Chemotherapy: Open Access
Open Access
ISSN: 2167-7700
ISSN: 2167-7700
Research Article - (2024)Volume 12, Issue 4
Objective: This study aims to evaluate the preoperative Neutrophil-To-Lymphocyte Ratio (NLR) and ultrasound tumor characteristics to identify risk factors for Central Lymph Node Metastasis (CLNM) in clinically lymph Node-Negative (cN0) Papillary Thyroid Carcinoma (PTC) patients. Based on these risk factors, a nomogram predictive model is developed to aid in formulating individualized treatment plans for clinical practice.
Methods: A retrospective analysis was conducted on 471 patients who underwent surgery and were pathologically diagnosed with PTC in our hospital between January 2021 and January 2022. Preoperative clinical data and ultrasound findings were collected, including NLR from routine blood tests, age, gender, maximum tumor diameter, tumor location, laterality (unilateral or bilateral), aspect ratio, tumor margin, presence of calcifications, tumor relationship with the thyroid capsule, preoperative Thyroglobulin (TG) and Thyroid-Stimulating Hormone (TSH). Based on the presence of CLNM, patients were categorized into a metastasis group and a non-metastasis group. Univariate and multivariate analyses were conducted using Statistical Package for the Social Sciences (SPSS) software to identify independent risk factors for CLNM. The patients were randomly divided into a training group and a validation group in a 7:3 ratio. Receiver Operating Characteristic (ROC) curves, calibration plots and decision curve analysis were generated using R software to assess the feasibility of the predictive model.
Results: Among the 471 PTC patients, 215 cases (45.6%) were confirmed to have CLNM. Univariate analysis showed that factors such as gender, NLR, tumor diameter, tumor margin, calcifications, aspect ratio, tumor location, tumor relationship with the thyroid capsule, laterality and TG levels were associated with CLNM. Multivariate logistic regression identified male gender, higher NLR, larger tumor diameter, irregular tumor margins, microcalcifications and tumor invasion of the thyroid capsule as significant risk factors for CLNM in PTC patients. Based on these findings, a personalized nomogram was constructed and validated internally in two cohorts. The areas under the ROC, AUC for the training and validation groups were 0.836 and 0.825, respectively, indicating good discriminatory power. Hosmer- Lemeshow test results demonstrated good model calibration in both groups. Calibration curves further confirmed the model's predictive accuracy.
Conclusion: High NLR, microcalcifications, irregular tumor margins, tumor diameter >1 cm, thyroid capsule invasion and male gender are independent risk factors for CLNM in PTC patients. The predictive model constructed based on these factors can significantly predict the probability of CLNM in PTC patients. This non-invasive tool will aid in preoperative lymph node assessment and provide effective guidance for surgeons in developing individualized treatment plans.
Papillary thyroid carcinoma; Central lymph node metastasis; Neutrophil-Lymphocyte Ratio (NLR); Ultrasound; Predictive model
Thyroid cancer is one of the fastest-growing malignant tumors globally and it is also the most common endocrine malignancy [1]. According to the 2020 global epidemiological report on thyroid cancer, the age-standardized incidence rate of thyroid cancer worldwide is 10.1 per 100,000 people, with 3.1 per 100,000 in males. The age-standardized mortality rate is 0.5 per 100,000 in females and 0.3 per 100,000 in males [2]. The rate of increase surpasses that of any other cancer. In China, the estimated number of newly diagnosed thyroid cancer cases in 2015 was 200,700, accounting for 5.11% of all newly diagnosed cancer cases, making it the seventh most common cancer. The crude incidence rate of thyroid cancer in 2015 was 13.17 per 100,000 people, a significant increase compared to 4.30 per 100,000 in 2005 [3]. This rapid rise in incidence has been partly attributed to the widespread adoption of health check-ups, leading to an increase in detection rates. However, some studies suggest that despite the increase in detection rates, the proportion of advanced-stage thyroid cancer has not significantly decreased, further confirming the rapid growth in thyroid cancer incidence [4].
Papillary Thyroid Carcinoma (PTC) is the most common histological subtype of thyroid cancer, accounting for approximately 80-85% of all thyroid cancer cases. The 10-year survival rate for PTC exceeds 90% [5]. Despite the favorable prognosis and high survival rates compared to many other malignancies, an average of 15.3% to 49.3% of PTC patients experience tumor metastasis to the cervical lymph nodes [6]. The most common site for lymph node metastasis in PTC is the central compartment (level VI) and the high incidence of Central Lymph Node Metastasis (CLNM) has led some experts to suggest that Prophylactic Central Lymph Node Dissection (PCLND) may reduce the risk of tumor recurrence [7]. Performing CLND aids in postoperative staging and guides further treatment. Therefore, the Chinese guidelines recommend routine ipsilateral central lymph node dissection for PTC patients [8]. However, the 2015 American Thyroid Association (ATA) guidelines do not recommend PCLND for clinically lymph Node- Negative (cN0) patients. The benefit-risk ratio of PCLND in cN0 patients remains controversial [9]. Some studies have shown that PCLND does not improve prognosis and may increase the risk of postoperative complications, suggesting that PCLND should not be routinely performed. A study of 11,569 cN0 PTC patients reported that PCLND did not reduce the local recurrence rate or improve long-term survival, but instead increased the risk of complications such as recurrent laryngeal nerve injury and hypoparathyroidism [10]. Therefore, accurately assessing the lymph node status of PTC patients before surgery is critical for determining whether PCLND should be performed.
Recent advances and study rationale
In recent years, research has shown a close association between inflammation and cancer progression, including tumor initiation, promotion, malignant transformation, invasion and metastasis [11]. As early as the 19th century, discovered the presence of leukocytes in tumor tissues, establishing a link between chronic inflammation and malignancy [12]. The preoperative Neutrophil-To-Lymphocyte Ratio (NLR), calculated from the absolute neutrophil and lymphocyte counts in routine preoperative blood tests, has emerged as a biomarker reflecting both tumor and inflammation status. NLR may also indicate the overall systemic inflammatory response and the immune status of patients. Numerous studies have demonstrated that elevated NLR is associated with higher recurrence or mortality rates in cancers such as lung cancer, gastric cancer, pancreatic cancer, colorectal cancer, hepatocellular carcinoma and breast cancer [13]. Therefore, NLR is applicable across a wide range of solid tumors in clinical settings. Studies have indicated that thyroid cancer patients exhibit higher NLR levels compared to those with benign thyroid nodules and that patients with lymph node metastasis present with higher NLR levels than those without metastasis [14]. Furthermore, elevated NLR levels in patients with differentiated thyroid cancer are associated with larger tumors and a higher risk of recurrence. Taken together, these findings suggest that elevated NLR levels hold diagnostic value for lymph node metastasis in thyroid cancer patients. Given that routine blood tests are a standard and easily accessible preoperative examination, the assessment of preoperative NLR has the potential to improve the diagnostic accuracy for Central Lymph Node Metastasis (CLNM).
Current methods for diagnosing lymph node metastasis in preoperative thyroid cancer patients primarily include ultrasound, preoperative lymph node biopsy, Computed Tomography Scan (CT) and Magnetic Resonance Imaging (MRI). Although advancements in diagnostic equipment and techniques have been made, no preoperative examination can accurately assess lymph node metastasis in thyroid cancer with high precision. While ultrasound evaluation of the central compartment lymph nodes is limited by interference from surrounding tissues and gas, certain features of the primary thyroid tumor on ultrasound can help identify highrisk factors for lymph node metastasis. Studies have shown that a tumor size greater than 1 cm, microcalcifications, capsular invasion and abundant blood flow are significant clinicopathological risk factors for CLNM in PTC patients [15]. Wu et al., reported that ultrasound features, including nodule morphology and color Doppler flow patterns, can predict cervical lymph node metastasis in PTC patients [16]. These predictive factors may help compensate for the low sensitivity of preoperative imaging, aiding in the identification of aggressive PTC phenotypes.
In this study, we aim to analyze the risk factors for central lymph node metastasis in cN0, PTC patients using preoperative examinations. By accurately assessing lymph node metastasis and developing a predictive model, we seek to reduce the rate of missed diagnoses of lymph node metastasis, improve patient prognosis and minimize complications, ultimately aiding in the formulation of more precise, individualized treatment plans for clinical practice.
Study subjects
A total of 471 patients with clinically lymph cN0 Papillary Thyroid Carcinoma (PTC) who underwent either unilateral thyroidectomy or total thyroidectomy combined with ipsilateral Central Lymph Node Dissection (CLND) at the department of thyroid surgery in our hospital between January 2021 and January 2022 were retrospectively collected [17]. The cN0 criteria were as follows:
• No palpable lymph nodes or lymph nodes with a maximum diameter <2 cm on clinical examination.
• No evidence of enlarged lymph nodes on imaging or lymph nodes with a maximum diameter <1 cm or a maximum diameter between 1 cm-2 cm but with an aspect ratio >2, regular morphology, clear corticomedullary demarcation and without punctate microcalcifications or central liquefactive necrosis.
Patients with unilateral disease and no evidence of lateral compartment lymph Node Metastasis (cN0) underwent unilateral thyroid lobectomy combined with CLND. For patients with bilateral thyroid cancer, Total Thyroidectomy (TT) combined with bilateral central lymph node dissection was performed. The central lymph node dissection boundaries were as follows: The upper boundary at the hyoid bone, the lower boundary at the superior border of the innominate artery and the lateral boundaries at the medial edge of the common carotid arteries. Routine dissection included prelaryngeal, pretracheal and lymph nodes anterior to the recurrent laryngeal nerve on the left side and additionally, the lymph nodes posterior to the recurrent laryngeal nerve on the right side.
Inclusion criteria
• No previous history of thyroid surgery or radioactive iodine (I-131) treatment.
• Preoperative CT and ultrasound examinations consistent with cN0 PTC.
• All patients underwent unilateral thyroidectomy and prophylactic central lymph node dissection.
