Pediatrics & Therapeutics
Open Access
ISSN: 2161-0665
ISSN: 2161-0665
Review Article - (2022)Volume 12, Issue 6
Background and objectives: Maternal problems during pregnancy are an important and influential factor on the health status and consequences of newborns. This study was performed to compare the status of premature infants born to mothers with pregnancy problems and without pregnancy problems.
Materials and methods: This cross-sectional study examined the files of 1110 premature infants admitted to Ghaem Hospital in Mashhad from 2015 to 2022. Sampling was available in this study. After reviewing information about mothers (gestational age, maternal age, type of delivery, parity, underlying diseases, pregnancy complications, placental and membranous problems) and infant (age, height, weight, head circumference, Apgar score of the first and fifth minutes), infants were divided into two groups: mothers with and without pregnancy problems.
Results: 79.7% and 20.3% of preterm infants were in the mothers with and without medical pregnancy complications groups, respectively. Higher Maternal age and cesarean-section delivery rate were associated with medical pregnancy complications (P-value <0.001). Preeclampsia, hypertension, diabetes, and heart problems were the most prevalent complications found among our population. The first minute Apgar score, weight, height, head circumference in infants of mothers with medical pregnancy complications were lower than in another group (P-value <0.05). In addition, pregnancy complications were a significant contributor to the incidence of Premature Rupture of Membranes (PROM) (P=0.012) and Respiratory Distress Syndrome (RDS) (P=0.001).
Conclusion: This study has shown that pregnancy complications adversely pose the risk of severe consequences such as preterm delivery, cesarean section, PROM, Lower weight and gestational age and RDS. In the light of our findings, proper control of high-risk mothers may face the prospect of adverse outcomes.
Pregnancy-induced complications; Mother; Neonate; Preeclampsia; Hypertension; Diabetes; Prematurity; Premature rupture of membranes
While most pregnant women experience healthy pregnancy and childbirth, some women encounter Pregnancy-Induced Complications (PIC) that threatens the health of both themselves and their neonates [1]. Risk factors such as Maternal medical conditions, maternal sociodemographic factors, past obstetric history, adverse environmental conditions, unhealthy lifestyles, and adolescent pregnancy play a critical role in the emerging PIC [1-3]. The scope of high-risk pregnancy is immense and has damaging consequences on the psychological health of the mother, neonates, and all functional aspects of the family [4-6]. Maternal medical complications such as PROM, urogenital infection, preeclampsia, cervical insufficiency, fetal malformations, polyhydramnios endanger not only the health of the mother but are also considered as strong risk factors for preterm delivery [7]. Premature birth refers to all live births before completion the 37th week of pregnancy or less than 259 days after the first day of the last menstrual period and makes up 10.6% of the total number of births [8]. Prematurity accounts for 35% of death of neonates, and 16% of children under five years [8,9]. Prematurity is a growing public health concern worldwide that has known as a principal cause of neonatal mortality and a significant contributor to neonatal long-term adverse effects [10,11]. There is mounting evidence that premature birth poses a considerable economic burden on the healthcare system, and their families are more likely to deal with psychological and financial problems [12,13].
Measuring the height, weight, and head circumference of neonates at birth are reliable methods in monitoring fetal growth and development during pregnancy. Measuring these indices deem also an informative determinant of the risk of long-term abnormalities [14]. The importance of these indicators is becoming greater when it comes to high-risk pregnancies. The literature on HC growth has highlighted the significant association of head size growth with neurodevelopmental disorders involving socio-emotional, cognitive, and motor impairments, especially in preterm neonates [15].
Pre-existing maternal medical conditions or pregnancy-induced complications are doubtlessly influential factors that lead to dire consequences on the growth of the fetus that prematurity is one the most noticeably undesired results. Prematurity can be directly caused by a related disorder such as diabetes or an adverse outcome of the treatment of a maternal condition such as preeclampsia which ultimate treatment is the termination of pregnancy. It is hoped that this research will contribute to a deeper understanding of maternal medical condition's impact on the consequences of preterm neonates. Therefore, this essay aims to provide a comparison between the health condition of premature infants born to mothers with and without pregnancy complications.
This cross-sectional study comprised 1110 preterm neonates admitted to the neonatal ward of Ghaem Hospital in Mashhad during 2015-2022. Selecting neonates was based on the availability sampling method. This study was conducted in accordance with the declaration of Helsinki and has been approved by the ethics committee of Mashhad University of Medical Sciences. The ethics committee reference number and project code are IR.MUMS. MEDICAL.REC.1399.31 and 990608, respectively. Initially, preterm newborns were recruited from the intensive neonatal care unit. Maternal, prenatal, and neonatal medical records were thoroughly evaluated in detail by the researchers. Primary inclusion criteria for the neonates were less than 37 gestational weeks and singleton. Neonates diagnosed with congenital anomalies and stillbirth deliveries were excluded from the study. Data were collected using a checklist designed in two parts of maternal and neonatal sections. The first part consists of maternal characteristics, including maternal age, delivery mode, parity, pre-pregnancy medical conditions, and pregnancy-induced complications. The second section includes data on neonatal characteristics, including gestational age, height, weight, head circumference, first and five Apgar score, and respiratory distress syndrome. Preterm neonates were divided into two groups according to a maternal medical condition, which case and control groups were made up of preterm newborns of mothers with and without experiencing PICs.
Gestational age at birth was determined based on the last menstrual period and initial ultrasound findings (before 20th week’s gestation). Maternal pregnancy complications in the case group include pre-pregnancy and pregnancy-induced diabetes, hypertension, preeclampsia, eclampsia, Help syndrome, hypothyroidism, epilepsy, infection, vaginal bleeding, severe Depression, placental abruption (placenta Previa, oligohydramnios, polyhydramnios), history of obstetric complications (addiction, history of abortion, IVF, stillbirth). Maternal hypertension was considered Systolic Blood Pressure (SBP) over 140 mmHg and Diastolic Blood Pressure (DBP) over 90 mmHg or an increase in blood pressure compared to the first trimester (SPB>30 and DPB>15 mmHg) after 20 completed weeks.
Preeclampsia diagnosis criteria were as follows:
1. Pregnancy older than 20 completed gestational weeks.
2. High blood pressure (SBP>140 mmHg or DBP>90 mmHg on two times (at least 4 hours apart) (in a case that has previously had high blood pressure: SBP>160 mmHg, DPB>110 mmHg on one point).
3. Proteinuria (protein/creatinine ratio>0.3, proteinuria>0.3 g (24-h urine) protein urine dipstick of 1) [16]. The diagnostic threshold of gestational diabetes was 92 mg/dl, 180 mg/dl, and 153 mg/dl of fast blood sugar, immediately, 1 and 2 hours after Oral Glucose Tolerance Test (OGTT), respectively [17]. Mothers who did not experience any medical complications with pregnancy were regarded as mothers with a normal perinatal period (control group).
Statistical analysis was performed using SPSS software (version 21). To representing findings, tables, graphs, and descriptive statistical indices have been used. The data were normalized using Kolmogorov-Smirnov. Pearson correlation coefficient and t-test were applied for parametric variables, and Spearman's rank correlation coefficients and Mann-Whitney were employed for nonparametric ones. Significance levels were set at less than 5% in all tests.
The initial sample consisted of 1110 preterm neonates,70 of whom died in the delivery room, 31 of whom had incomplete data, 59 of whom suffered from congenital anomalies, were excluded from the study. Ultimately, the project was performed on 950 eligible preterm infants. 79.7% of them were divided into those whose mothers were diagnosed with PIC and 20.3% whose mothers had a wholesome pregnancy period. As can be seen from Table 1, based on the independent t-test, the difference between the mean age of mothers, first Apgar score, weight, height, and head circumference at birth in the two groups were statistically significant. The figures below clearly illustrates the distribution of PIC containing preeclampsia (256 mothers), pregnancy hypertension (173), diabetes 95, hypothyroidism (89), heart disease (22), epilepsy (18), and other complications (93) (Figure 1).
| Characteristics | Mother groups | Mean ± SD | P-Value |
|---|---|---|---|
| Maternal age (year) | Normal prenatal | 27.52 ± 6.57 | P<0.001 |
| Abnormal prenatal | 30.01 ± 6.01 | ||
| Parity | Normal prenatal | 2.10 ± 1.38 | P=0.386 |
| Abnormal prenatal | 2.22 ± 1.33 | ||
| Apgar first minute | Normal prenatal | 6.85 ± 1.81 | P<0.001 |
| Abnormal prenatal | 6.32 ± 2.14 | ||
| Apgar five minutes | Normal prenatal | 7.99 ± 1.55 | P=0.329 |
| Abnormal prenatal | 7.84 ± 1.69 | ||
| Weight (g) | Normal prenatal | 1587.07 ± 560.55 | P<0.001 |
| Abnormal prenatal | 1376.08 ± 392.87 | ||
| Length (cm) | Normal prenatal | 41.59 ± 3.77 | P<0.001 |
| Abnormal prenatal | 39.94 ± 3.75 | ||
| Head circumference (cm) | Normal prenatal | 29.28 ± 2.78 | P=0.031 |
| Abnormal prenatal | 28.77 ± 2.39 |
Table 1: Maternal and neonatal characteristics, in two groups of mothers with and without PIC.
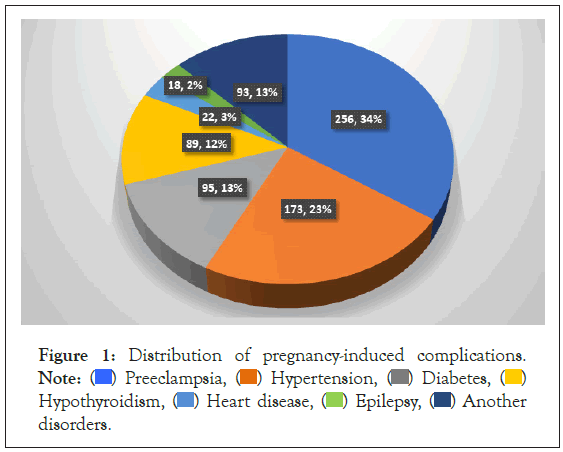
Figure 1: Distribution of pregnancy-induced complications. Note:  Preeclampsia,
Preeclampsia,  Hypertension,
Hypertension,  Diabetes,
Diabetes,  Hypothyroidism,
Hypothyroidism,  Heart disease,
Heart disease,  Epilepsy,
Epilepsy,  Another
disorders.
Another
disorders.
A chi-square test revealed no clear distinction between the need for cardiopulmonary resuscitation and neonatal gender in the two groups. The results of our study show that in mothers with pregnancy problems 68.5% had cesarean section and 31.5% had normal delivery, while mothers without pregnancy problem had 52.4% cesarean section and 47.6% normal delivery. Nevertheless, the cesarean section rate was significantly higher in mothers who experienced PIC (P-value=0.001). According to our results, 27% and 6.7% of mothers with and without PIC developed Premature Rupture of Membranes (PROM), respectively (P=0.012) (Figure 2).
Figure 2: Distribution of vaginal delivery, Cesarean section, in two
groups of mothers with and without PIC. Note:  Natural vaginal
delivery ,
Natural vaginal
delivery ,  Cesarean section ,
Cesarean section ,  Assisted delivery.
Assisted delivery.
In this study, maternal age was found to play a significant role in the incidence of preterm birth that older mothers were more likely to predispose to preterm delivery. In accordance with the present results, previous studies have demonstrated the direct impact of maternal aging on the increased chance of preterm delivery [18]. Jiang et al. [19], reported that the rate of preterm delivery was significantly higher in women over 35 years and adolescent mothers compared to mothers in other age ranging, and a U-shaped relationship of preterm birth risk and maternal age was observed. As noted by Faucett et al. [20], maternal aging does not increase the risk of preterm delivery by itself, indeed, they assumed that advanced maternal age potentially enhanced the risk of PICs such as placenta previa, intrauterine growth restriction, fetal death, gestational diabetes, gestational hypertension, preeclampsia, cesarean delivery, hence, maternal medical conditions related to increasing maternal age lead to preterm delivery.
Another remarkable finding showed that the incidence rate of prematurity was 4-folded higher in those experienced PICs. These statistics lend support to the view that PICs made a notable contribution to preterm delivery and are consistent with data obtained in previous studies that have confirmed a correlation between PICs and increased risk of preterm birth. Etuk et al. [21], identified mothers with PIC to be considerably prone to preterm delivery. Similarly, Morisaki et al. [22], have recognized preterm delivery as one of the detrimental consequences of highrisk pregnancy. Another study demonstrated that women with a history of diabetes, thyroid dysfunction, and heart disease were 2.3 times more likely to give birth prematurely than good medical conditions mothers [23]. In accord with the present study, another observation reported that pregnancy complications lead to an increased chance of preterm delivery by up to 6-16 times compared to women with a regular prenatal period [24]. To determine the effects of PICs, Wagura et al. [25], shown the risk of preterm birth increased 8-fold in mothers who developed pregnancy-induced hypertension and 4-fold in mothers who sustained antepartum hemorrhage. As mentioned above, apparently, maternal medical conditions are considered substantial contributors to preterm delivery, which occasionally can directly lead to preterm delivery, and in some cases, indirectly as consequences of treatment are able to pose preterm birth.
