Journal of Biomedical Engineering and Medical Devices
Open Access
ISSN: 2475-7586
ISSN: 2475-7586
Research Article - (2021)Volume 6, Issue 11
Introduction: Human corona virus infection disease (COVID-19) has resulted in a global pandemic affecting millions of people. The maximum risk of spread of infection is during transport of these infected patients within hospital or to a hospital.
Materials and Methods: An idea of combining negative and positive pressure systems to devise a portable batteryoperated, vacuum chamber for transport of infected and non-infected patients was adapted in devising a transport chamber. The chamber was used for transport of COVID patients as trial run following which swabs were taken from inlet and outlet to rule out virus contamination of the chamber. The relatives accompanying the patient and healthcare workers (HCWs) involved were also tested for corona virus.
Results: The pressurized protective transport chamber (PPTC) was used in transport of 152 COVID patients in trial phase and 556 patients in total. The swabs taken from outlet and inlet of PPTC showed no viral contamination. Also 200 HCWs and 250 relatives were tested and all were negative for COVID infection.
Conclusion: PPTC is an effective method of transport of infected patients and will help in curtailing the spread of infection.
Negative pressure mode; Positive pressure mode; COVID-19, Health care workers; Infected; Immunocompromised.
When COVID-19 pandemic hit mankind, the whole world stood still and all health care workers were diverted towards COVID care [1]. COVID-19 virus being a severe acute respiratory syndrome (SARS) group of viruses is primarily transmitted through aerosols, also initially assumed to spread due to direct contact with the patients and contaminated surfaces [2]. Despite use of personal protective gears, increased rate of infection amongst Health Care Workers (HCWs) while treating COVID patients, it had a negative impact on the health care system which was attributed to exposure during transport of patients. A patient arriving at a hospital has to go through a process before getting admitted starting from registration counter to the ward. Once admitted the patient might require consultations from various doctors and might be shifted to radiology suite for imaging studies. This process of travelling within various departments of the hospital results in spread of infection especially in situations like the present COVID-19 pandemic. These infections affect not only the relatives and attendants of the patient but also healthcare workers (HCWs) involved in the treatment of these patients. This has been seen in the present pandemic where a greater number of HCWs have been affected by the disease Bandyopadhyay S, et al. [3]. This has resulted in increased mortality & morbidity among healthcare workers. To tackle this situation, we used the concept of negative pressure isolation rooms and airflow of operation theatres to device a transport system. The use of acrylic sheets for safe airway management has already been described in the literature [4,5]. Additional use of barrier, 'Aerosol Box' during intubation has shown good results in reducing spread of contaminants to the environment thus, preventing exposure of HCWs Gupta V, et al. [6]. Negative pressure isolation rooms have been advocated in the management of COVID-19 and other SARS group of virus infected patients to prevent spread of infection [7,8]. In order to achieve a safe isolation of the patient and to prevent spread of infection during transit, a PPTC having dual pressure mode system was developed.
The PPTC consists of both positive and negative pressure mode. The first significant point of difference between the two is that positive pressure mode systems protect the patient while negative protects the HCWs. This was designed in the initial days of COVID-19 pandemic. Its purpose was to prevent transmission to HCWs and bystanders. This transport system will be efficacious in preventing spread of infection and thereby reducing morbidity and mortality in pandemic situations.
The chamber is made up of acrylic sheets fused together to form an airtight hood and the whole assembly rests on a base made up of stainless steel. Fastened to the hood are rubber gloves enabling examination of patients from outside without coming in direct contact with the infected patient.
The 150 mm tall base is made up of 304 SS grade stainless steel which contains both positive and negative pressure duct systems, with incorporated high efficiency particulate air (HEPA) filters and UV- C tube.
Head end of the acrylic box has 2 ports – one is an oxygen valve and other is a swivel connector for ventilator connection.
Both lateral sides of acrylic box have been fastened with 5 gloves and 4 utility ports in which one can be used for ultrasonography probe and other 3 small ports for passage of intravenous tubing and cables of multipara monitor.
Positive pressure is achieved inside the chamber with high cubic feet/min (125l/minute) (cfm) flow inlet fans. This air is first filtered through HEPA filter at inlet hence aerosol particles and other potential contaminants in the surrounding environment do not enter the chamber (Figure 1).