• Postoperative pathology confirmed the diagnosis of papillary thyroid carcinoma.
• Complete blood count performed within one week before surgery.
• No infectious diseases within one month before surgery.
• Complete clinical data available.
Exclusion criteria
• Presence of acute or chronic specific or nonspecific infectious diseases.
• Patients with immunodeficiency or hematological diseases.
• Patients with Hashimoto's thyroiditis, subacute thyroiditis or other conditions that could alter the white blood cell count and distribution.
• Patients with other malignant tumors.
• Patients undergoing reoperation for recurrent thyroid tumors.
• Patients with incomplete clinical data.
C-tirads classification standards and laboratory data acquisition criteria
The classification system proposed by Kwak et al., was used to categorize and record tumor characteristics, including tumor margin (smooth, irregular, or indistinct), calcification (macrocalcification >1 mm or microcalcification ≤ 1 mm), shape (aspect ratio ≥ 1 or <1), laterality (unilateral or bilateral), tumor location (upper, middle, lower pole, or isthmus) and blood flow (categorized as strip-like, spot-like, or absent) [18]. For each patient, one lesion was selected:
• For a solitary nodule, the corresponding lesion from the ultrasound examination was used.
• For multiple nodules, the lesion with the highest TIRADS classification on ultrasound was selected and the corresponding pathology report was used for analysis.
The tumor relationship with the thyroid capsule was assessed according to the four ultrasound criteria proposed by Kamaya et al., to evaluate capsular invasion: 1) Contact between the nodule and capsule, 2) Outward bulging of the capsule contour, 3) Absence of capsule contour and 4) Extension of nodule vessels beyond the capsule [19]. Capsular invasion was defined as a tumor adjacent to the capsule, regardless of whether capsule echogenicity was interrupted.
All laboratory data were obtained from tests performed within one week before surgery, including fasting complete blood count with differential, Thyroglobulin (TG) and Thyroid-Stimulating Hormone (TSH). NLR was calculated as the absolute neutrophil count divided by the absolute lymphocyte count. Age was categorized into ≥ 55 years and <55 years according to the 8th edition of the American Joint Committee on Cancer (AJCC) staging system.
Statistical methods
The collected data were analyzed using SPSS 25.0 and R software. Continuous data with a normal distribution were expressed as mean ± standard deviation (x̄ ± s) and comparisons between groups were conducted using the independent sample t-test. For non-normally distributed data, the median (interquartile range) (M (Q1, Q3)) was used and the Mann-Whitney U test was applied for group comparisons. Categorical data were expressed as counts and percentages (n (%)) and comparisons between groups were performed using the chi-square (χ2) test, continuity correction χ² test or Fisher’s exact test for univariate analysis.
Variables with statistical significance in univariate analysis were included in a binary logistic regression model for multivariate analysis, using forward stepwise selection (entry criterion p<0.05) to identify independent risk factors associated with CLNM. The 471 PTC patients were randomly divided into a training group and a validation group in a 7:3 ratio using R software. A nomogram was constructed using R software (version 4.0.1) to establish a predictive model for CLNM in papillary thyroid carcinoma. The diagnostic accuracy of the model was evaluated using Receiver Operating Characteristic (ROC) curves. The model's goodness-offit was assessed with calibration plots and its clinical utility and risk-benefit ratio were validated using decision curve analysis.
Basic clinical data
A total of 471 patients with postoperative pathological confirmation of PTC were included in the study, of which 215 cases (45.6%) showed Central Lymph Node Metastasis (CLNM) and 256 cases (54.4%) did not. Among them, 364 patients (77.3%) were female and 107 patients (22.7%) were male. The age range was 19-80 years. According to the 8th edition of the American Joint Committee on Cancer (AJCC) staging system, 347 patients (73.7%) were classified as younger than 55 years and 124 patients (26.3%) were 55 years or older. Tumor sizes ranged from 2 to 52 mm, with 325 patients (69.0%) having a tumor diameter ≤ 10 mm and 146 patients (31.0%) having a tumor diameter >10 mm.
Regarding the laterality of cancer lesions, 405 patients had unilateral lesions and 66 patients had bilateral lesions. Tumor location was distributed as follows: Upper pole (108 cases), middle pole (220 cases), lower pole (128 cases), and isthmus (15 cases). Preoperative ultrasound indicated smooth tumor margins in 245 cases and irregular or blurred margins in 226 cases. Capsular invasion was observed in 257 patients, while 214 patients had no capsular invasion. Tumor microcalcification was present in 160 cases and absent in 311 cases. The aspect ratio was <1 in 194 cases and ≥ 1 in 277 cases. Blood flow patterns on ultrasound were categorized as no detectable blood flow in 115 cases, spot-like blood flow in 129 cases and strip-like blood flow in 227 cases. The median ThyroGlobulin (TG) level was 11.4 ng/mL (interquartile range: 5.59-22.93 ng/mL) and the median Thyroid-Stimulating Hormone (TSH) level was 1.48 Uiu/mL (interquartile range: 1.04-2.18 Uiu/mL).
