Journal of Clinical & Experimental Dermatology Research
Open Access
ISSN: 2155-9554
ISSN: 2155-9554
Research Article - (2019)Volume 10, Issue 6
Background: This community-based epidemiological study aimed to estimate the prevalence and risk factors of sensitive skin syndrome (SSS) using the validated Sensitive Scale-10 (SS-10) questionnaire in Hong Kong.
Methods: In January 2018, 500 subjects were recruited (quota sampling method) across five Hong Kong districts from high to lower level of pollutions (Mong Kok, Tsim Sha Tsui, Causeway Bay, Tsuen Wan, and Shatin; n=100 each). Face-to-face interviews were conducted by volunteers without prior knowledge on sensitive skin definition. Each participant filled out a questionnaire containing information on demography, concomitant skin diseases, and SS-10. Prevalence estimation was based on the cutoff value developed on clinical data in Hong Kong. Risk factors of sensitive skin were analysed using multiple linear regression modelling with total score of SS-10 as the outcome variable.
Results: Our study reported a prevalence of 11.4% of sensitive skin in the local community sample, with skin conditions and districts as significant predictors. The model accounted for 67.6% variance of the total SS-10 score and significantly differed from the null model: F (10, 489)=101.95, p<0.001 with an effect size of 2.09. Significant predictors of sensitive skin included eczema (β=17.02, p<.001), urticaria (β=15.48, p<0.001), psoriasis (β=19.86, p<0.001), food allergy-induced skin sensitivity (β=7.00, p<0.001), and cosmetics-induced skin sensitivity (β=14.84, p<0.001). Tsim Sha Tsui (TST) predicted skin sensitivity significantly (β=6.46, p<0.001) with reference to Shatin.
Conclusion: Our study reported a lower prevalence of SSS in Hong Kong. Suggested predictors were skin conditions, crowded and polluted districts, food allergies, and cosmetics.
Sensitive skin syndrome; Epidemiology; Hong Kong; Cutoff value; Receiver operating characteristic curve; 10-item sensitive scale validated questionnaire
Sensitive skin syndrome (SSS) is group of conditions that manifest as occurrence of unpleasant sensations, namely, stinging, burning, pain, pruritus, and tingling sensations, in response to stimuli that normally should not provoke such sensations. These unpleasant sensations cannot be explained by lesions attributable to any skin disease [1]. SSS is a complicated global clinical and public health problem with increasing prevalence [2-9]. The skin in SSS usually appears normal or is accompanied by transient erythema. SSS can affect all body locations including scalp [10], but the face is particularly prone to SSS [11]. Epidemiological data worldwide over the years have confirmed its existence [12-18]. It also negatively affects patient’s Dermatology Life Quality Index (DLQI) and quality of life with neuropsychiatric complications [19]. SSS is a significant health burden with severe consequences in clinical practice [20].
Previous studies on the prevalence of SSS using self-diagnosis and self-report in populations in Belgium, France, Germany, Greece, Italy, Portugal, Spain, Switzerland, United States of America, Brazil, and Russia have yielded an approximate prevalence rate of 40% [12-18]. In Asian countries, a high prevalence of SSS in Japanese populations (52.84% men and 55.98 women) was reported, but a mean prevalence of 8.62% in men and 15.93% in women was reported across Beijing, Shanghai, and Guangzhou in China (N=9154) [18,21].
Since SSS is a subjective skin syndrome with minimal observable signs, clinical diagnosis depends on a detailed clinical history that substantially burdens physicians and provides additional challenges to busy clinical settings. A universal confirmatory diagnostic test has not been agreed upon and recommended until now. At the same time, it is desirable to have a more costeffective, well-designed, and validated self-reported questionnaire to gather information on the syndrome and distinguish individuals with and without sensitive skin. However, most published studies present data and attributes obtained in clinics, phone surveys, or mail-out questionnaires, with some focusing exclusively on a female population [11,22,23]. For screening methods, most of the community surveys on SSS were based on a self-reported four-point scale (very sensitive, moderately sensitive, not very sensitive, and not sensitive at all), which may be subjected to individual variations in perceptions and interpretations on the severity of skin sensitivity [14,15,18,21-25]. However, some studies use a two-point scale (sensitive and not sensitive), without clarifying the definition of the criteria of SSS [12,14].