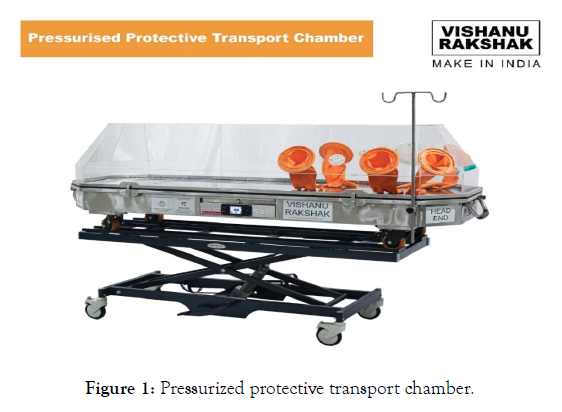
Figure 1: Pressurized protective transport chamber.
The achieved negative pressure inside the chamber prevents flow of air from inside to outside thus preventing spread of infective pathogens. The outlet duct enforced with HEPA filter traps most of the harmful bacteria and viruses. HEPA filters placed at the outlet vent are sterilized by continuous Ultraviolet-C light exposure.
The efficiency of the system was tested by serial swabs of the inlet and outlet ducts over the period of 12 months. The HCWs and attendants actively involved in transport of patients were subjected to COVID-RT-PCR test over a period of 12 months.
The transport chamber needs to be disinfected in between two successive transits by the spray of 1% hypochlorite solution with contact time of 1 to 10 min and Hepa filters being disinfected by use of UV-C light.
The HCWs involved in transportation of COVID-19 positive patients were tested for COVID-19 infection by COVID-RT-PCR Nasal and pharyngeal swabs after a vigorous use of this transport pod within hospital premises, ambulances over a period of 12 months. The HCWs were symptom free over this period and were tested negative for COVID-19 virus on RT-PCR. Along with HCWs the relatives of the patients were also tested and were found to be negative for COVID-19 infection.
The pressurized protective patient transport chamber (PPTC) was used in transport of 152 COVID patients in trial phase and a total of 556 patients. The swabs taken from outlet and inlet of PPTC showed no viral contamination. Total of 200 HCWs were tested and 250 relatives were tested and all were negative for COVID infection.
Manuscript
Initially there was an exponential rise in number of cases of COVID-19 which forced HCWs to work with limited man power. Many HCWs got infected while transporting and treating COVID positive cases. Thus, a dual pressurized transport chamber was developed to prevent infection of HCWs. Negative pressure mode of this chamber serves the purpose of transportation of infected and suspected patients.
Along with COVID-19 virus it is also an excellent transport facility in isolating patients with any airborne respiratory disease [8]. The negative pressure assembly, at head end creates negative pressure up to 45-50 Pa, and the high efficiency ‘nano protect HEPA filter’ clears the air that leaves patient compartment.(Christopherson et al., 2020)
This chamber allows safe transport also enabling examination and basic invasive procedures like catheterization, intubation, and intravenous access within an enclosed space without compromising the integrity of isolated system. It is the mainstay in protecting HCWs and preventing contamination of the environment with infectious aerosols. Positive and negative pressure systems that are maintained through closed-loop control the pressure inside this chamber.
Positive pressure mode is used to protect the patient inside the chamber from infectious environmental particles in which fans create pressure of +45 to +50 Pascal. Augmented HEPA filter at inlet valve prevents any contaminant from entering the chamber [8]. Head end with an oxygen valve and one swivel connector along with utility gloves allows accurate and swift airway management without compromising integrity and safety of the system. Other 3 attached gloves help in treating patients inside and aid in IV tubing manipulation, multipara monitor attachment, and even sonography probe manipulation. The design of the box has tried to overcome certain issues of difficult manipulation of laryngoscope, endotracheal tube and bougie and the box can be used in obese and patients with short neck too as it has an ergonomic design. This pressurized chamber - negative pressure mode will help in protecting the HCWs or even the surroundings and positive pressure mode for immunocompromised patients from environmental infection. However, an appropriate training on mannequin is important prior to use on patients to prevent any mishap during airway management in critically ill patients.
The portable rechargeable battery system without need of any power supply for time duration of 6-8 hours serves well for ambulance travels. It is technically challenging to create ambulances with negative pressure isolation facilities, this is where this compact, robust and ambulance compatible trolley comes in handy. This compact, robust and compatible chamber which can be easily fit into ambulances, air ambulances and can be used as an alternative to negative pressure isolation rooms.
Filtration system
Combines a pre-filter, a highly efficient HEPA- filter, and a UVCradiation source
Hepa filters: High efficiency particulate air filters.
● Filters entrap around 99.97% of air particles with diameter 0.3 microns and above.
