appears that those who gave birth by caesarean section complied more closely with the ONC schedule (50.57% compared with 27.88%). A bivariate analysis showed that there was a statistically significant link between mode of delivery and compliance with recommended ONC (p < 0.01). The same observation was made by Koné [11] with 15% of caesarean section patients compared with 0.1% of vaginal birth patients who complied with PNC. This could be explained by the fact that caesarean patients are obliged to return to the clinic for treatment of the surgical wound or to monitor a particular pathology (hypertension, diabetes, etc.). It would therefore seem necessary to raise patients' awareness of the benefits of PNC from the ANC.
Analysis of the relationship between age and compliance with PNC showed that younger patients had performed more recommended PNC without there being a statistically significant relationship between age and compliance with the number of recommended PNC (p =0.92). Age at delivery is an important factor in the analysis of inequalities in the use of maternal health services and health services in general. Moreover, the literature shows that younger women are more likely to seek care during pregnancy, childbirth and the post-partum period than older women, mainly because of the greater weight of traditional values among the latter [22].
In our series, primiparous women (37.6%) were more likely to comply with ONCs, although there was no statistically significant link between parity and complain with the recommended number of ONCs (p=0.68). De Sousa [23] found that "the choice of modern assistance, in hospital, is more frequent for first births" and concluded that "it can be assumed that greater care is taken with first births". Diallo [24] found that in Guinea, 65.48% of multiparous women (2 to 4 children) and 55.88% of large multiparous women (5 or more children) gave birth at home, compared with 13.09% and 25% respectively of primiparous women. In the authors' own words, "the habit and experience acquired during previous childbirths seem to lead them to dispense with health facilities". With regard to marital status, it appears that women in union are more likely to perform the recommended PNC than single women, with frequencies of 35.97% and 30.77% respectively. Women in union are more likely to seek care before, during and after childbirth, mainly because their social network is more likely to cover healthcare costs [22].
In our study, patients who had undergone recommended ANC were more compliant with PNC than those who had not (37.50% versus 14.29%). There was a statistically significant association between the performance of recommended ANC during pregnancy and compliance with PNC (p < 0.01). Numerous studies on the use of postnatal care services have identified compliance with ANC during pregnancy and delivery in a qualified environment as factors positively influencing the use of these services [9]. Indeed, the more a woman performs the recommended ANC and gives birth in a health facility, the more likely she is to be informed about the existence and usefulness of post-natal care [25, 26].
Our results showed that patients living in the Dakar department were more complacent about postnatal care than women living in the suburbs. However, there was no statistically significant association between place of residence and compliance with the recommended number of CPONs (p = 0.16). Also with the advent of COVID 19, to reduce travel, most patients living in the suburbs of Dakar carried out their PNC close to home.
Family planning
In our study, of the 1134 patients, 346 had benefited from postpartum family planning, i.e. a frequency of 30.5%. This rate is lower than that reported by Niang [27], which was 38.1%, and much higher than that of Ann [6], which was 9.2%. Patients who had given birth by caesarean section accounted for 76.3% of postpartum family planning cases. This could be explained by the fact that vaginal deliveries only stayed in the maternity unit for 24 hours after delivery because of our reduced hospital capacity. The implant was the most commonly used method, accounting for almost ¾ of patients (73.3%), followed by the IUD (18.2%). Our results were similar to those of Niang [27] who recorded 71.7% implants. In contrast, in Sidibé's series [28], the pill was the most frequent method (48%) followed by injectable contraception (40%) and implants (22%). In Benin, the study by Sainzoux [29] showed that condoms were the most commonly used contraceptive method (40.69%), followed by pills (27.11%). In our practice of post-partum family planning, we note a predominance of longacting methods in the choice of patients, particularly implants.
This is the service's vision, in line with international recommendations aimed at increasing contraceptive prevalence worldwide, particularly in our developing countries. In Senegal, with the adoption of the National Action Plan for Family Planning, the government has embarked on a policy of repositioning family planning, with the aim of increasing the contraceptive prevalence rate.
Complications
In our series, complications were noted in 10.9% of patients. This rate was similar to that reported by Sawadogo [30], which was 9.67%, but lower than that of Ténété [31], who found 3.13% puerperal complications. Postpartum hypertension was the most frequent complication, accounting for 59.6% of complications. In the study by Sawadogo [30], the rate was 33.14%. Post-partum haemorrhage accounted for 27.4% of complications and 1.5% of deliveries. This rate is similar to that of Shaheen [32] in Pakistan, which was 1.6% of admissions. It is lower than those reported by Bang [33] in India and Telly Sy [34] in Guinea, which were 3.2% and 5.21% of admissions respectively. This difference may be due to the fact that Bang's study concerned only severe post-partum haemorrhage, whereas our work took into account all cases of postpartum haemorrhage. Furthermore, in our practice the estimation of blood loss is lacking and is subjective because it is based on visual criteria which often underestimate it. There were no cases of death during our study; Koubi [35] and Sawadogo [30] respectively found case fatality rates of 2% and 1.97%.
CPON coverage could be improved among patients who gave birth at the IHS maternity hospital, despite the acceptable rate we recorded. This will require raising the awareness of all those involved in maternal and neonatal care. We must seize this opportunity to screen for cervical cancer using the VIA test, the FCV and/or the HPV test.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Citation: SAMB F (2024) Post-natal consultation at the institute hygiene social hospital in Dakar: about 2324 cases collected between 1 September 2020 and 29 February 2021. 13(1):708.
Received: 01-Jan-2024, Manuscript No. JWH-24-28885; Editor assigned: 03-Jan-2024, Pre QC No. JWH-24-28885; Reviewed: 17-Jan-2024, QC No. JWH-24-28885; Revised: 22-Jan-2024, Manuscript No. JWH-24-28885; Published: 29-Jan-2024 , DOI: 10.35248/2167- 0420.24.13.708
Copyright: © 2024 SAMB F. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited