Gynecology & Obstetrics
Open Access
ISSN: 2161-0932
ISSN: 2161-0932
Research Article - (2018) Volume 8, Issue 2
Introduction: Operative delivery is defined as any procedures carry out to facilitate the delivery of the infant. Globally in, 2010, an estimated 18.5 million Cesarean Section (CS) are carry out each year. In Ethiopia, large proportion of the population be lacking in access to essential obstetric care including CS.
Objective: The aim of this study was to determine the prevalence and its associated factors among women undergone operative delivery at Hawassa University Comprehensive Specialized Hospital, Southern Ethiopia, 2017.
Methods and materials: This study conducted in Hawassa University Comprehensive Specialized Hospital, Southern Ethiopia from June to August, 2017. Retrospective record review study was conducted over the past three year’s period from June 2014-June 2016 G.C. Mothers who gave birth over the past three years were the study population. A systematic random sampling technique was used to recruit the study participants. The sample size was determined using a single population proportion formula and a total of 414 study participants were used. Logistic regression was carried out to identify factors associated with women undergone operative delivery. Adjusted odds ratios with their 95% confidence intervals and p<0.05 were considered to have significant association.
Results: In the current study overall prevalence of operative delivery was 38.4% [95% CI: 0.34, 0.43]. Among these; 35.4% were cesarean section, vacuum 2.10%, and Forceps 0.9% deliveries respectively. The probability of operative delivery was 67% [AOR=1.67; 95%CI: 1.05, 2.66] and & 5.31 times [AOR=5.31; 95%CI: 1.79, 5.69] more likely to practice operative delivery in the age group of 25-34 year and >=35 years than 15-24 years.
Conclusions and recommendations: Significant proportion of women practiced operative delivery. Age of women, gestational age and antepartum hemorrhage were main factors with women undergone operative delivery. Emphasis needs to be given women in the group of 25-34 and >=35 years.
Keywords: Operative Deliveries; Associated Factors; Southern Ethiopia; Cesarean Section
Operative delivery is defined as any procedures carry out to facilitate the delivery of the infant. These procedures may include vacuum-assist delivery, use of forceps, and cesarean delivery. Generally vacuum-assist devices consist of a cup applied to the fetal head, a handle for given that traction, a mechanical or electric device for producing vacuum pressure, and a meter for measuring pressure. Cesarean Section (CS) is the operative delivery of the infant throughout an abdominal and uterine incision [1].
Globally in, 2010, an estimated 18.5 million Cesarean Section (CS) are carry out each year [2]. In most low-and middle income countries (LMIC), emergency obstetric care, including Cesarean Section (CS), consist of a large proportion of surgical activity [3,4]. The World Health Organization (WHO) also estimated in 2008 that 3.2 million additional CS were needed in the low-and middle income countries while 6.2 million unnecessary Caesarean deliveries were carry out in a different place [5].
Studies from different countries showed that the incidence of instrumental vaginal delivery has huge geographic differences. In the urbanized countries it ranges10-15% in the UK and 4.5% in the United States, while in low income countries like Niger, Burkina Faso, Mali and Mauritania, lower rates of 1-3% were reported [6,7]. Studies from other areas, revealed that magnitude of forceps and vacuum deliveries were different in different countries: in Zaria and Ibadan forceps delivery rates of 3.6% and 1.57% were reported while vacuum delivery rates of 1.5%, 1.6%, 1.7% and 0.9% were reported from Enugu, Ile-Ife, Ilorin and Kano, respectively [8-10].
In Ethiopia, large proportion of the population be lacking in access to essential obstetric care including CS [11]. Access to caesarean sections can reduce maternal and neonatal mortality and complications such as obstetric fistula. On the other hand, use of caesarean section with no medical need can put women at risk of short-term and long-term health troubles [12]. The 2016 EDHS report found that 2% of live births in the 5 years before the survey were delivered by caesarean section. One percent of the caesarean section were determined after the onset of labor pains, compared to the less than 1% that were determined before onset of labor pains [12].