● HEPA filters capture pollen, dirt, dust, moisture, bacteria (0.2-2 microns), virus (0.2-0.3 microns) and sub-micron liquid aerosol (0.02-0.5 microns)
● Pre-filters were used to increase durability of HEPA filter. Pre-filters entrap particles of size 10 micron and above from air before reaching HEPA filter.
● Air exchange per hour: An air exchange of 121 liters per minute is achieved despite the flow of air through the HEPA filter (Table 1).
| Battery Autonomy | 12V,36AH (6-8 hours battery backup) |
| Positive Pressure | +45 to +50 Pa |
| Negative Pressure | -45 to -50 Pa |
| Inlet Filtration | HEPA (Type 4) 0.02-0.03 Microns |
| Outlet Filtration | HEPA (Type 4) 0.02-0.03 Microns |
| Filtration Performance | 99.97% |
| Electrical Connections | 12VDC |
| Weight of Chamber (approx.) | 82kg |
| Seal Port for Medical Appliances | 3 |
| Manipulation Ports | 5 |
| Sterilizations of Filters | Integrated UV-C rays (15W) |
| (Do not use UVC light when patient is inside the chamber) | |
| Air Quality Index Sensor | To Calculate -Particulate matter count per million |
| Temperature and Humidity sensor | Gives us inside chamber temperature and humidity |
| Control screen touch board with screen | Control switch for pressure, UV-C, display and temperature, humidity, and ppm (particulate count matter per million) |
Table 1: Technical details.
Different modes and its Uses
Positive pressure mode: Positive pressure mode maintains a higher pressure inside the chamber with high cubic feet/min (125 L/ minute) (CFM) inlet fans. This air is first filtered through HEPA filter at inlet (Table 2).
| S.No | Pressure (Pascals) | Volume (Decibels) |
|---|---|---|
| 1. | 50 | 69.8 |
| 2. | 40 | 68.6 |
| 3. | 30 | 66.7 |
| 4. | 20 | 65 |
| 5. | 10 | 64.5 |
Table 2: Positive pressure noise readings.
Aerosol particles and other potential contaminants in the surrounding environment do not enter the chamber (Figure 2).
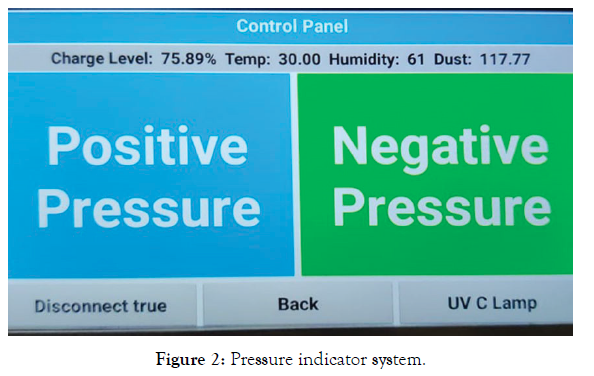
Figure 2: Pressure indicator system.
Advantages – Can be used in transportation of:
1. Immunocompromised individuals
2. Patients on immunosuppressant therapy
3. Post-transplant surgeries
4. Bubble child
Negative pressure mode: The achieved negative pressure inside the chamber prevents flow of air from inside to outside thus preventing spread of infective pathogens (Figure 2). The outlet duct enforced with HEPA filter ensures that the air expelled out of the system is made. HEPA filters placed at the outlet vent are sterilized by continuous UVC exposure (Table 3).
| S.No | Pressure (Pascals) | Volume (Decibels) |
|---|---|---|
| 1. | 50 | 70.1 |
| 2. | 40 | 68.6 |
| 3. | 30 | 67.6 |
| 4. | 20 | 64.5 |
| 5. | 10 | 63.5 |
Table 3: Negative pressure noise readings.
Advantages – Can be used for transport of:
1. COVID-19 positive patients
2. Tuberculosis patients
3. Viral and bacterial meningitis
4. EBOLA
Description of pressurised protective transport chamber
The chamber rests on a base of stainless steel and consists of a hood made up of acrylic sheets. Fastened to the hood are rubber gloves enabling examination of patients from outside without coming in direct contact with the infected patient.
• Dimensions of the box (Figure 1)
• Length of chamber (L)-2080 mm
• Width of chamber (W)-750 mm
• Height of chamber (H)-745 mm
The 150 mm tall base is made up of 304 SS grade stainless steel which contains both positive and negative pressure duct systems, with incorporated HEPA filters and UV-C tube.
Head end of the acrylic box has 2 ports – One is an oxygen valve and other is a swivel connector for ventilator connection (Figure 3).
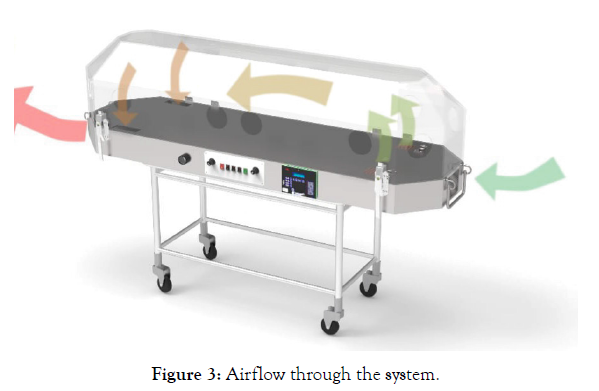
Figure 3: Airflow through the system.
Both lateral sides of acrylic box have been fastened with 5 gloves and 4 utility ports in which one can be used for ultrasonography probe and other 3 small ports for passage of intravenous tubing and cables of multipara monitor.
Decontamination and disinfection
The transport chamber needs to be disinfected in between two successive transits by the spray of 1% hypochlorite solution with contact time of 1 to 10 min and HEPA filters being disinfected by use of UVC light.
Efficiency of the system
In order to evaluate the efficiency of this system, the HCWs actively involved in transportation of this system were serially monitored over a period of 12 months for any sign and symptoms of COVID-19 and also subjected to COVID-19 RTPCR tests every 6 months. The transport chamber has been brought into use at 3 main tertiary COVID Care Centers in Mumbai (Figures 4 and 5).
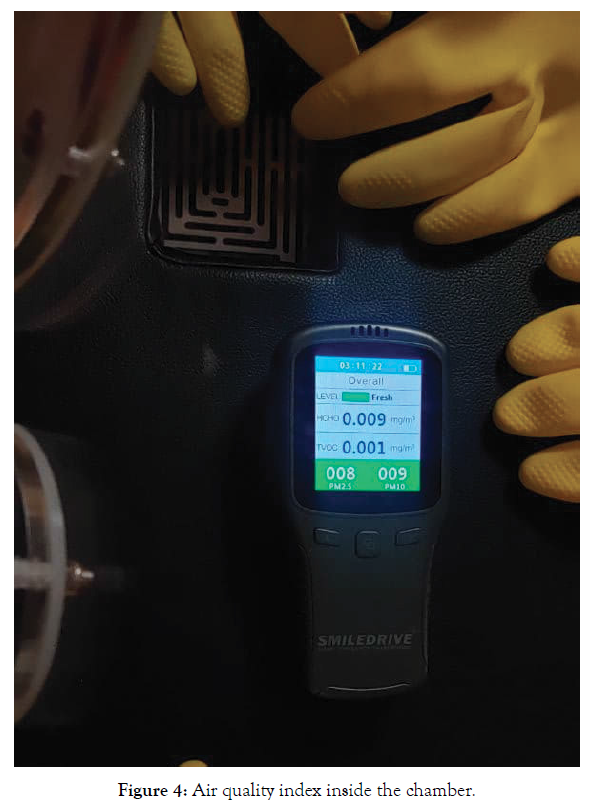
Figure 4: Air quality index inside the chamber.

Figure 5: Air quality index outside the chamber.
Limitations
Due to its ergonomics and robust sturdy built, the weight of this trolley becomes a minor setback as it requires at least a pair of attendants for transport.
A robust, ergonomically designed and cost-effective transport pod is need of the hour in current COVID-19 pandemic. Safety of frontline workers is of utmost importance and this device is a boon for protecting the HCWs and patient relatives.
Currently the protective patient transport chamber is being used in three major COVID Centers of Mumbai City out which two are State Government run and another is run by Municipal Corporation. Disease free status of the HCWs and attendants after use of this transport pod, it can be safely assumed that the infectivity rate is drastically cut down with the use of this Protective patient transport chamber if used as per guidelines and with proper personal protective equipment.
This design is based on our initial experience and will have amendments as per our evolving experiences.
• Medimek Industries
• Mediform
Citation: Bhandarwar AH, Jawale HM, Bakhshi GD, Padekar HD, Tandur AE, Dhimole NN (2021) Pressurised Protective Transport Chamber – A Novel Patient Transport System. J Biomed Eng Med Dev 6:199.
Received: 23-Oct-2021 Accepted: 08-Nov-2021 Published: 15-Nov-2021 , DOI: 10.35248/2475-7586.21.6.199
Copyright: © 2021 Bhandarwar AH, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.