The NLR values ranged from 0.01 to 9.95, with a median value of 1.91. For this continuous variable, we assumed a linear relationship between the probability of CLNM and NLR values. However, in cases of extreme values such as NLR of 9.95 without corresponding lymph node metastasis, this could influence the overall NLR level. To minimize the impact of individual outcomes on the model, the NLR values were stratified according to the optimal cutoff point for the relationship between NLR and CLNM, converting NLR into a categorical variable. Based on the relationship between NLR and lymph node metastasis in PTC patients, the Receiver Operating Characteristic (ROC) curve was plotted, with an Area Under the Curve (AUC) of 0.640, a maximum Youden index of 0.276, p <0.001, a sensitivity of 65.1% and a specificity of 62.5%. The optimal cutoff value for NLR was 1.905. Accordingly, patients were divided into two groups: The low NLR group (NLR ≤ 1.905) with 237 patients (50.3%) and the high NLR group (NLR >1.905) with 234 patients (49.7%).
Analysis of preoperative NLR and clinicopathological features
Statistically significant differences were observed between different NLR levels in terms of the presence of CLNM, tumor diameter and tumor laterality (unilateral or bilateral lesions) (p<0.05). However, no significant differences were found in terms of gender or age (p>0.05) (Table 1). These results indicate a correlation between preoperative NLR and CLNM.
| NLR | P | |||
|---|---|---|---|---|
| Low-level | High-level | |||
| CLNM | - | - | c2=31.188 | <0.001 |
| Positive | 78 | 137 | - | - |
| Negative | 159 | 97 | - | - |
| Primary tumor size(mm) | - | - | c2=6.130 | 0.013 |
| <10 | 175 | 148 | - | - |
| ≥ 10 | 62 | 86 | ||
| Gender | - | c2=0.001 | 0.972 | |
| Female | 183 | 181 | - | - |
| Male | 54 | 53 | - | - |
| Age | - | - | c2=1.376 | 0.241 |
| <55 | 169 | 178 | - | - |
| ≥ 55 | 68 | 56 | ||
| Bilateral | - | - | c2= 5.979 | 0.014 |
| No | 192 | 213 | - | - |
| Yes | 24 | 42 | - | - |
Table 1: Relationship between NLR and clinicopathological features of patients.
Univariate analysis of risk factors for central lymph node metastasis
Univariate analysis of clinical data between the CLNM group and the non-metastatic group revealed that factors such as NLR, gender, preoperative ultrasound tumor diameter, tumor location, tumor laterality, tumor margins, capsular invasion, calcification status, tumor aspect ratio and TG levels were associated with CLNM in PTC patients. Conversely, no significant differences were found for age, blood flow status or TSH levels (Table 2).
| Positive or negative for CLNM | P | |||
|---|---|---|---|---|
| Positive | Negative | |||
| NLR | - | - | c2=31.188 | <0.001 |
| Low-level | 159 | 78 | ||
| High-level | 97 | 137 | - | - |
| Gender | - | - | c2=8.438 | 0.004 |
| Female | 211 | 153 | - | - |
| Male | 45 | 62 | ||
| Primary tumor size (mm) | - | - | c2=82.298 | <0.001 |
| ≤ 10 | 222 | 103 | - | - |
| >10 | 34 | 112 | - | - |
| Tumor location | c2=7.922 | 0.048 | ||
| Lowe | 57 | 71 | - | - |
| Middle | 131 | 89 | ||
| Upper | 61 | 47 | ||
| Isthmus | 7 | 8 | ||
| Bilaterality | c2=8.396 | 0.004 | ||
| No | 231 | 174 | ||
| Yes | 25 | 41 | ||
| Invasion of thyroid capsule | - | - | c2=57.138 | <0.001 |
| No | 157 | 57 | - | - |
| Yes | 99 | 158 | - | - |
| irregular margins | c2=30.522 | <0.001 | ||
| No | 163 | 82 | - | - |
| Yes | 93 | 133 | - | - |
| Microcalcifcation | - | - | c2=67.182 | <0.001 |
| No | 211 | 100 | - | - |
| Yes | 45 | 115 | - | - |
| Taller than wide shape | - | - | c2=9.552 | 0.002 |
| <1 | 89 | 105 | - | - |
| ≥ 1 | 168 | 100 | - | - |
| Age | - | - | c2=0.935 | 0.334 |
| <55 | 184 | 163 | - | - |
| ≥ 55 | 72 | 52 | - | - |
| Blood flow signal | - | - | c2=5.461 | 0.065 |
| No | 73 | 42 | - | - |
| Mottling | 69 | 60 | - | - |
| Slender | 114 | 113 | - | - |
| TG(ng/ml) M(Q1,Q3) | 11.15(5.79-20.93) | 12.05(6.7-24.15) | Z=-0.353 | 0.02 |
| Tsh(Uiu/ml) M(Q1,Q3) | 1.48(1.03-2.14) | 1.50 (1.17-2.15) | Z=-0.048 | 0.962 |
Table 2: Results of univariate analysis of central lymph node metastasis in papillary thyroid carcinoma.