In addition, until now the epidemiologic data on SSS in Hong Kong has been in paucity due to the absence of a widely validated screening tool. Thus, this study aimed to measure the prevalence of SSS through a community epidemiological study and examine the associated risk factors of SSS in Hong Kong in terms of age, sex, occupation, marital status, and skin conditions by employing the well-validated 10-item Sensitive Scale (SS-10) questionnaire [26].
The survey complied to the ethical principles of the Helsinki declaration (1983). Voluntary consents were obtained from the interviewees and the interviews posed no physical and mental risks to the participants. Since it was a questionnaire survey, consent was given by the local Academy of Medicine ethical committee.
Measure
This study used the SS-10 questionnaire (Appendix 1a) developed by Misery et al. [26] in assessing the severity of SSS. This 10-item version was developed from the original SS-14, excluding four rare symptoms, namely, scaling, swelling, oozing, and scabs, with the advantages of being quicker and easier to administer. SS-10 has been tested in 11 countries globally and has demonstrated good psychometric characteristics in measuring the severity of SSS, including good content validity that captures the core symptoms of sensitive skin, as well as good internal consistency (Cronbach’s alpha=0.94). Cronbach’s alpha is an estimate of the reliability of psychometric test. SS-10 was also reported to have a significant and high correlation with Dermatology Life Quality Index (DLQI) (r=0.57, p<0.005). A translated validated Chinese language version was used in this study (Appendix 1b) with the cutoff value of 25.5 or above indicating a possibility of sensitive skin established in Chan’s study in clinical population in Hong Kong with good sensitivity and specificity [27,28]. The positive cases of SS are dermatologist diagnosed in a clinic setting [27]. The area under the curve (AUC) of our derived Receiver Operating Characteristic (ROC) curve was 0.866 (95% confidence interval 0.843-0.889) [28]. An AUC of 0.866, sensitivity of 91.7%, and specificity of 75.5% indicated that the SS-10 has a good diagnostic ability in our community setting study of SSS in Hong Kong [28].
In January 2018, a total of 500 subjects were recruited using the quota sampling method with geographical area as the quotacontrol from highly industrialised areas to areas with more greenery. Two of them were in Kowloon peninsula (Mong Kok, Tsim Sha Tsui), one in Hong Kong island (Causeway Bay), and two in the special administrative zones of Hong Kong (Tsuen Wan and Shatin), which are less densely populated than the former three (Figure 1). Quota sampling is a cost-effective method that guarantees the inclusion of populations of interest by recruiting the sample from various locations to increase the representativeness of the studied sample to be generalised to the whole population [29]. One hundred participants were recruited in each of the five different areas. Participants were interviewed face-to-face on the streets in these geographical locations in Hong Kong. The interviewers had no prior knowledge of the condition. Participation was voluntary. Consent was given to the interviewers when participants completed the questionnaire and the anonymity of participants was maintained. The questionnaire asks for the demographic information (sex, age, ethnicity, marital status, sex and age of children, and concomitant skin diseases) and the contents of the SS-10.
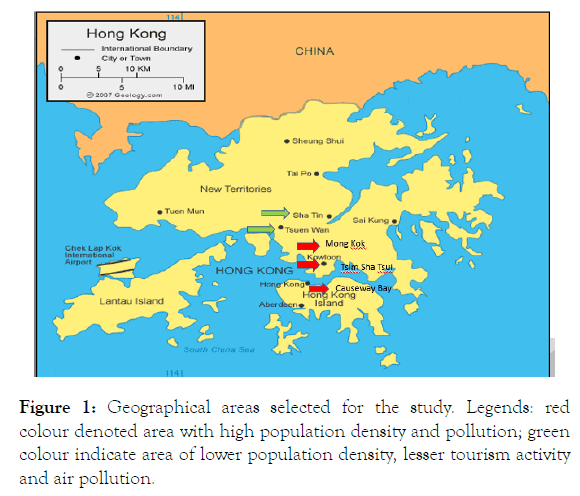
Figure 1. Geographical areas selected for the study. Legends: red colour denoted area with high population density and pollution; green colour indicate area of lower population density, lesser tourism activity and air pollution.
Data were analysed using the Statistical Package for the Social Sciences (SPSS) version 20 (IBM Corp., Armonk, NY, USA).