Caesarean section rates are advanced among first births (4.3%) than for those of elevated orders. Among women who had their most recent live birth in a health facility, 79% of those who gave birth by caesarean section spend three or more days at the facility after delivery compared with 5% of those who had a vaginal birth [12].
Instrumental vaginal delivery is an input element of essential obstetric care, scaling up its use in resource deprived countries through training and supply of appropriate equipment is likely to contribute to reduce maternal and newborn morbidity and mortality [13]. According to the WHO and other UN (United Nations) agencies, assisted vaginal delivery is one of the six critical functions of basic emergency obstetric and new born care (EmONC) [14].
The continuing confront for those responsible for the delivery of the obstetric patient is to carry on examining the indication and appropriate procedure for operative intervention [15]. There were studies that were conducted on women under gone operative deliveries at district levels in Ethiopia. The study conducted in Oromia Regional State revealed that the 29.4% of operative delivery rate and C/S rate was 21%, vacuum 5.6%, forceps 1.3%, destructive deliveries 0.65% [16]. Efforts toward achieving healthy mothers are very critical to stakeholders on Maternal Neonatal and Child Health (MNCH). Therefore, the aim of this study was to determine the prevalence and its associated factors among women undergone operative delivery at Hawassa University Comprehensive Specialized Hospital, Southern Ethiopia, 2017.
Study area and period
This study was conducted in Hawassa University Comprehensive Specialized Hospital (HUCSH) found in Hawassa city, Southern Nations and Nationalities Peoples Region (SNNPR). It is capital city of SNNPR and located at 275 km far from Addis Ababa. Hawassa city in which 359, 358 people are living according to city’s Health Department Estimation in 2017. It has been structured by 7 urban sub-cities collectively have 21 kebeles and 1 Rural sub-city includes 11 kebeles. The city has 83 both public and private health institutions. In detail these were one Public Referral and Teaching hospital, one Public General Hospital, 4 Private Primary Hospitals, 9 Public Health Centers, 17 Public Health Posts and 51 Private Clinics.
HUCSH is the largest hospital in Southern Ethiopia with more than 300 beds which renders service to both the people in region and other people coming from the neighboring region. The hospital was established in 2004/05, provides specialized services and comprehensive health services (prevention, treatment and research). The outpatient department consists of 17 rooms and inpatient service consists of 5 main departments. The average number of patients flow at the OPD is more than 200 people per day. This study was conducted from June to August, 2017.
Study design
Retrospective record review of study was conducted to determine the prevalence and its associated factors among women undergone operative delivery at Hawassa University Comprehensive Specialized Hospital, Southern Ethiopia over the past three year’s period from June 2014-June 2016 G.C.
Population: Source Population: All mothers who gave birth in Hawassa University Comprehensive Specialized Hospital
Study population: Mothers who gave birth over the past three year’s period from June 2014 - June 2016 G.C records review at Hawassa University Comprehensive Specialized Hospital.
Inclusion criteria: Mothers who gave birth over the past three year’s period from June 2014-June 2016 G.C at Hawassa University Comprehensive Specialized Hospital.
Exclusion criteria: Records that didn’t contain full information were excluded from the study. So, 8 records were excludes from the study.
Sampling and sample size determination
Sampling technique: A systematic random sampling technique was used to recruit the study participants using record review of over the past three year’s period from June 2014-June 2016 G.C from Hawassa University Comprehensive Specialized Hospital, Southern Ethiopia. Since total number of counted cards from past three years records was 12017 cards, K value was determined by using formula K=N/n=12017/422=28.47 and K value was approximated to 28. Finally random start was selected by using lottery method and the selected random start was number “8”. By using this random start data was collected from record at every 28th cards.
Sample size determination
The sample size was determined by using a single population proportion formula. It was computed by assuming the prevalence of operative delivery was 50% (which was important to obtain the maximum sample size since we could not find related study conducted in this area) with 95% confidence interval. Accordingly, the sample size calculated for the study is 422 and 10% non-response.
It was calculated from the formula, 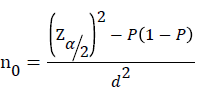
n0= initial sample size derived from estimation formula
 The confidence interval, i.e 1.96 to be 95% confident
The confidence interval, i.e 1.96 to be 95% confident
P =Prevalence of operative delivery taken 50 %( 0.5)
d=Is the marigin of error to be tolerated and a value of 5% was taken.
n-Sample size
10% non-response was considered
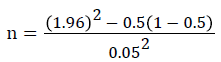
n=384
n=384+10% non-response=422
Out of 422 records; 8 records showed the mothers admitted for nonobstetric cases and didn’t get full information about in line with my objectives. So, 8 records were excludes from the study. Finally the calculated sample size was 414.
Study variables
Dependent variable: Operative delivery was mother who practices at least one of the three of the deliveries (Cesarean delivery, Forceps delivery, Vacuum delivery). Success =1=Yes. If mother who practiced at least one of the three of the operative deliveries was categorized in to success. Failure =0=No. If the mothers who did not practice at least one of the three of deliveries but who practiced spontaneous vaginal delivery was categorized in to failure.
Independent variables:
1. Age
2. Gravidity
3. PROM
4. Hypertensive Disorders of Pregnancy
5. Place of residency (urban and rural)
6. Abruptio placentae
7. Fetal Distress
8. Augmentation and Induction
9. Anemia
10. Mal-presentation
11. Placenta previa
Data collection
Mothers who gave birth over the past three year’s period from June 2014-June 2016 G.C at Hawassa University Comprehensive Specialized Hospital were reviewed for this study. Cards of mothers who had birth in (HUCSH) over three years period was obtained retrospectively. The data was collected by using checklist. Individual information collected from record reviewed from patient history, physical examination, progress note of records from cards.
Data quality control measures: The principal investigator provided training to data collectors. Training includes explanation of the study objectives; techniques for how to file check list, and how to keep confidentiality of data. Pre-testing was done on 30 patients in the different hospital a few days before the data collection. After the pretesting some modification and development of the check list was done. Supervision was done throughout the data collection process and daily checking of the collected data was done in order to keep consistency and problems encountered were managed accordingly. During data entry attention was given to check errors and data cleaning was considered.
Data processing and analysis
The data was cleaned, coded and analyzed by using SPSS version 20. The results of the analysis were presented in the form of tables and figure. For categorical variables, frequency, percentage and descriptive summaries were used to describe the study variable using univarite analysis. Logistic regression was carried out to identify factors associated with women undergone operative delivery. Independent variables found to be significant in the simple binary logistic regression analysis at a cut-off point of p-value <0.25 with 95% confidence interval were included in the multiple binary logistic regression models [17].
In the multiple binary logistic regression model the effect of each independent variable on the women undergone operative delivery were assessed by controlling for the possible confounders using a stepwise backward logistic analysis.
Adjusted odds ratios with their 95% confidence intervals and pvalue of less than 0.05 were considered to have significant association between the women undergone operative delivery and the explanatory variables.
Presence of possible confounders and interaction effects were investigated by computing relative changes on ß coefficients at a cutoff point 15% [18]. If percentage of beta change in a given variable was greater than 15%, then the variable which brought this change have a confounding or interaction effect. To check the interaction effect of the variable, new variable was created by multiplying the two variables (a product term). If the new variable become statistically significant at p-value<0.05, then this variable was considered to have an interaction and the product term was kept in the final model. But if the product term was not significant in the model, it was removed from the model and the variable, which brought the beta change was considered as a confounder .
Occurrence of multicolinearity was checked for the final model with cut-off point mean of variation inflation factor (VIF) less than five [19]. Less than 5 mean VIF value indicates absence of extreme colinearity problem among explanatory variables in the logistic regression model. The model fitness was checked using Hosmer and Lemeshow [20].
Ethical consideration: For this study ethical clearance was sought from the ethical review Board of Hawassa University, College of Medicine and Health Sciences. A permission and support letter was obtained from the Hawassa University, College of Medicine and Health Sciences, Dean Office and Clinical Service Director of (HUCSH). The purpose of the study was clearly explained to study participants. Each study participant was informed about the purpose, methods, and benefits of the study. Study participants was explained and reassured that anything said for research purposes only and no one even their treating doctor have access to their response.
Operational definitions
1. Operative delivery: An obstetric procedure in which active measures are taken to accomplish delivery; includes: Cesarean delivery, forceps delivery and Vacuum delivery
2. Cesarean delivery: The delivery of a fetus, placenta & membrane through an abdominal & uterine incision.
3. Forceps delivery: Means of extracting the fetus with the aid of paired metallic instruments called obstetric forceps.
4. Vacuum delivery: Use of a suction device applied to the fetal scalp to help facilitate delivery of fetal head.
5. Spontaneous vaginal delivery: A natural process of delivery with no operative intervention.
6. Preeclampsia: Is hypertension & edema which occurs after 20 completed weeks of gestation.
7. Eclampsia: Abnormal body movement or loss of consciousness during pregnancy, labor or within 7 days post-delivery, unrelated to other causes
8. Obstructed labor: Failure of progress of fetus in the birth canal for mechanical reasons arising from the maternal pelvis or the fetus itself despite of adequate uterine contraction
9. Placental abruption: Premature separation of the normally implanted placenta before the delivery of the fetus
10. Placenta previa: Implantation of placenta in the lower part of uterus
11. Anemia: Hb level of 11 g/dl or less
12. Chorioamnionitis: Infection of the amniotic membrane
13. Premature rupture of membrane: Rupture of amniotic membrane before onset of labor
14. Fetal distress: A condition in which the fetus is unable to get adequate oxygen & nutrients due to impaired placental blood flow
15. Mal-presentation: When the fetal part other than the head comes out first
16. Breech presentation: When the foot or buttock of the fetus presents
17. Face presentation: When the face of the fetus presents
18. Shoulder presentation: When the shoulder of the fetus presents
19. Brow presentation: When forehead o fetus presents
Socio demographic characteristics of study participants
A total of 414 women were participated in this study and the response rate was 98%. The minimum and the maximum age of the study participants were 15 and 40 years, respectively. The mean age of the study subjects was 26.32 years (+4.24, standard deviation (SD)). Out of 414 study participants; two hundred sixty seven 267 (64.7 %) of study participants were found in the age group of 25 to 34 years. More than half 274 (66.2%) of study participants were from urban residents (Table 1).
| Status of child | ||
|---|---|---|
| Alive | 388 | 93.7 |
| Still birth | 21 | 5.1 |
| Early neonatal death | 5 | 1.2 |
| Apgar score(minute) | ||
| <3 | 29 | 7 |
| >=3 | 385 | 93 |
| Antepartum hemorrhage | ||
| Yes | 23 | 5.6 |
| No | 391 | 94.4 |
| Premature rupture of membrane | ||
| Yes | 19 | 4.6 |
| No | 395 | 95.4 |
Table 1: Socio- demographic and reproductive characteristics of study population at Hawassa University Comprehensive Specialized Hospital, Southern Ethiopia, 2017.
Prevalence of women undergone operative delivery
The overall prevalence of women undergone operative delivery was 38.4% [95% CI: 0.34, 0.43] (Table 1).
Reproductive characteristics of study participants
Two hundred forty 240 (58%) of study participants were in the gravidity of 1 & 2. More than three forth 326 (78.7%) of study participants were parity of in the group of 0 to 1 children. Three hundred forty three 343 (82.9%) of study participants were attended antenatal care visit. Out of 414; study participants, almost all 375 (90.6%) of study participants were no have medical complication. Three hundred thirty three 333 (80.4%) of study participants children birth weight were in the group of 2500 to 4000 g. Nearly all 388 (93.7%) of study participants child status were indicates live birth. Out of 414, study participants; most 391 (94.4%) of study participants were not faced antepartum hemorrhage (Table 1).
