International Journal of Physical Medicine & Rehabilitation
Open Access
ISSN: 2329-9096
ISSN: 2329-9096
Research Article - (2022)
In patients with Obstructive Sleep Apnea (OSA), Upper Airway (UA) collapse occurs when the forces of the UA muscles become less than those produced by negative pressures, resulting in loose soft tissue (uvula and surroundings) at the back of the mouth. Continuous Positive Airway Pressure (CPAP) at a predetermined titration pressure normally provides continuous pressurized and humidified air to prevent airway collapse. However, many patients cannot tolerate high titration pressures, which may have health implications, such as stroke, especially in patients diagnosed with cardiovascular disease. A Super-Imposed Pressure Oscillation (SIPO) technique was proposed to reduce the titration pressure by superimposing the oscillating pressure on the CPAP-reduced pressure. Using MRI scans, this study focuses on developing a computer model to predict diagnostic parameters such as the Hydraulic Diameter (HD), Lateral Pharyngeal Wall (LPW) thickness, and Apnea-Hypopnea Index (AHI) under three scenarios: OSA, CPAP, and CPAP with SIPO. Head and neck MRI sessions were performed. UA obstruction is discussed in preparation for ANSYS analysis of the three scenarios at various times within the breath cycle. SIPO on CPAP showed significant improvement over CPAP treatment. Correlations between HD, AHI, LPW, and disease severity have been well established.
Apnea hypopnea index; Obstructive sleep apnea; Superimposed Pressure Oscillations (SIPO); Continuous positive airway pressure
Obstructive Sleep Apnoea (OSA) normally results in various health implications that reduce the quality of life [1]. It is characterized by recurrent episodes of pharyngeal airway obstruction and collapse during sleep [2] which can occur either at the level of the uvula or the tongue [3] due to the lack of bone structure. Upper Airway (UA) obstruction may occur when the forces generated by UA negative pressures exceed the forces produced by the UA muscles [4,5]. The tendency for UA obstruction and collapse increases during sleep in the supine position due to gravitational forces which pull the soft tissues towards the airway walls, reducing the breathing air gap [6].
OSA patients may experience hundreds of apnoea events per night [7] resulting in restless sleep which may lead to hypersomnolence and diabetes [8], arrhythmia [9], stroke, hypertension, memory loss, cardiovascular disease, and low sexual drive in men [10,11]. The pathophysiology of OSA appears to be the result of anatomical and neuromuscular susceptibility factors; however, the exact mechanism is not fully understood. UA collapse can be related to the positioning of the fat tissue on the lateral wall of the pharynx [12]. However, previous studies were based on static inspections, which reflect only one point in time. UA obstruction is a dynamic process in patients with OSA and requires a time-dependent study to show a history of complete obstruction.
Continuous Positive Airway Pressure (CPAP) is considered the first standard treatment for patients diagnosed with moderate-to-severe OSA [13]. However, there have been many rejections of CPAP owing to nasal congestion and dryness [14]. Furthermore, patients with cardiovascular disease may experience stroke symptoms owing to high titration pressures [15]. The pharyngeal and UA muscle activities increase when stimulated by pressure oscillations. Super-Imposed Pressure Oscillation (SIPO) has been successfully proven to keep the UA open with no form of collapse during both inspiration and expiration and at reduced-titration CPAP settings [16]. This study focuses on developing a computer model to predict some commonly used diagnostic parameters such as Hydraulic Diameter (HD), Apnoea-Hypopnoea Index (AHI), and Lateral Pharyngeal Wall (LPW) under three scenarios: OSA, CPAP alone, and CPAP with SIPO.