Analysis was two-tailed with the risk of type 1 error set at 0.05. Based on the clinical sample in Hong Kong, a cut-off value of 25.5 yielded a sensitivity of 91.7% and a specificity of 75.5%. Total score>25.5 on the SS-10 indicated the probable presence of SSS.28 Risk factors were analysed using multiple linear regression. The regression model determines the variance in the severity of skin sensitivity accounted for by the risk factors, including area, sex, occupation, age groups, social class, marital status, number of children, sexes of the first and second children, skin type, and skin condition. Categorical variables were recoded into the dummy variables of 0 and 1. Assumptions were checked, including the independence of error terms and sequential correlation of adjacent errors, normality of distribution of residuals, absence of multicollinearity, and homoscedasticity indicated by the plot of standardized residuals versus predicted values.
In terms of demographic characteristics of the participants, the majority of the participants were white collar workers (26.4%), following which was blue-collar workers (23.0%), and students (19.8%). Most of the participants were married (61.2%) with child (62.0%). A higher percentage of female (60%) than male (40%) was recruited across all districts in the study. Demographic characteristics of the sample by gender were shown in Table 1. Among the 500 individuals surveyed, the mean SS-10 score was 10.3 (SD=10.8). The demographic characteristics of the sample are reported. In terms of prevalence, 443 (88.6%) had SS-10 score below 25.5, whereas 57 (11.4%) had SS-10 score above 25.5. Of these 57 individuals, 32 (56.1%) were female and 25 (43.9%) were male, with nonsignificant difference between the prevalence of SSS across sexes.
| Demographic characteristics | Male n (%) | Female n (%) | |
|---|---|---|---|
| Age | 13-18 | 50 (25.0) | 50 (16.7) |
| 19-29 | 19 (9.5) | 19 (6.3) | |
| 30-39 | 59 (29.5) | 62 (20.7) | |
| 40-49 | 18 (9.0) | 82 (27.3) | |
| 50-59 | 4 (2.0) | 37 (12.3) | |
| Above 60 | 50 (25.0) | 50 (16.7) | |
| Occupation | Student | 49 (24.5) | 50 (16.7) |
| White collar | 53 (26.5) | 79 (26.3) | |
| Blue collar | 60 (30.0) | 55 (18.3) | |
| Housewives | 0 (0) | 88 (29.3) | |
| Unemployed or retired | 38 (19.0) | 28 (9.3) | |
| N (%) | |||
| Marital status | Single | 190 (38) | |
| Married | 306 (61.2) | ||
| divorced | 4 (0.8) | ||
| First child sex | Male | 160 (32) | |
| Female | 118 (23.6) | ||
| Male | 45 (9) | ||
| Female | 76 (15.2) | ||
Table 1: Demographic characteristics of the subjects.
In terms of reported skin condition of the participants, the most common sensitive symptoms were itchiness (79.8%), tightness (68.6%), erythema (60.8%) discomfort (44.2%), pain (26.8%), and heat (23.8%) (Figure 2). In this study, eczema was the most common reported skin disease (n=106, 21.2%), followed by urticaria (n=16, 3.2%), psoriasis (n=13, 2.7%), and other skin diseases (n=46, 9.2%) such as xerosis and acne vulgaris. In addition, 2.2% of the participants reported food allergy (n=11) and 2% reported skin discomfort due to cosmetics (n=10).
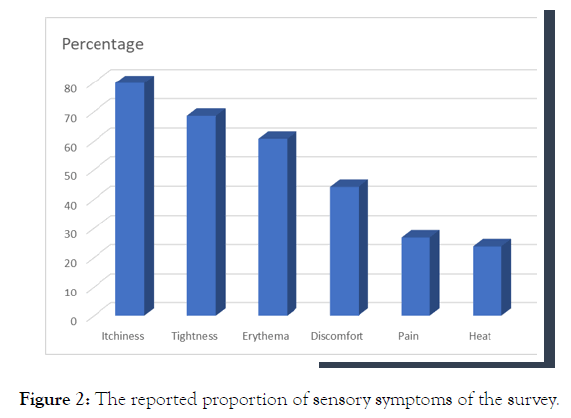
Figure 2. The reported proportion of sensory symptoms of the survey.