In the current study most of women under gone types of operative delivery was cesarean delivery (35.45%) and the least was forceps delivery (0.9%) (Figure 1).
Factors associated with women undergone operative delivery
In the multivariate analysis age of women, gestational age and antepartum hemorrhage were significantly associated with women undergone operative delivery.
The probability of women undergone operative delivery was 67% [AOR=1.67; 95% CI: 1.05, 2.66] and & 5.31 times [AOR=5.31; 95% CI: 1.79, 5.69] more likely to practice operative delivery of women in the age group of 25-34 year and >=35 years respectively as compared with those women in the age group of 15-24 year.
Gestational age and antepartum hemorrhage were the identified predictors with women undergone operative delivery. Women whose gestational age were greater than or equal to 42 weeks were 4.14 times [AOR=4.14; 95% CI: 1.56, 6.96] higher odds of women practiced operative delivery as compared with those women whose gestational age was less than 37 weeks. Those women who faced antepartum hemorrhage were 7.62 times [AOR=7.62; 95% CI: 2.69, 3.85] more likely to practiced operative delivery as compared with those women who did not face antepartum hemorrhage (Table 2).
| Variables | Types of operative delivery (%) | COR of 95%CI | AOR of 95% CI | |
|---|---|---|---|---|
| SVD | Operative delivery | |||
| Age (in year) | ||||
| 15-24 | 69.5 | 30.5 | 1 | 1 |
| 25-34 | 59.7 | 40.3 | 0.22 [0.08,0.63] | 1.67 [1.05, 2.66] |
| >=35 | 33.3 | 66.7 | 0.34 [0.12,0.93] | 5.31 [1.79, 5.69] |
| Place of residence | ||||
| Rural | 55.7 | 44.3 | 1 | 1 |
| Urban | 64.6 | 35.4 | 0.67 [0.45,1.04] | |
| Gravidity | ||||
| Gravida 1&2 | 63.3 | 36.7 | 1 | 1 |
| Gravida 3&4 | 62.8 | 37.2 | 1.02 [0.65,1.61] | |
| >=5 Gravida | 50.9 | 49.1 | 1.66 [0.91,3.02] | |
| Parity | ||||
| 0-1 | 63.5 | 36.5 | 1 | 1 |
| 2-4 | 55.4 | 44.6 | 0.65 [0.31,1.35] | |
| >4 | 53.1 | 46.9 | 0.91 [0.38,2.18] | |
| ANC follow up | ||||
| Yes | 61.5 | 38.5 | 0.98 [0.58,1.66] | |
| No | 62 | 38 | 1 | 1 |
| Gestational age (weeks) | ||||
| 64.835.211 | ||||
| 37-41 weeks | 62.6 | 37.4 | 0.36 [0.14,0.92] | 1.38 [0.77,2.47] |
| >=42 weeks | 40 | 60 | 0.39 [0.17,0.91] | 4.14 [1.56,6.96] |
| Medical complication | ||||
| Yes | 51.3 | 48.7 | 0.62 [0.32, 1.22] | |
| No | 62.7 | 37.3 | 1 | 1 |
| Weight of child (gram) | ||||
| <2500 | 56.9 | 43.1 | 1 | 1 |
| 2500-4000 | 63.1 | 36.9 | 0.86 [0.35, 2.14] | |
| >=4000 | 53.3 | 46.7 | 0.66 [0.31, 1.41] | |
| Status of child | ||||
| Alive | 61.9 | 38.1 | 1 | 1 |
| Still birth | 52.4 | 47.6 | 1.47 [0.61, 3.55] | |
| Early neonatal death | 80 | 20 | 0.41 [0.04, 3.66] | |
| Apgar score (minute) | ||||
| <3 | 51.7 | 48.3 | 1 | 1 |
| >=3 | 62.3 | 37.7 | 1.554 [0.72,3.29] | |
| Antepartum hemorrhage | ||||
| Yes | 63.9 | 36.1 | 0.15 [0.05,0.43] | 7.62 [2.69,3.85] |
| No | 21.7 | 78.3 | 11 | 1 |
| Premature rupture of membrane | ||||
| Yes | 63.2 | 36.8 | 1.07 [0.41,2.78] | |
| No | 61.5 | 38.5 | 1 | 1 |
Table 2: Multivariate analysis of factors associated with women undergone operative delivery at Hawassa University Comprehensive Specialized Hospital, Southern Ethiopia, 2017.