UA Constructions
All procedures were approved by the Ethics Committee of the Auckland University of Technology. Limited head and neck MRI scans were obtained for 10 patients with OSA (seven males and three females). All participants were tested by an Ear, Nose, and Throat (ENT) specialist to examine their upper airways. The first two columns of the demographic data for the participants including Column1: identification number, sex (M or F), and age; Column 2: body mass index (kg/m2) and neck circumference (Cm), age, and sex. All participants were New Zealand European with a mean age of 55.0 ± 2.6 years. The study excluded smokers, subjects with metallic implants including pacemakers, and those with surgical intervention and pregnancy.
MRI data of the UA were collected by a registered radiographer at the University of Auckland Centre for Advanced MRI. Each participant assumed a recumbent position within the MRI scanner, with the coil positioned over the head of the subject. Figure 1 shows a sample of the collected MRI data scan for the UA, indicating the region of interest, that is, the nasopharynx, oropharynx, and laryngopharynx.
Figure 1: Materialise Mimics 3D image segmentation process: (A) coronal plane view; (B) Axial Plane; (C) sagittal plane and (D) a 3D window.
DICOM files were converted into IGES format to prepare MRI images for UA construction. The Mimics software was used to track the UA region. After the study file was imported, the UA was selected and converted to a Mimics project file containing all images. Once the alignment of the images was confirmed, three flat views were obtained.
Figure 1 shows the coronal plane view (A), axial plane (B), sagittal plane (C), and 3D window (D) in which each 3D-model can be displayed. Pre-defined MRI scans were selected to set the threshold at which the required area was highlighted. By activating the 3D preview, the segmented model could be clearly verified.
The target area which included the nasopharynx, oropharynx and hypopharynx parts was selected, cut, and then constructed as a 3D model from the top three views. It was then flattened to create smooth edges and the UA model was converted to STL format and exported to the Meshmixer software, which was used to modify the bulky UA into a hollow enclosure. With the "Hollow" command, the model was marked with a shell thickness of 1 mm [17]. The newly created STL file was imported as a Solid Body into SolidWorks Software and exported into IGES format to be examined in the ANSYS Fluent Software.
Bi-directional Fluid-Structure Interaction (FSI)
Airflow was a combination of the breath cycle with CPAP or CPAP and SIPO pressure, all of which were set to the CFX fluid setting. Solver "Computational Fluid Dynamics (CFD) can solve the deformations of the UA wall when the interaction (coupling) between the UA hyperelastic wall and the airflow is established. Bi directional Fluid-Solid Interaction (FSI) was used to create the breakdown of the UA (respiratory arrest) and increase the narrowing of the UA to test the effectiveness of the airflow under the three scenarios. Apnoea was defined as an airflow reduction of 90% and hypopnoea as an airflow reduction of 30% [18]. A 10% reduction in the airway radius (upper third of the hypopharynx) results in a 35% decrease in airflow in the UA anatomical regions [19], which can lead to apnoea syndrome [20,21].
For the UA tissue, a hyperelastic material was selected on the ANSYS Workbench [17] with E=18 kPa. Poisson’s ratio in the range 0.45-0.49 [22] was implemented and did not show any significant difference in the results. The temperature range was set to 37-38 to simulate the reported air temperature in the lungs, and the density was set to 1000 kg/m3 [23]. The instantaneous shear modulus was set to 10480 Pa. CFD/CFX simulations were performed to determine the viscoelastic behaviour of the tissue.
For the SIPO condition, a mean titration pressure of 70% was used to mimic that used in a previous clinical trial [24]. The normal CPAP titration pressure was in the range of 4-20 CmH2O; thus, the reduced pressure was in the range of 4-14 CmH2O. The IGES file of the UA model was loaded into the geometric design module. The geometry was created such that the UA was assumed to be an enclosure with a 1 mm wall thickness filled with air.