Multivariate analysis using binary logistic regression
The following the univariate analysis, variables with statistical significance, including gender, tumor diameter, tumor location, presence of microcalcifications, aspect ratio, tumor margins, laterality, capsular invasion, NLR and TG, were included in the binary logistic regression analysis. Using forward stepwise analysis, variables such as tumor aspect ratio, tumor laterality and TG were excluded as non-significant factors. The final results identified male gender, larger tumor diameter, the presence of microcalcifications, irregular tumor margins, elevated NLR and capsular invasion as independent risk factors for CLNM in PTC patients (Table 3).
| Variable | B | SE | Wald | P | |
|---|---|---|---|---|---|
| Gender | F/M | 0.863 | 0.287 | 9.044 | 0.003 |
| Primary tumor size(mm) | ≤ 10/>10 | 1.163 | 0.287 | 16.451 | <0.001 |
| Lower | - | - | 7.515 | 0.057 | |
| Middle | -0.779 | 0.298 | 6.862 | 0.009 | |
| Tumor location | Upper | -0.45 | 0.34 | 1.741 | 0.187 |
| isthmus | 0.005 | 0.668 | 0.001 | 0.994 | |
| Microcalcifcation | Yes/No | 1.255 | 0.25 | 25.099 | <0.001 |
| Taller than wide shape | <1/≥ 1 | 0.249 | 0.221 | 1.264 | 0.261 |
| irregular margins | Yes/No | 0.966 | 0.237 | 16.575 | <0.001 |
| Bilateral | Yes/No | 0.005 | 0.373 | 0.001 | 0.99 |
| NLR | Low-level/High-level | 1.073 | 0.24 | 20.022 | <0.001 |
| Invasion of thyroid capsule | Yes/No | 1.104 | 0.247 | 19.948 | <0.001 |
| TG | - | 0.002 | 0.002 | 1.037 | 0.309 |
| - | - | -2.368 | 0.329 | 51.955 | <0.001 |
Table 3: Results of binary logistic regression analysis.
Construction of the nomogram predictive model
Based on the independent risk factors identified in the multivariate logistic regression analysis, six significant factors were selected: Male gender, tumor diameter ≥ 10 mm, presence of microcalcifications, irregular tumor margins, elevated NLR levels and capsular invasion. These factors were visually integrated into a nomogram to predict the probability of Central Lymph Node Metastasis (CLNM) in clinically lymph Node-Negative (cN0) PTC patients.
By using the nomogram, clinicians can calculate the predicted probability of CLNM by assigning a score to each predictive factor based on preoperative examination results. The scores for each factor are summed to obtain a total score. A vertical line is then drawn from the total score to the “Diagnosis Rate” axis to determine the predicted probability of CLNM for the patient (Figure 1).

Figure 1: Nomogram for predicting the risk of CLNM in PTC patients. Note: Gender=1: Female; Gender=2: Male; Diameter=1: Tumor diameter ≤ 1 cm; Diameter=2: Tumor diameter >1 cm; Calcification=0: No microcalcification; Calcification=2: Presence of microcalcification; Margin=0: Smooth margins; Margin=1: Irregular margins; NLR=1: Low NLR; NLR=2: High NLR; Thyroid capsule=0: No invasion; Thyroid capsule=1: Invasion present.
Evaluation of the nomogram
The model's discriminative ability was evaluated using the area under the Receiver Operating Characteristic (Roc) AUC, which measures the model’s capacity to effectively differentiate between patients at varying risk levels of developing CLNM. The 471 patients were randomly divided into a training group (329 patients) and a validation group (142 patients) in a 7:3 ratio. The AUC for the training group was 0.836, while the AUC for the validation group was 0.825, indicating good discriminative power of the model (Figures 2 and 3).

Figure 2: AUC curve for the training group.
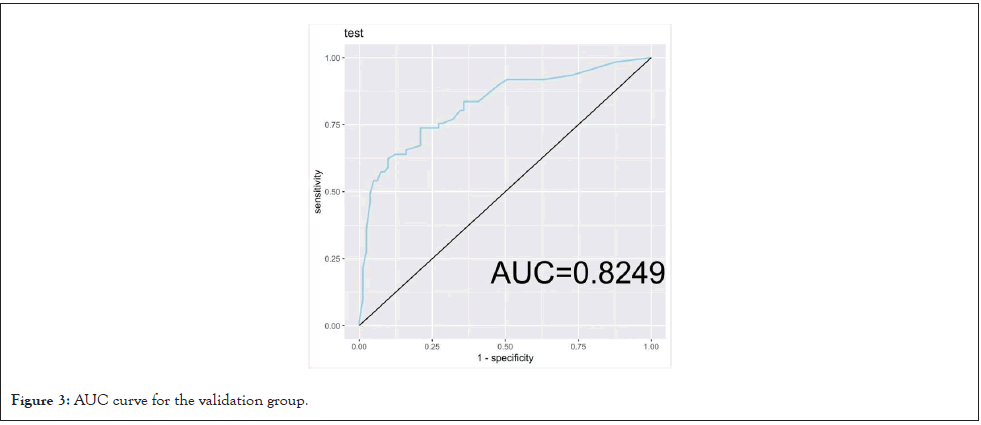
Figure 3: AUC curve for the validation group.