The current study found that Variance inflation factors (VIF) value was 1.06. This confirmed that there was no significant colinearity among predictors.
The statistically non-significant value of the Hosmer-Lemeshow statistics (prob>chi2=0.834) has been evidenced for the model fitting the data reasonably well (Table 3)
| Diagnostic tests | Value |
|---|---|
| Hosmer-Lemeshow goodness | 0.834 |
| Variance inflation factors (VIF) | 1.06 |
Table 3: Model diagnostics results in the multivariate analysis of factors associated with women undergone operative delivery at Hawassa University Comprehensive Specialized Hospital, Southern Ethiopia, 2017.
In this study overall prevalence of operative delivery was 38.4% [95% CI: 0.34, 0.43]. Among these; 35.4% were cesarean section, vacuum 2.10%, and Forceps 0.9% deliveries respectively. This finding is higher than studies conducted in Mattu Karl Hospital, Oromia Regional State, south west Ethiopia and Addis Ababa which was (29.2%) and 20% respectively [16,21]. Possible reason for these discrepancies may be accredited to difference in accessibility and availability of obstetric care in Addis, Mattu, Hawassa and its surroundings. With regard to Cesarean section the present study findings (35.4%) is higher than the acceptable standard range which WHO 20%, lower than national rate in private clinics (46%) and a higher than national institutional C/S rate (18%). The discrepancies might be due to individual preferences as indication in private clinics and sample size difference between the current study and the national figure.
In the present study C/S rate in Hawassa Compressive Specialized Hospital was 35.4% were cesarean section, vacuum 2.10%, and Forceps 0.9% deliveries. At Tikur Anbessa Hospital C/S (10%), vacuum (6.4%), forceps (3.1%), destructive delivery (0.4%) [21]. This difference might be due to availability of services and credited to preference to other operative deliveries and variation in indication.
In the multivariate analysis age of women, gestational age and antepartum hemorrhage were significantly associated with women undergone operative delivery.
Women in the age group of 25-25 years and >=35 years had association with operative delivery. This finding is consistent with study conducted in Yirgalem General Hospital, SNNPR, Ethiopia. Reason for this due to age of women increases the maternal complication also increases.
Those women who faced antepartum hemorrhage had association with operative delivery. This study is in line study conducted in Mattu Karl Hospital, Oromia Regional State, South west Ethiopia [16]. Possible explanation might be due to some of mothers were referred from peripheries after they develop obstructed labour which predisposes for infection and uterine atony which is a risk for APH.
Since the study was hospital based record review, to draw inferences to the wider community can be difficult. Incomplete records.
Considerable proportion of women practiced operative delivery. Age of women, gestational age and antepartum hemorrhage were significant factors associated with women undergone operative delivery. Emphasis needs to be given women in the group of 25-34 and >=35 years, gestational age in the group of >=42 weeks and those pregnant women who faced antepartum hemorrhage.
Availability of data and materials: The data that support the findings of this study was available from the corresponding author upon reasonable request in the form of SPSS Version 20.
Competing interest: We declare that we have no competing interests.
Funding: we declare that Hawassa University, College of Medicine and Health Sciences, School of Public and Environmental Health was provided fund for design of the study, data collection, analysis, interpretation of finding and writing the manuscript.
Authors’ contributions: BJB, took part in planning the study, management of quality of data, analyzes the data and participated in designing the study and writing the manuscript. We are read and approved this manuscript.