Meshing is an important ANSYS function that differs between airspace and tissue. Airway models were solved using the Fluid-Flow (CFX) Modeller on the ANSYS Workbench diffusion (smoothing) method with a linear elastic solid and spring/boundary layer/ Laplace [23] because of its tendency to produce better mesh quality. The simulations were repeated for different SIPO frequencies and amplitudes [24]. The complete breath cycle takes 4 s, with 2 s for a single inhalation and 2 s for a single exhalation. However, an automatic meshing method is used in the static structural analysis to avoid discrepancies in the resulting meshing. To examine ANSYS meshing efficiency, a skewness 0.5-1 indicates bad cell quality and 0-0.5 is good to excellent. This model yielded a skewness of less than 0.2 which is an excellent meshing quality [17]. The number of nodes and elements were 15332 and 15358, respectively.
Fluid flow analysis
Simulations were performed to represent pharyngeal obstruction in OSA, CPAP therapy, or both CPAP and SIPO therapy.
Pharyngeal obstruction (collapse-case)
While conscious in the supine position, MRI showed that the patients could have UA narrowing, but no full UA obstruction was observed. To investigate OSA in these participants, pharyngeal obstruction/airflow reduction was performed at the level of the tongue [17]. The external pressure strain originates from the posterior part of the decreased genioglossus, hyoglossus, and geniohyoid muscles (tongue base level) into the pharynx (Figure 2). A common tongue weight of approximately 60-70 grams with a cross-sectional region of the pharyngeal beginning of 700 mm2 was considered [25,26]. Thus, to set the pressure, it was observed that using an inward directional pressure of 2500-3000 Pa towards the hypopharynx resulted in airflow reduction. This was executed to achieve a 90% airflow reduction [27].
Figure 2: (A) Tongue presses on the hypopharynx; (B) Arrow pointing towards the model shows the external load on the pharyngeal part at the base of the tongue.
ANSYS shows that the maximum deformation inside the UA wall represents the inward/outward displacement distinction that is positioned among the unique geometry before and after applying the loading. Therefore, the following equation is proposed to measure the UA pharyngeal gap anterior/posterior assuming zero minimum obstruction.
UA gap (mm) = Obstructive deformity mm-CPAP/SIPO (mm) deformity (1)
CPAP application
Under CPAP, we used the same respiratory cycle (inspiration/ expiration) and obstruction. The first step in this modelling process was to adjust the inlet/outlet pressure to maintain the 70% titration pressure used in the initial clinical trial (0.4-1.4 kPa). The air direction in the script is during the inhalation process, whereas the exhalation process assumes the opposite direction. However, in the software, it was coded to make it resemble a breathing cycle with two breaths each time. As the CPAP introduces a pneumatic splint in the UA to help patients overcome apnoeic obstructions, in the modelling process, we considered the inlet at the nasopharynx and the outlet at the trachea inlet. Deformation of the UA was observed using UA static analysis.
CPAP with SIPO application
CPAP with SIPO has been proposed as an improved treatment method that reduces titration pressure and UA dryness by stimulating salivary secretion [16]. This method s achieved by superimposing pressure oscillations on a CPAP device during the breathing cycle. Thus, the applied pressure P in KPa is assumed to be
P=CPAP pressure+0.1 sin(ωt) kPa (2)
In the actual operation, the SIPO was adjusted to simulate clinical trials. 0.1 kPa in the equation represents an oscillating pressure of 1 cmH2O. Finally, pr essure enters the UA from the nasopharynx as the CPAP is delivered
Diagnostic parameters
This section summarises the diagnostic parameters for three scenarios: OSA obstruction, CPAP, and CPAP with SIPO. These parameters are UA HD, PWT, LPW and AHI. HD is determined
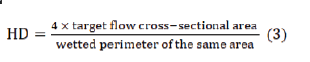
To determine this, the UA geometry was cross-sectionally cut at the deformed area and then exported to the Bluebeam software for HD calculations. To check the HD values, the same cross section was measured using software, DICOM 3D Image and Radiant, and the outcomes were in excellent agreement. Table 1 shows the calculated HD and size of the flow opening for obstructions under the three scenarios stated above.