The multiple linear regression model identified that geographical areas or districts and skin condition were significant predictors of the severity of skin sensitivity. The model accounts for 67.6% variance of the total SS-10 score and a significant difference from the null model, F(10,489)=101.95, p<0.001 with an effect size of 2.09. Interpreting the β coefficients of the dependent variable, significant predictors of the total score of sensitive skin included eczema (β=17.02, p<0.001), hives (β=15.48, p<0.001), psoriasis (β=19.86, p<0.001), other skin conditions (β=18.14, p<0.001), food allergy-induced skin conditions (β=7.00, p<0.001) and cosmetics-induced skin sensitivity (β=14.84, P<0.001) with no skin disease as the reference category. With regard to the districts, Tsim Sha Tsui significantly predicted skin sensitivity (β=6.46, P<0.001) with reference to Shatin (Table 2).
| Variables | β | S.E.β | Standardized coefficients | t | P |
|---|---|---|---|---|---|
| Eczema | 17.022 | 0.701 | 0.646 | 24.27 | 0 |
| Hives | 15.482 | 1.593 | 0.253 | 9.716 | 0 |
| Psoriasis | 19.862 | 1.76 | 0.293 | 11.284 | 0 |
| Others | 18.137 | 0.985 | 0.487 | 18.42 | 0 |
| Cosmetic-induced conditions | 14.838 | 1.993 | 0.193 | 7.444 | 0 |
| Food allergy-induced conditions | 7.004 | 1.906 | 0.095 | 3.676 | 0 |
| No reported skin problem as the reference category | |||||
| TST | 6.463 | 0.878 | 0.24 | 7.358 | 0 |
| CWB | 1.639 | 0.879 | 0.061 | 1.864 | 0.063 |
| TW | 1.148 | 0.879 | 0.043 | 1.306 | 0.192 |
| MK | -1.54 | 0.877 | -0.057 | -1.755 | 0.08 |
Shatin as the reference category. TST: Tsim Sha Tsui; CWB: Causeway Bay; TW: Tsuen Wan; MK: Mong Kok).
Table 2: Multiple regression of SS-10.
To the best of our knowledge, this local study is the first to examine the prevalence and demographic correlation of SSS in a community sample from Hong Kong using the well-validated SS-10 questionnaire. Our study reported a prevalence of 11.4% of sensitive skin in the local community sample based on the cutoff value of SS-10. This study reported that the prevalence rate of SSS in Hong Kong was comparable to that in community-based studies conducted in the metropolitan cities of Beijing, Shanghai, and Guangzhou in China, which documented 16% in women and 9% in men on average [21] and 23% on a smaller sample consisting predominantly of women, all using self-report questionnaires [22].
The difference between the prevalence difference is unclear and not fully studied. The difference between the prevalence of SSS in China compared to Europe and the States may be due to climatic and difference in latitudes of these cities. The more southern part of the country has a higher sunshine, solar radiation and humidity [30]. The methodology used in the study in China is self-declared; some Chinese may not know ‘sensitive skin’ very well, hence, even they have perceived the sensation of pain over their skin in normal circumstances, they will not contribute this as sensitive skin and failed to self-declare [21]. The large number of people reporting to have sensitive skin might reflect the condition of sensitive skin is commonly addressed in media and is known among relatively prosperous population. Cultural factors and media might have influenced the propensity to report self-perceived sensitive skin [31]. An alternative explanation is suggested by Taïeb: as sensitive skin maybe a continuum; the sensitive skin group might be divided into the “very sensitive skin” and “relatively or rather sensitive skin ’ groups. People reporting slightly sensitive skin were considered the same as people without sensitive skin. 31 Under this distribution or division, very sensitive skin was declared by 8.6% of people worldwide (Range 6.3-15%) (Figure 3). A difference of sensitive skin prevalence between countries and locations is observed. The exact reason is unknown. Genetic predisposition to epidermal barrier protein, neuronal aberrancy, environmental factors, lifestyle behaviors, physiological and psychometric factors may be interactive.
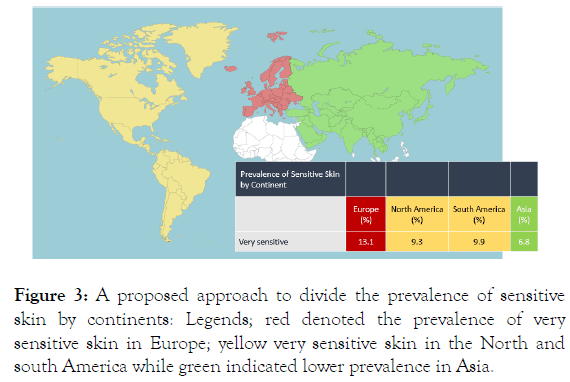
Figure 3. A proposed approach to divide the prevalence of sensitive skin by continents: Legends; red denoted the prevalence of very sensitive skin in Europe; yellow very sensitive skin in the North and south America while green indicated lower prevalence in Asia.
In this study, the significant risk factors or predictors of SSS draw indirect connection, although inconclusive between tourist areas and the severity of sensitive skin, as significant areas that predict sensitive skin in TST are the centres of commercial tourisms and densely populated. The findings supported the documented association between air pollution and skin sensitivity [4,32]. These also elucidate the rising concern of cosmetic exposure and food allergy. Indeed, stress diets with poor nutritional fast foods, first- to third-hand cigarette smoking and air pollutions, application of cosmetic products, and artificial fumes like formaldehyde substances released from architectural renovations could be possible confounders and underlying culprits. The proposed functional role of the epidermal keratinocytes acting as biosensors in nociceptive and pruritogenic small neurogenic fibre signal transmission through Transient Receptor Potential (TRP) V1, TRPV3, TRPV4 and TRPM8 via the dorsal root ganglion ascending to the somatosensory cortex resulting the unpleasant sensation of heat, pruritus, pain and tautness may provide a plausible coherent explanation on how the peripheral and central nervous system reciprocate to these unfavourable environmental, lifestyle, endogenous factors [33-35].
We observe that sensitive skin is more common in individuals with eczema and other skin diseases. The International Forum for the Study of Itch defined the perception of the unpleasant sensations in SSS in the absence of pre-existing skin diseases as a possible cause. SSS may overlap or co-exist with some common chronic skin conditions but still has its own characteristic features. This is important in defining SSS as a discrete condition for study and research. Richter has observed that xerosis in SSS is more frequent, but majority of SSS cases do not involve dryness of skin [36]. The link between sensitive skin and disrupted skin barrier is well reported; it is highly possible that increased trans epidermal water loss and decreased epidermal barrier integrity may facilitate the penetration of irritant or allergen into the skin; eventually induce more stress in the skin which lead to alternation in epidermal nerve innervation and affect the perceived dysfunctional sensation including TRP and nociceptive afferent nerve fibers.
Our study based on a clinical cutoff value with a ROC curve of sensitivity of 91.7% and specificity of 75.5% (AUC=0.866) using the validated SS-10 derived from a clinic attendee sample may have selected those patients with very sensitive skin in the community. Further studies are mandated to study the usefulness of SS-10 as a screening tool of SSS in the community. In addition, the psychometric properties of the SS-10 including test-retest reliability could also be addressed in future studies by testing the skin sensitivity on participants repeatedly over time to provide a fuller picture of the performance of SS-10 and the change in skin sensitivity over a period of time.
The present study has the following limitations. First, this study lacked sufficient factors directly associated with geographic areas to explain the district effect in the regression model. Second, factors such as air validity and lifestyle that directly reflect the characteristics of the geographic area could be included in future studies. In addition, by increasing the number and variations of geographic areas included in future studies, the issue of the district effect on the risk factors of sensitive skin could be fully addressed in a hierarchical model. Third, quota sampling method has been criticised of being biased to people who show interests in the research topic and easily accessible, thus hindering the generalisation of the studied sample to the population [29]. This limitation was counteracted by recruiting participants from multiple locations in Hong Kong with different climate characteristics. Future studies with larger sample size and variability of districts using a more probabilistic method and a more comprehensive checklist of possible risk factors may shed light into the possible attributes of SSS in the Asian population.
SSS is a prevalent condition in ethnic Chinese in Hong Kong. Using the SS-10 questionnaire, which is a self-reported screening tool of sensitive skin, the prevalence in the current study in the male and female samples was comparable with the reported Chinese prevalence. To our best knowledge, the present study is the first to use a self-report instrument on screening individuals with SSS in a community sample in Hong Kong. It may begin a new line of research using a convenient, non-invasive, costeffective, and acceptable way to study subjects in a community setting. Significant risk factors associated with SSS are skin conditions, geographic area, cosmetic stimulants, and food allergy. Follow-up surveys using the same methodology over time may shed more light on this important issue. Moreover, our findings will provide a basis for further research of SSS locally and may improve the awareness of dermatologists in clinical settings of other populations to make cross-cultural comparison of the prevalence of SSS in other cities in China that share similar ethnic background, lifestyle, and cultures yet different climatic conditions, such as temperature, humidity, wind, and sun exposure.
Received: 05-Nov-2019 Accepted: 18-Nov-2019 Published: 25-Nov-2019
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.