Calibration and validation of the nomogram model
The calibration of the nomogram model was assessed using the bootstrap resampling method, with 1,000 resamples to generate calibration curves. These curves demonstrated that the predicted probability of CLNM closely matched the actual probability of CLNM in both the training and validation groups (p=0.949), indicating good calibration.
In Figures 4 and 5, the x-axis represents the predicted probability of CLNM from the nomogram, while the y-axis represents the actual probability of CLNM occurrence. The 45°C dashed line represents a perfect prediction, where the predicted outcomes align exactly with the actual outcomes. The solid line reflects the calibration of the nomogram model. The closer the solid line is to the 45°C line, the better the model’s fit and the higher its predictive accuracy. Both the training and validation groups showed good calibration (p=0.949).
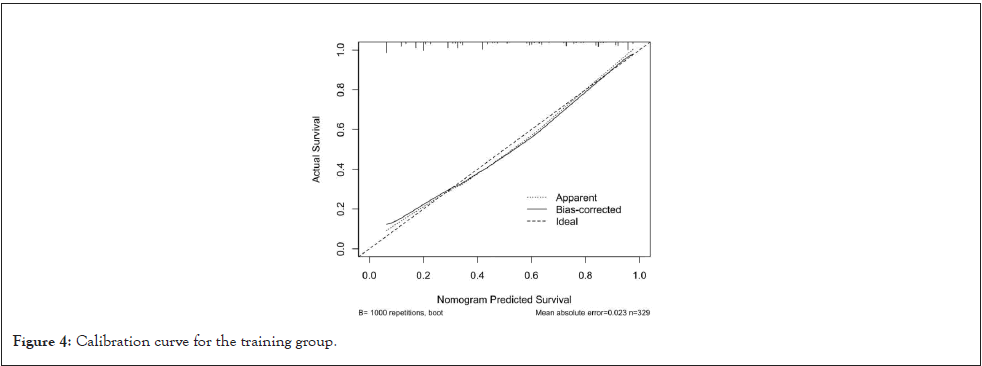
Figure 4: Calibration curve for the training group.
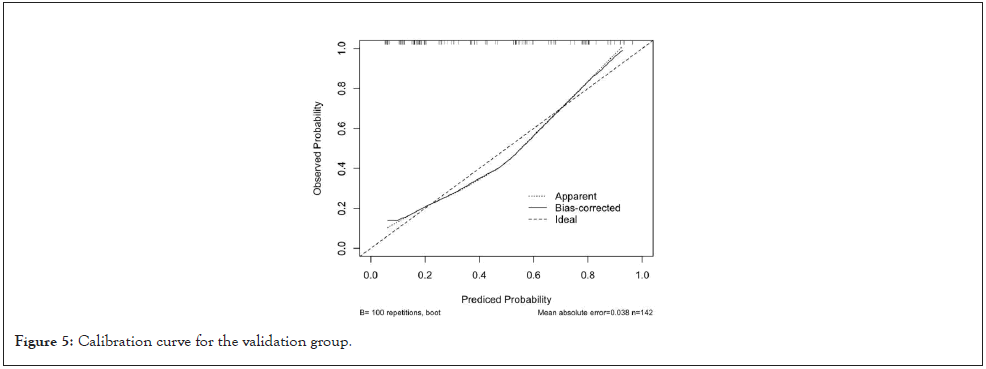
Figure 5: Calibration curve for the validation group.
Clinical decision curve analysis
To evaluate the clinical utility of the nomogram model for deciding when to perform Prophylactic Central Lymph Node Dissection (PCLND) in PTC patients, decision curve analysis (Figure 6) was performed. The x-axis represents the threshold probability and the y-axis represents the net benefit. In addition to the axes, two reference lines are shown: The "All" line represents the net benefit if all cN0 PTC patients undergo PCLND, while the "None" line represents no intervention for any patient. The red and blue lines represent the decision curves for the training and validation groups, respectively.
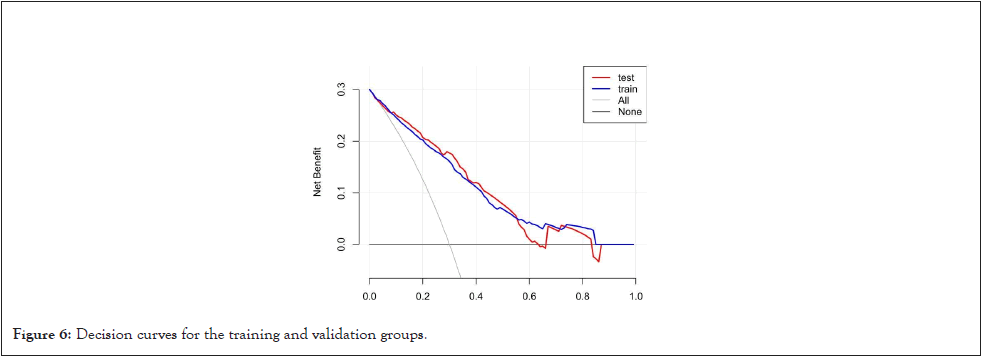
Figure 6: Decision curves for the training and validation groups.