Another noteworthy finding indicates that PROM was four times higher in mothers diagnosed with PICs than healthful mothers. A parallel study established a connection between maternal medical conditions and PROM, which is higher 3-5 times in mothers with PICs in comparison with healthy ones [25]. A possible explanation for this might be due to the principal mechanism of PROM that refers to choriodecidual infections and inflammation and a reduction in the collagen of fetal membranes. Factors predisposing to PROM include a history of PROM, Maternal addiction, Urinary tract infection during pregnancy, Maternal diabetes, Preeclampsia, placental abruption, polyhydramnios, multiple pregnancies, Trauma, and genetic, nutritional, and enzymatic disorders which potentially pose challenges on pregnancy and enhanced the risk of PROM that lead to preterm delivery and its deleterious outcome [26,27].
A higher incidence of cesarean delivery was observed in the mothers who represented PICS rather than the control group. In a large longitudinal study on 2496 cesarean deliveries by Pallsmaa et al. [28], it was shown that 27% of pregnant women experience pregnancy-induced complications, and 10% of them are diagnosed with severe complications. These results are in agreement with those obtained by Persson et al. [29], which showed the remarkable link between gestational diabetes and the cesarean section, which was considerably higher in this population. These findings match those observed in a study conducted by Grandi et al. [30].
Another finding to emerge from the analysis is that the first Apgar score in newborns of the high-risk pregnancy group was significantly lower than neonates born to mothers without PICs. Apgar score commonly has been used to represent neonatal health conditions, which are typically measured 1,5, and 10 minutes after birth. It is widely well-known that a low Apgar score, generally defined as a score below 7, is associated with an increased risk of neonatal mortality [31]. In agreement with the current study, Bayoumi et al. [32], reported a relationship between low first Apgar and preeclampsia. In the study conducted by Grandi et al. [30], on the preterm population, comparable to our results, there is no affiliation between the fifth Apgar score of neonates and gestational diabetes.
The Finally yet importantly relevant finding showed that weight, height, and head circumference at the birth of preterm infants with an abnormal prenatal period were significantly lower than preterm infants in the normal prenatal period. Comparison of the range of neonatal anthropometric indices with those of other studies confirmed the akin neonatal weight range [33-35]. In findings represented by Bayoumi et al. [32], the low mean weight, height, head circumference, and gestational age at birth were noticeably related to preeclampsia. Correspondingly, multivariate logistic regression showed a strong relationship between gestational age, birth weight, height, and preeclampsia [32]. Sirenden et al. [36], demonstrate that the rate of preterm birth, low birth weight, and fetal complications were substantially higher in the group of neonates born to severe preeclampsia accompanying other maternal medical conditions. To determine the consequence of preeclampsia on neonates, Eviston et al. [37], demonstrated that low height and weight at birth were statistically related to preeclampsia. Surprisingly, after adjusting the confounding factors, increased head circumference at birth was observed in neonates born to mothers who experienced preeclampsia [37]. Another study indicated a relationship between the higher weight and gestational week at birth and gestational diabetes [38].
According to the results of our study, Respiratory Distress Syndrome was approximately 1.5 times more common in preterm infants with PIC (P=0.001) . In the study by Liu et al. [39], Diabetes in mothers during pregnancy was associated with an increased risk of RDS in infants. In a study revealed that maternal preeclampsia slightly increases the risk of severe RDS in VLBW infants [40].
The scope of this study was limited in terms of the retrospective nature of the study. Since the data were extracted from the medical records of neonates and mothers, it was not possible to assess other relevant factors naming economic and social status, maternal nutrition, etc. The study was performed on 950 eligible preterm infants. 79.7% of them were divided into those whose mothers were diagnosed with PIC and 20.3% whose mothers had a wholesome pregnancy period. This study has shown that pregnancy complications adversely pose the risk of severe consequences such as preterm delivery, cesarean section, PROM, Lower weight and gestational age and RDS. In the light of our findings, proper control of high-risk mothers may face the prospect of adverse outcomes.
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Hassan B, Fatemeh B (2022) Pregnancy-Induced Complications and Neonatal Outcome. Pediatr Ther. 12:459.
Received: 05-Jul-2022, Manuscript No. PTCT-22-18374; Editor assigned: 07-Jul-2022, Pre QC No. PTCT-22-18374 (PQ); Reviewed: 21-Jul-2022, QC No. PTCT-22-18374; Revised: 28-Jul-2022, Manuscript No. PTCT-22-18374 (R); Published: 08-Aug-2022 , DOI: 10.35841/2161-0665.22.12.459
Copyright: © 2022 Hassan B, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.