| Pt. ID | HD awake | HD obstruction | Obstruction opening percentage % | HD CPAP | CPAP opening percentage % | HD SIPO | SIPO opening percentage % |
|---|---|---|---|---|---|---|---|
| 1 | 38.8 | 4.2 | 10.80% | 8.996 | 23.20% | 9.336 | 24.10% |
| 2 | 40.5 | 4.6 | 11.30% | 8.95 | 22.10% | 10.5 | 25.90% |
| 3 | 46.5 | 5 | 10.90% | 8.845 | 19.00% | 18.61 | 40.00% |
| 4 | 49 | 5.5 | 11.20% | 7.13 | 14.60% | 11.1 | 22.70% |
| 5 | 18.1 | 1.945 | 10.70% | 5.411 | 29.90% | 11.5 | 63.50% |
| 6 | 28.6 | 2.67 | 9.30% | 5.8 | 20.30% | 7.8 | 27.30% |
| 7 | 29.5 | 3.3 | 11.20% | 12.1 | 41.00% | 24.5 | 83.10% |
| 8 | 23 | 2.4 | 10.40% | 7 | 30.40% | 14.9 | 64.80% |
| 9 | 27.6 | 2.9 | 10.50% | 5.8 | 21.00% | 11.2 | 40.60% |
| 10 | 28 | 3 | 10.70% | 5.1 | 18.20% | 11.5 | 41.10% |
Table 1: HD under: awake, OSA obstruction, CPAP and CPAP with SIPO.
PWT in centimetres is the distance between the edge of the UA sidewall tract and the inner edge of the pharyngeal fat pad measured on both side of the pharynx. The average of the two gives LPW thickness which normally can be measured by (i) the lateral distance between the pharyngeal fat pad and the edge of the UA wall on either side of the neck, or (ii) the distance between the carotid artery and the edges of the UA walls on both sides (Figure 3). A low PWT value implies that the UA is wide enough to allow more air to enter the lungs, which leads to a healthy sleep pattern. In general, the pharynx of men is found to be thicker than those of women, and hence less air is allowed into the lungs. This agrees with the statistics showing OSA prevalence is more in men than women.
Figure 3: Level of pharyngeal anatomy used to calculate the LPW thickness.
AHI is normally used to measure the severity of OSA. A previous study has indicated that LPW thickness is the most important factor predicting the severity of OSA and that AHI is directly proportional to LPW. In that study 76 participants received polysomnography during sleep to measure their AHI. All participants received ultrasound distance measurements and PSG, and MRI data were collected for 15 of them. A good correlation was found between the ultrasound and MRI measurements of the pharynx. In our study, Bluebeam Revu × 64 extreme software version 12.0 was used to measure the throat thickness of the 10 participants. According to the increase and decrease of HD obtained from ANSYS simulations, the obstructions under OSA, CPAP and both CPAP with SIPO measurements were determined from the participants’ pharynx thicknesses.
HD and LPW
Table 1 shows the HD of the 10 patients tested in this study. The percentage of opening under OSA ranged from 9.3-11.3%, under CPAP 14.6%-41%, and CPAP with SIPO 22.7-64.8. This indicates that a significant improvement occurred with the SIPO.
LPW thickness was measured for 10 OSA participants, and the results were added to the 76 participants and are presented in Figure 4. There was a direct correlation between ultrasound and MRI LPW thickness (r=0.78, P=0.001). The LPW thickness had high repeatability, and the correlation coefficients were within the range of 0.90-0.97 for the reliability of the inside and between the operators. There were 58 participants with significantly elevated OSA (AHI ≥ 10/h) had a high Body Mass Index (BMI), larger neck circumference, and high LPW. The thickness measured using ultrasound was greater than ours (n=18), and the hourly AHI was less than 10. In univariate analysis, LPW thickness was positively correlated with AHI (r=0.37, P=0.001). In the multivariate analysis, after adjusting for age, sex, neck circumference, and BMI, LPW thickness was positively correlated and independent of AHI. The positive correlation between LPW thickness and AHI was only valid for men in univariate and multivariate analyses (n=62).
Figure 4: The relationship between LPW and AHI:
Significance of air pressure on UA walls: Two-way FSI was applied to 10 UA geometric shapes and simulations were conducted to investigate the effect of air pressure on the hyper-elastic UA track. The effect of air pressure load during the respiration cycle under the three conditions. The results of the finite element analysis are displayed through colour coding: red indicates the point of maximum deformation, blue indicates the point of minimum compressive load, and green represents the effect of the average force on the wall. The minimum deformation level of all geometric shapes is ~0 (position), far from the applied pressure after the load is distributed, where there is almost no force. Each model was viewed from front, side, and back. The internal deformations in contact with the front wall of the neck are shown in this figure.
In three scenarios (subjects 1,3,4,8 and 9), the largest deformities were concentrated in the posterior hypopharyngeal wall. However, the largest deformations in models 2,5 and 6 occurred on the anterior pharynx wall. Lateral deformations were also observed in Models 6,7 and 9. Anterior deformity is related to pressure therapy to expand the tongue and UA of the uvula. Similar to actual clinical trials, the AHI score at this location was higher. Lateral deformity represents the fact that the treatment puts pressure on the lateral pharyngeal muscles (i.e. upper and lower pharyngeal muscles, throat, and underneath the tongue), and a patient can effectively fall asleep without lying on the back; subsequent deformities cause the treatment to affect the pharynx muscles, which start at the front of the neck and end at the back of the neck.
Table 2 lists the maximum deformations for the three scenarios considered in this study at various times during the breathing cycle. The percentage change in HD in the three cases (Table 1) was subtracted from the maximum deformation of the obstacle (representing the lower value of the maximum deformation) to obtain the accessible air opening value. Subtract the value obtained from the LPW thickness in the case of obstruction and then change each value into a case divided by two to obtain the average thickness of the pharynx. The procedure is expressed as follows obstructed;
| Patient | 1st sec | 2nd sec | 3rd sec | 4th sec | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Obst | CPAP | SIPO | Obst | CPAP | SIPO | Obst | CPAP | SIPO | Obst | CPAP | SIPO | |
| 1 | 3.3 | 1.7 | 0.21 | 3.21 | 1.86 | 0.91 | 3.02 | 2.95 | 2.34 | 3.2 | 2.31 | 1.43 |
| 2 | 4.71 | 2.03 | 0.11 | 4.67 | 3.03 | 1.26 | 3.71 | 3.04 | 1.28 | 3.71 | 3.03 | 0.28 |
| 3 | 4.16 | 4.76 | 0.91 | 5.6 | 4.5 | 0.12 | 4.16 | 4.51 | 1.13 | 4.16 | 4.55 | 1.46 |
| 4 | 3.15 | 1.68 | 0.42 | 1.27 | 1.75 | 0.99 | 1.25 | 1.76 | 1.1 | 1.39 | 1.83 | 1.21 |
| 5 | 1.74 | 2.96 | 0.51 | 1.5 | 2.45 | 0.69 | 2.37 | 2.44 | 0.39 | 3.54 | 2.33 | 0.33 |
| 6 | 2.32 | 0.99 | 0.17 | 1.26 | 0.93 | 0.67 | 1.21 | 1.02 | 0.76 | 1.22 | 1.07 | 0.76 |
| 7 | 1.97 | 2.77 | 0.33 | 1.98 | 1.96 | 0.19 | 3.98 | 1.78 | 0.18 | 2.45 | 1.92 | 0.65 |
| 8 | 0.60 | 0.20 | 0.23 | 1.11 | 0.58 | 0.76 | 1.51 | 1.51 | 1.12 | 3.11 | 2.7 | 0.11 |
| 9 | 4.02 | 3.91 | 0.7 | 4.80 | 3.82 | 0.8 | 3.78 | 3.82 | 0.85 | 3.87 | 3.83 | 0.9 |
| 10 | 2.58 | 1.57 | 0.32 | 3.52 | 1.49 | 0.19 | 1.46 | 0.48 | 0.21 | 0.48 | 0.54 | 0.57 |
| Mean ± SE | 2.86 0.40 | 2.26 0.43 | 0.39 0.08 | 2.89 0.54 | 2.24 0.4 | 0.66 0.12 | 2.64 0.39 | 2.33 0.40 | 0.94 0.20 | 2.71 0.40 | 2.41 0.38 | 0.77 0.15 |
Table 2: Maximum Deformations (mm) at various times within the Breath Cycle-Obstructed, CPAP and CPAP with SIPO.
LPW=Bilateral LPW+Obstructed maximum deformation (4)
Pharyngeal gap CPAP=Maximum obstruction-Minimum CPAP deformation (5)
LPW CPAP=LPW obstruction–Pharyngeal opening CPAP (6)
Pharyngeal opening SIPO=Maximum obstruction–Minimum deformation (7)
LPW SIPO=LPW obstruction–pharyngeal opening SIPO % use of SIPO therapy (8)
The average expected AHI for the CPAP treatment (Figure 5) decreased by 11.9%, whereas that for the SIPO treatment decreased by 24.7%.
Figure 5: 3D View of UA Modelling.
Comparing the maximum deformations for the three scenarios, Table 2, it can be seen that the largest deformation in the participants occurred in the first two seconds (inhalation) with participant no. 3,4,6,9 and 10. In the 3rd and 4th seconds, participants 5,7 and 8 observed the largest deformities. The maximum distortion of the obstruction was between 2 mm and 5.4 mm until the CPAP therapy was gradually reduced between 0.5 mm and 4.5 mm. During SIPO therapy, the distortion ranged from 0.11 mm to 1.12 mm.
To check the effectiveness of CPAP and SIPO treatments for obstruction in the first four seconds (Table 3), the historical time of UA malformation was considered. The mean ± SE of 1st second in the obstruction condition was 2.86 ± 0.40, while the obstruction was reduced to 2.26 ± 0.43. The number of SIPO cases also continued to drop to 0.39 ± 0.08. Among these three cases, the deformation in the first second is the largest.
| Pt. ID-gender &age | Original Clinical Data | Obstructed | Under CPAP | CPAP+SIPO | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| BMI-Neck | LPW mm | AHI Event/h | CPAP-CmH2O | LPW mm | AHI | LPW mm | AHI | LPW mm | AHI | |
| 1-M43 | 29.1-42 | 34.8 | 36.7 | 13 | 38.1 | 77 | 36.5 | 61 | 35.01 | 51 |
| 2-M60 | 28.9-43 | 33.1 | 44.0 | 12 | 37.81 | 75 | 36.13 | 57 | 33.21 | 47 |
| 3-F42 | 61.8-52 | 41.7 | 95.0 | 10 | 47.3 | 102.5 | 46.2 | 94 | 41.82 | 87.5 |
| 4-M60 | 35.1-49 | 39 | 15.0 | 11 | 42.15 | 87 | 40.68 | 83 | 39.3 | 72 |
| 5-M54 | 33.4-44 | 35.87 | 15.6 | 11 | 39.41 | 72 | 38.2 | 69 | 36.2 | 58 |
| 6-M48 | 38.9-53 | 35.47 | 73.0 | 7 | 37.8 | 68.8 | 36.46 | 57.5 | 35.64 | 53.5 |
| 7-M60 | 36.1-46 | 35.72 | 29.0 | 12 | 39.7 | 90 | 37.5 | 75 | 35.9 | 62 |
| 8-F662 | 33.0-38 | 38.4 | 2.0 | 4 | 41.5 | 95 | 41.1 | 93 | 38.51 | 77 |
| 9-M66 | 35.5-48 | 33.4 | 22.0 | 6 | 38.2 | 82 | 37.22 | 73 | 34.1 | 55 |
| 10-F55 | 34.0-49 | 36.73 | 63.0 | 6 | 40.2 | 82.5 | 38.1 | 70 | 36.8 | 63 |
| Mean ± SE | 36.6 ± 3.0 | 36.42 ± 0.84 | 39.5 ± 9.3 | 9.2 ± 1.0 | 40.22 ± 0.92 | 83.18 ±3.35 | 38.81 ± 0.98 | 73.25 ± 4.23 | 36.65 ± 0.82 | 62.6 ± 4.02 |
Table 3: Demographic data for ten OSA participants with the modelling results for LPW and AHI under OSA obstruction, CPAP and CPAP with SIPO.
In the 2nd second of obstruction, the mean SE was 2.89 ± 0.54, while CPAP decreased to 2.24 ± 0.4 and 0.66 ± 0.12 SIPO. The decline in SIPO was different from that in the first second. The average ± standard errors of the 3rd second of the blocking sequence CPAP and SIPO are 2.64 ± 0.39, 2.33 ± 0.40, and 0.94 ± 0.20. During the 4th second, the mean ± standard error was 2.71 ± 0.40. The three consecutive obstruction cases, CPAP and SIPO were 2.41 ± 0.38, and 0.77 ± 0.15, respectively.
Compared with non-therapy cases, the thickness of the LPW was also reduced after CPAP and SIPO. The number of untreated cases after CPAP decreased from 40.22 ± 0.92 to 38.81 ± 0.98, that is 3.50% reduction, while the reduction when applying SIPO was 8.87%. When using CPAP, the expected AHI value decreased from 83.18 ± 3.35 to 73.25 ± 4.23, which is 11.938% reduction, while using SIPO, the expected AHI value decreased by 24.74%.
Comparing our results (n=10) with a previous actual sleep study (n=33) conducted according to the same modelling procedure of obstruction indicated that using CPAP with SIPO resulted in a 29.96% reduction in AHI, whereas using CPAP alone resulted in a 14.54% reduction. The significant difference between the expected AHI and actual AHI is due to the fact that the number of samples between the two groups is not equal; more UA samples need to be modelled. In the same sleeping position, each person's simulated UA pressure load and the actual pressure load should be the same. To find the correct and more accurate measurement results, the LPW lateral measurement technique should be compared with the angle measurement method.
We discuss the estimation of HD, AHI, and LPW under OSA, CPAP, and CPAP with SIPO conditions using computer modelling based on demographic and MRI data collected from 10 patients with OSA. Simulations were conducted for the pharynx settings under these conditions. The main outcome of this study was that SIPO with CPAP showed significant improvement over CPAP treatment.
We acknowledge Callaghan Innovation-New Zealand for supporting the student with fellowship number FAPX1603 during her course of study.
Ethical approval was successfully approved by the Auckland University of Technology Ethics committee.
The authors declare that they have no conflict of interest.
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef] [Google Scholar] [PubMed]
[CrossRef]
[CrossRef] [Google Scholar] [PubMed]
Citation: Al-Mohamadamin D, Al-Jumaily AM, Ashaat S (2022) Predicting Obstructive Sleep Apnea Diagnostic Parameters under Continuous Positive Airway Pressure without and with Oscillation. Int J Phys Med Rehabil. S20:002.
Received: 08-Sep-2022, Manuscript No. JPMR-22-19126; Editor assigned: 14-Sep-2022, Pre QC No. JPMR-22-19126 (PQ); Reviewed: 04-Oct-2022, QC No. JPMR-22-19126; Revised: 11-Oct-2022, Manuscript No. JPMR-22-19126 (R); Published: 20-Oct-2022 , DOI: 10.35248/2329-9096-22.S20.002
Copyright: © 2022 Al-Mohamadamin D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.