The decision curves demonstrate that, for both the training and validation groups, the net benefit of using the predictive model is higher than that of performing PCLND on all patients or none at all. This indicates that the model has good clinical value, as it provides a more individualized and effective decision-making tool for PCLND intervention in cN0 PTC patients.
With improvements in living standards and advances in diagnostic techniques, the incidence of PTC has been steadily increasing. PTC generally exhibits non-invasive behavior and has an excellent prognosis, with a 10-year overall survival rate as high as 96% and a 15-year overall survival rate exceeding 87% [20,21]. Some authors have suggested that the examination, diagnosis and management of PTC should be adjusted to account for the fact that many thyroid cancers are low-risk and do not require immediate or aggressive intervention [22]. Despite the generally favorable prognosis, some PTC cases follow a clinically aggressive course. In our study, nearly 50% of PTC patients had Central Lymph Node Metastasis (CLNM), consistent with literature reports showing lymph node involvement in 20%-50% of cases. Even small primary tumors confined to the thyroid can exhibit metastatic potential [23].
Our goal is to distinguish patients at higher risk of lymph node metastasis to balance risks and benefits and develop more personalized treatment plans to improve disease outcomes.
The central lymph nodes are sentinel nodes for thyroid cancer metastasis, but there remains a lack of accurate methods for detecting lymph node involvement preoperatively. Ultrasound, the most commonly used imaging tool for preoperative assessment of thyroid cancer, has limitations in evaluating metastatic lymph nodes, especially in the central compartment. The central lymph nodes are located deep in the neck and can be obscured by surrounding structures such as air, adipose tissue and bones, leading to poor detection rates. Additionally, it is often difficult to distinguish between metastatic and inflammatory hyperplastic lymph nodes in this region, as the typical features of metastatic lymph nodes, such as microcalcifications and central liquefactive necrosis, may be absent. Even with high-quality, high-resolution ultrasound performed by experienced radiologists, the detection rate for lymph nodes in this area is only 23.9% and the detection rate is closely related to lymph node size and ultrasound equipment capabilities [24-25]. Sensitivity is significantly reduced when lymph nodes are smaller than 9 mm [26].
Since early observations in cancer biology, the connection between inflammation and cancer has been long suspected. Numerous epidemiological, genetic and molecular studies have now confirmed this significant link. Inflammation plays a critical role in the initiation, maintenance and promotion of tumor growth [27]. Neutrophils can produce pro-inflammatory cytokines such as Vascular Endothelial Growth Factor (VEGF), Interleukins (IL-2, IL-6, IL-10) and suppress Tumor Necrosis Factor-Alpha (TNF-α) secretion, all of which are associated with lymph node metastasis and tumor progression. On the other hand, lymphocytes exert anti-tumor effects by monitoring the immune system and inducing tumor cell apoptosis [28].
This study focused on the interactions between cellular components in the tumor microenvironment. Our research demonstrated a positive correlation between preoperative NLR and PTC characteristics such as tumor size, lymph node metastasis and bilaterality. Furthermore, we evaluated preoperative NLR as a predictor of lymph node metastasis in PTC patients. Higher preoperative NLR was associated with a higher rate of lymph node metastasis, with the optimal NLR cutoff point identified as 1.905, similar to the 1.92 cutoff suggested by Ceylan et al. Ceylan also reported a correlation between high NLR and extrathyroidal extension in malignant thyroid tumors [28]. In this study, due to the wide range of NLR values, we divided patients into high and low NLR groups, excluding cases with extreme NLR values but no lymph node metastasis. ROC curve analysis was used to assess the diagnostic performance of NLR for lymph node metastasis, with an Area Under the Curve (AUC) of 0.640. Multivariate analysis confirmed high NLR as an independent risk factor for CLNM (OR=2.924, 95% CI: 1.828-4.679), indicating that high preoperative NLR has good predictive value for lymph node metastasis. Therefore, for patients with elevated preoperative NLR, the risk of lymph node metastasis should be carefully considered and PCLND may be warranted.
While NLR is easily obtained from routine preoperative blood tests, it has some limitations. NLR can be influenced by inflammatory diseases and hematologic conditions, reducing its specificity and potentially affecting the stability of predictive models. Furthermore, as a retrospective study, we were unable to completely rule out other diseases that might affect blood cell counts in preoperative patients. Future research will focus on controlling for such confounding factors to improve diagnostic accuracy.
Several studies have shown that, beyond gender-specific organs such as the uterus, prostate, ovaries and breasts, where gender differences in cancer incidence are easily explained, significant sex differences in incidence and survival rates are also observed in shared organs such as the thyroid, lungs and liver [29,30]. In this study, of the 471 PTC patients, 107 (22.7%) were male and 364 (77.3%) were female, with the proportion of females being three times higher than males. This finding is consistent with the global thyroid cancer epidemiology report from 2020, which indicated an age-standardized incidence rate of 10.1 per 100,000 women and 3.1 per 100,000 men globally. The explanation for this gender difference is often linked to the presence of estrogen receptors in the thyroid confirmed the presence of both α- and β-estrogen receptors in the thyroid gland. Although papillary thyroid carcinoma cells have lower levels of α-estrogen receptors, these levels can significantly increase under physiological estrogen stimulation, leading to the rapid growth of thyroid tumors (benign or malignant) during pregnancy. This may be one of the reasons why females constitute the majority of thyroid cancer patients.
However, male patients tend to exhibit more aggressive PTC progression. In a study which included 2,595 PTC patients, male patients had a higher risk of lymph node and distant metastasis and a greater risk of long-term recurrence [30]. The Salmonella Microsome Mutagenicity Assay (AMES) risk stratification system includes gender as a risk factor for long-term recurrence. In a multivariate analysis of Seasonal Energy Efficiency ratio (SEER) data from 1973-1981. Multivariate analysis confirmed that male gender is an independent risk factor for CLNM (OR=2.371, 95% CI: 1.351-4.136), consistent with previous research. Therefore, more attention should be given to the possibility of central lymph node metastasis in male PTC patients.
Ultrasound characteristics and CLNM
Neck ultrasound is a mainstay in PTC evaluation, providing valuable insights into tumor features such as size, margin clarity and calcifications [31]. High-resolution ultrasound has improved nodule detection, even down to 2 mm-3 mm. Certain ultrasound features, like microcalcifications, correlate strongly with malignancy and their presence in PTC has been linked to higher CLNM rates [32]. In our study, 71.9% of patients with microcalcifications had CLNM compared to 32.2% without them. Similarly, tumors with ill-defined margins had higher CLNM rates (58.9%) than those with clear margins (33.5%). Multivariate analysis confirmed these characteristics as independent CLNM risk factors, indicating ultrasound’s potential in preoperative CLNM risk prediction.
The role of PCLND in PTC remains a subject of debate, especially for low-risk patients. According to ATA guidelines, PCLND is not routinely recommended for T1-2N0M0 patients but may be considered in high-risk cases (T3, T4, or cN1a) [33]. Studies indicate that PCLND can reduce recurrence rates, but it also carries risks, such as hypocalcemia and recurrent laryngeal nerve damage [34,35]. Our findings support PCLND's utility in reducing recurrence for patients with higher CLNM risk. However, the decision should be individualized, considering the patient’s overall risk profile and potential complications.
Using independent risk factors identified in this study, we constructed a CLNM prediction model with an Area Under the Curve (AUC) of 0.836 for the training group and 0.825 for the validation group, indicating robust discriminatory capability. The model includes variables such as NLR, gender, tumor diameter, microcalcifications, and ill-defined margins. Calibration and net benefit analysis affirmed the model’s clinical relevance, suggesting it can serve as a practical tool in determining the need for PCLND. This model provides a step forward in risk-based surgical planning, but further validation in multicenter prospective studies is necessary to confirm its clinical utility.
Preoperative factors such as a higher NLR, presence of microcalcifications, irregular tumor margins, thyroid capsule invasion, tumor diameter greater than 1 cm and male gender are independent risk factors for Central Lymph Node Metastasis (CLNM) in patients with Papillary Thyroid Carcinoma (PTC). The clinical prediction model based on these factors can effectively predict CLNM in PTC patients. The newly developed nomogram demonstrates significant utility in helping surgeons manage Lymph Node Metastasis (LNM) in this patient subgroup and provides a basis for more individualized treatment plans.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and was approved by the ethics committee of Zhangzhou Affiliated Hospital of Fujian Medical University (No. 2024LWB362). All personal identifiers were removed from the data to ensure participant confidentiality.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All the authors have made significant contributions to the study design, data acquisition, analysis and interpretation. They have substantially participated in drafting the manuscript and critically revising the important content and assume responsibility for all aspects of this work. All authors contributed to the article and approved the submitted version.
This work was supported by the Natural Science Foundation of Fujian Province, China (Grant No. 2024J011562) and the Natural Science Foundation of Fujian Province, China (Grant No. 2023J011826).
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Chen M, Hong J, Lan J, Lyu G, Huang N, Zhou Y et al. (2024). Preoperative NLR Combined with Ultrasound to Construct a Predictive Model for Central Lymph Node Metastasis in cN0 Papillary Thyroid Carcinoma. Chemo Open Access.12:226
Received: 18-Nov-2024, Manuscript No. CMT-24-35344; Editor assigned: 20-Nov-2024, Pre QC No. CMT-24-35344 (PQ); Reviewed: 04-Dec-2024, QC No. CMT-24-35344; Revised: 11-Dec-2024, Manuscript No. CMT-24-35344 (R); Published: 19-Dec-2024 , DOI: 10.35248/2167-7700.24.12.226
Copyright: © 2024 Chen M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited