Journal of Depression and Anxiety
Open Access
ISSN: 2167-1044
ISSN: 2167-1044
Research - (2021)Volume 10, Issue 2
Introduction: Depression is one of major health problems of patients with type 2 diabetes mellitus. However, it remains undiagnosed and left untreated in more than half of diabetes cases. Despite 80% of people with type 2 diabetes live in low and middle-income countries; many studies on depression and its associated factors among patients with type 2 diabetes mellitus were conducted in the developed world.
Objective: The present study was aimed to assess prevalence of depression and associated factors among type 2 diabetes patients attending hospitals in Ilu AbaBor and Bunno Bedelle Zones, South West Ethiopia, 2020.
Methods: A cross-sectional study design was conducted on 354 type 2 diabetes patients attending hospitals of Ilu AbaBor and Bunno Bedelle Zones from January 1 to March 30, 2020. Convenient sampling technique was used to select study participants after the sample size was allocated to each hospital. Data were entered into EpiData manager version 4.2.2 and exported to statistical package for the social science (SPSS) version 20.0 and analyzed using descriptive statistics, Bivariate and Multivariate logistic regressions. The statistical significance was set at p<0.05
Results: Out of the 354 patients recruited, 321 (90.7%) patients were involved in the study. The mean age of the participants was 41.3 with SD of 12.8 years. The prevalence depression was 118 (34.9%) of which 20.9% of participants were moderately depressed. Age [AOR 2.7; 95%, CI: 1.10, 6.43], family or social support [AOR=1.7, 95% CI: 1.37, 2.57], having diabetic complications [AOR=3.8, 95% CI: 1.61, 9.37] and level FBS [AOR=5, 95% CI: 1.93, 12.68] were the factors significantly associated with depression
Conclusion: Relative to global estimation, the prevalence of depression was high among patients with type 2 diabetes. Therefore, early diagnoses and treatments of depression primarily to improve self-care and medication adherence which in turns reduce risk of disability and early death were recommended.
Type 2 Diabetes mellitus; Depression; Prevalence; Associated Factors
AOR: Adjusted Odd Ratio; BDI: Beck depression inventory; CI: Confidence Interval; DM: Diabetes Mellitus; FBS: Fast Blood Sugar; SPSS: Statistical Package for Social Science; T2DM: Type 2 Diabetes Mellitus
Type two diabetes Mellitus (T2DM) is most prevalent type of diabetes among adults and constitutes around 90-95% of all cases [1,2]. It has been estimated that number of people with T2DM is 200 million in 2010 and the number is expected to rise to 300 million by the year of 2025 [3]. Ethiopia is one of the top Africa countries with the highest number of people affected by diabetes mellitus (DM). According to international diabetes federation (IDF), the prevalence of diabetic mellitus in Ethiopia is steadily increasing with 3.5% in 2011 [3], 4.36% in 2013 [2], and 5.2% in 2015 making one of the top four countries with the highest adult diabetic populations in sub-Saharan Africa [4]. Recent systematic review conducted showed that prevalence of diabetes in Ethiopia is ranging from 0.3% to 7% [5].
Depression is a significant health problem among patients with T2DM, with an estimated prevalence of 15–20% [6,7]. It is the third leading cause of burden of diseases worldwide and is two to three times higher among patients with diabetes than general population [8]. A prospective cohort study revealed that depression among type 2 diabetes patients is associated with an increased risk of long-term complications of diabetes [9]. Many studies also reported that depression is associated with poor adherence to diet, exercise, disease control medication, and cessation of smoking recommendations [10], higher medical costs, and greater mortality among patients with diabetes [11].
Despite its greatest negative impact on health outcome, depression remains undiagnosed in more than half of diabetes cases. This suggest that depression is unrecognized and in the more that 50% patients with type 2 diabetes, which in turns may exacerbate the progression of diabetes [12]. Several studies throughout the globe have reported inconsistent prevalence of depression among type two diabetic patients. For instance, the prevalence of depression among T2DM was 49.0% in India [13], 43.5% in Pakistan [14], 47.4% in Saudi Arabia and 69.0% in Egypt [15]. However, the prevalence of depression among type 2 diabetes was not studied adequately in Ethiopia. But existing studies reported the better 13% [16] and worst 47% [17] prevalence of depression among patients with specific type 2 DM in the Ethiopia
Previous studies revealed that socio-demographic and economic factors, diabetic profile, having diabetic complications, comorbidity with other disease, blood pressure status, body mass index, physical activity, stress, and sleeping hours are factors associated with depression [18-20]. In addition, being female, lack of social support, unhealthy lifestyle, alcohol intake, loss of spouse or close person, non-adherence to dietary and medication regimen were reported as significant predictors [21,22].
Despite 80% of people with type 2 diabetes live in low and middle-income countries, many researches on depression among patients with type 2 diabetes were conducted in the developed world [23]. Moreover, only a few studies have been conducted in Africa particularly in Ethiopia and no studies conducted in the current study area to assess the prevalence and associated factors of depression among patients with specific type 2 diabetes. Therefore, the main aims of present study were assessing the prevalence of depression and associated factors among type 2 diabetes patients attending hospitals in Ilu AbaBor and Bunno Bedelle Zones, South West Ethiopia.
Study area and period
The study was conducted in Ilu AbaBor and Bunno Bedelle Zones, Oromia Regional state, South West Ethiopia. Ilu AbaBor zone is one of the 20 zones of Oromia regional state situated at South Western of the region and located at a distance of about 650 km from center of the country. Two hospitals namely: Mettu Karl hospital and Darimu hospital are found in the zone. Mettu Karl hospital is the only referral hospital in the zone and serves as a referral hospital for the zone and adjacent regional states. It also serves as training hospital for health sciences, medical interns and Master of Emergency Surgery Students from different Universities. Darimu hospital which is the only district hospital in the zone serves the people of Darimu town and surrounding rural kebeles and districts. Bunno Bedelle is another Oromia regional state zone situated at South-Western of the region and located at a distance of about 500km from the Addis Ababa, capital city of Ethiopia. Bedelle hospital and Didhessa hospital are the two-district hospital found in the zone serving population of the zone and adjacent districts. Both hospitals have been serving as training hospitals for health science students from different Universities. The study period was spanned from January 1to March 30, 2020.
Study design
Institution based cross sectional study design was conducted.
Source population
The source population of the study was all type 2 diabetic patients attending hospitals in Ilu AbaBor and Bunno Bedelle zones.
Study populations
The study population was all selected Type 2 diabetic patients attending hospitals in Ilu AbaBor and Bunno Bedelle zones.
Inclusion criteria
At the onset of the study, all registered Type 2 diabetic patients aged ≥18 years in public hospitals of Ilu AbaBor and Bunno Bedelle zones were included to the study.
Exclusion criteria
Seriously ill patients during data collection period were excluded from the study.
Sample size determination and sampling procedure
The sample size was determined using a single population proportion formula by considering the following assumptions:
95% level of confidence interval
5% margin of error (d)
36.9% as a prevalence of depression among type 2 diabetes patients from recent study [24].
( (Z α/2)2*P* (1-P))/d2 = ( (3.84*0.23)/0.0025 = 353.4 ≈354
Therefore, the sample size for this particular study was 354. In selecting study participants, first, the total sample size was allocated proportionally to number of registered T2DM in each hospital. Then, an individual patient was selected conveniently until required sample size was achieved.
Variables
The dependent variable of this study was depression and independent variables were age, sex, marital status, residence, religion, family or social support, educational status, occupation, level of education, duration of diabetes, mode of current treatment, having diabetic complications, smoking status, status of alcohol consumption, level of fast blood sugar (FBS), level of systolic blood pressure (SBP), level of diastolic blood pressure (DBP), body mass index (BMI),.
Data collection tool and method
Data was collected through face to face interviews. The interviews were conducted in a quiet room at where patients came for routine follow up. The collected data consisted of socio-demographic characteristics, clinical characteristics, social history, clinical parameters and questions related with depression. Levels of fast blood glucose, blood pressure and weight and height (BMI)) were obtained from the last patients’ medical record. The Beck Depression Inventory (BDI) scale questionnaire was used in this study. It has been widely used tool to rate depression severity over the last two weeks and has 21 multiple-choice questions [25,26]. Responses to the 21 questionnaires are made on a 4-point scale, ranging from 0 to 3. Total scores range from 0 to 63. The scores of 11-16, 17-20, 21-30, 31-40, and over 40 represent cut points for mild mood disturbance, borderline clinical depression, moderate depression, severe depression, and extreme depression, respectively [3].
Data analysis
Data were entered into Epi Data version 4.2.2 and exported to statistical package for the social science (SPSS) version 20.0. Frequencies means and standard deviations of independent variables and level of depression were analyzed using descriptive statistics. Bivariable and Multivariable logistic regressions were to identify factors associated with depression. Variables with a P-value of less than 0.25 in the Bivariable logistic regression were entered into the Multivariable regression model to control the possible effect of confounders. An adjusted odds ratio (AOR) with 95% confidence interval was used to identify the strength of the associated factors with depression. The statistical significance was considered at P-values< 0.05 in the multivariate logistic regression. The results of study were described in the form of text, tables and figure.
Participants’ socio-demographic characteristics
Out of the 354 diabetic patients recruited, 321 (90.7%) patients were involved in the study. Higher percentage 201 (62.6%) of participants were male. The mean age of the participants was 41.3 with SD of 12.8 years. 124 (38.6%) participants had no social or family supports. Nearly half 154 (48%) of participants did not attended more than primary school (Table 1).
| Variables | Categories | Frequency | Percent |
|---|---|---|---|
| Sex | Male | 201 | 62.6 |
| Female | 120 | 37.4 | |
| Age (m=40.5, S.D.=11.5) | 18-29 | 59 | 18.4 |
| 30-39 | 82 | 25.5 | |
| 40-49 | 103 | 32.1 | |
| 50+ | 77 | 24.0 | |
| Marital status | Single | 80 | 24.9 |
| Married | 220 | 68.5 | |
| Others | 21 | 6.6 | |
| Residence | Urban | 175 | 54.5 |
| Rural | 146 | 45.5 | |
| Religion | Orthodox | 122 | 38.0 |
| Muslim | 158 | 49.2 | |
| Protestant | 41 | 12.8 | |
| Family/Social support | Yes | 197 | 61.4 |
| No | 124 | 38.6 | |
| Occupation/Employment | Governmental | 110 | 34.3 |
| Farmer | 168 | 52.3 | |
| Merchant | 43 | 13.4 | |
| Level of education | Primary school | 154 | 48.0 |
| Secondary school | 101 | 31.5 | |
| diploma | 35 | 10.9 | |
| Degree and above | 31 | 9.7 |
Table 1: Socio-demographic characteristics of patients with type 2 diabetes mellitus attending hospitals in Ilu AbaBor and Bunno Bedelle zones, South-West Ethiopia, 2020 (n=321).
Participants’ clinical characteristics
In the present study the mean duration of stay with type 2 diabetes was 5.5 (SD = 3.9) years and oral medications was the most frequently 204 (63.6%) reported mode of treatment. Almost three fourth 238 (74.1%) of participants had overt diabetes (Table 2).
| Variables | Categories | Frequency | Percent |
|---|---|---|---|
| Duration with diabetes (m=5.5, S.D.=3.9) |
≤2 | 92 | 28.7 |
| 3-4 | 80 | 24.9 | |
| 5-9 | 88 | 27.4 | |
| 10+ | 61 | 19.0 | |
| Mode of current treatment | Oral | 199 | 62.0 |
| Insulin | 53 | 16.5 | |
| Oral and insulin | 32 | 10.0 | |
| Life style modification | 37 | 11.5 | |
| Having diabetes complications | Yes | 77 | 24.0 |
| No | 244 | 76.0 | |
| FBS (mg/dl), 153.0 ± 36.3 | Pre-diabetes ( 100-125) | 83 | 25.9 |
| Overt diabetes (≥126) | 238 | 74.1 | |
| SBP (mmHg) , 126.3 ± 11.6 | Normal (<120) | 49 | 15.3 |
| Pre-hypertension (120-130) | 230 | 71.7 | |
| Hypertension (≥140) | 42 | 13.0 | |
| DBP (mmHg), 81.8 ± 9.3 | Normal (<80) | 90 | 28.0 |
| Pre-hypertension (80-89) | 189 | 59.0 | |
| Hypertension (≥90) | 42 | 13.0 | |
| BMI (kg/m2), 24.0 ± 3.6 | Normal (18.5-24.9) | 205 | 63.9 |
| Overweight (25-29.9) | 95 | 29.6 | |
| Obese (≥30) | 21 | 6.5 |
Table 2: Clinical characteristics of patients with type 2 diabetes mellitus attending hospitals in Ilu AbaBor and Bunno Bedelle zones, South-West Ethiopia, 2020 (n=321).
Participants’ social history
The finding of present study showed that out of 321 participants 66 (20.6%) and 85 (26.5%) of participants had history of cigarette smoking and alcohol consumption respectively.
Prevalence of depression
Prevalence of depression among type 2 diabetic patients was found to be 112 (34.9%). The higher percentage (20.9%) of participants had moderate depression whereas few (2.5%) participants had extreme depression (Figure 1).
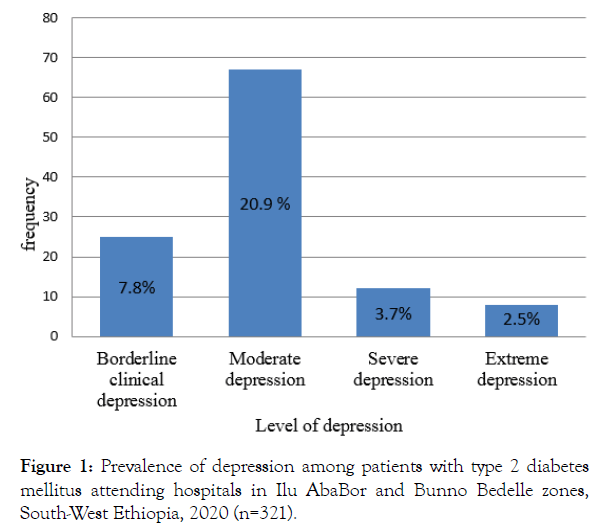
Figure 1: Prevalence of depression among patients with type 2 diabetes mellitus attending hospitals in Ilu AbaBor and Bunno Bedelle zones, South-West Ethiopia, 2020 (n=321).
Factors associated with diabetes related distress
Logistic regression analysis was conducted to identify factors associated with depression. During Bivariate analysis age, family or social support, duration of diabetes, mode of current treatment, having diabetes complications, smoking status, alcohol consumption status, and level of FBS were identified factors associated with depression at p<0.25. Further the multivariate analysis conducted indicated that duration of diabetes, mode of current treatment; smoking status and alcohol consumption status were not significantly associated with depression. However, the odd of depression among 50 and above years old participants were 2.7 times higher when compared with depression among 18-29 years old participants [AOR 2.7; 95%, CI: 1.10, 6.43]. Participants who had no family or social support had 1.7 times higher odds of depression than those who had family or social support [AOR=1.7, 95% CI: 1.37, 2.57]. Participants who had diabetes complications had 3.8 times higher odds of depression than those who had no diabetes complications [AOR=3.8, 95% CI: 1.61, 9.37]. The odds of depression among participants with overt diabetes was 5 times higher when compared to participants with pre-diabetes [AOR=5, m 95% CI: 1.93, 12.68] (Table 3).
| Variables | Depression | OR with 95% CI | p-value | ||
|---|---|---|---|---|---|
| No | Yes | Crude | Adjusted | ||
| Age | - | - | - | - | 0.002 |
| 18-29 | 41 (12.8) | 18 (5.6) | 1 | 1 | - |
| 30-39 | 70 (21.8) | 12 (3.7) | 0.38 (0.17,0.89) * | 0.30 (0.11,0.80) | - |
| 40-49 | 76 (23.7) | 27 (8.4) | 0.8 (0.39,0.89) | 0.86 (0.365,2.03) | - |
| 50+ | 22 (6.9) | 55 (17.1) | 5.7 (2.71, 11.96) *** | 2.7 (1.10,6.43)** | - |
| Family/social support | - | - | - | - | 0.04 |
| Yes | 140 (43.6) | 57 (17.8) | 1 | 1 | - |
| No | 69 (21.5) | 55 (17.1) | 2 (1.224,3.131) *** | 1.7 (1.37,2.57)* | - |
| Duration of diabetes | - | - | - | - | 0.66 |
| ≤2 | 64 (19.9) | 28 (8.7) | 1 | 1 | - |
| 3-4 | 64 (19.9) | 16 (5) | 0.570 (0.28, 1.15) | 0.58 (0.26,1.31) | - |
| 5-9 | 70 (21.8) | 18 (5.6) | 0.58 (0.29,1.16) | 0.36 (0.16,0.82) | - |
| 10+ | 11 (3.4) | 50 (15.6) | 10.39 (4.71,22.88) ** | 4.7 (1.65,13.71) | - |
| Mode of current treatment | - | - | - | - | 0.49 |
| Oral medication | 151 (47) | 48 (15) | 1 | 1 | - |
| Insulin | 18 (5.6) | 35 (10.9) | 6.1 (3.178,11.77) *** | 2.03 (2.36,3.98) | - |
| Oral and insulin | 14 (4.4) | 18 (5.6) | 4 (1.87,8.738) *** | 1.5 (0.48,4.71) | - |
| Lifestyle modification | 26 (8.1) | 11 (3.4) | 1.33 (0.612,2.892) | 2.1 (0.82,5.56) | - |
| Having diabetes complications | - | - | - | - | <0.001 |
| Yes | 21 (6.5) | 56 (17.4) | 8.95 (4.99,16.04) *** | 3.8 (1.61,9.37)*** | - |
| No | 188 (58.6) | 56 (17.4) | 1 | 1 | - |
| Smoking status | - | - | - | - | 0.175 |
| Yes | 30 (14.4) | 36 (11.2) | 2.8 (1.62,4.91) ** | 1.4 (0.53,4.06) | - |
| No | 179 (55.8) | 76 (23.7) | 1 | 1 | - |
| Taking alcohol | 0.917 | ||||
| Yes | 46 (14.3) | 39 (12.1) | 2 (1.139.3.147)** | 1.6 (1.28,2.50) | - |
| No | 163 (50.8) | 73 (22.7) | 1 | 1 | - |
| FBS (mg/dl), 153.0 ± 36.3 | <0.001 | ||||
| Pre-diabetes (100-125) | 74 (23.1) | 9 (2.8) | 1 | 1 | - |
| Overt diabetes (≥126) | 135 (135) | 103 (32.1) | 6.27 (2.99,13.12)*** | 5 (1.93,12.68)*** | - |
Table 3: Bivariate and multivariate analysis of factors associated with depression among patients with type 2 diabetes mellitus attending hospitals in Ilu AbaBor and Bunno Bedelle zones, South-West Ethiopia, 2020 (n=321).
Coexistence of depression with T2DM results in decreased medication adherence which in turns leads poor health outcome, increased disability and increased risk of death [27]. Studying prevalence and factors associated with depression is crucial to alarm early diagnosis and integration of depression treatment into primarily health care. But, prevalence of depression and its associated factors among type 2 diabetic patients was not studied adequately in the Ethiopia. Therefore, the main aim of present study was to assess prevalence of depression and its associated factors among type 2 diabetic patients attending hospitals in Ilu AbaBor and Bunno Bedelle zones.
In the present study the prevalence of depression among study participants was 34.9%. This finding was congruent with previous studies conducted in the Northern Ethiopia, 36.9% [24] and Qassim, 34.8% [28]. However, the prevalence of depression in the current study was more than two time of previous finding (15.4%) of study conducted in Gondar, Ethiopia [29]. Similarly, the current prevalence of depression among type 2 diabetic patients was much higher than the finding of previous studies conducted Sri Lanka, 5.9% [26] and Turunesh Beijing hospital, 21.3% [30]. This discrepancy could be explained by the difference in health care settings, study populations and measurement tool. For instances, both Turunesh Beijing hospital and tertiary care hospital in Sri Lanka are specialized hospitals. Those who are treated in a specialized hospital may have better and comprehensive care because of adequate skilled human power. Unlike to the current study the source population of study conducted in Turunesh Beijing hospital was both type one and type 2 diabetic patients and the measurement tool used to measure depression was also Patient Health Questionnaire-9 (PHQ-9).
On the contrary, this study found relatively lower prevalence of depression among type 2 diabetic patients than studies conducted in Iran, 59% [25], Ethiopia, 43.6% [31], Pakistan, 43.5% [14] and Malaysia, 40.3% [32]. These inconsistent findings might be due to different assessment tools, health service delivery systems, lifestyle, and social interaction. For example, in Pakistan and Malaysia, the hospital anxiety and depression scale (HADS) tool was used to assess prevalence of depression. The other reason for the difference might be due to different study settings and participants. For example, the study in Ethiopia was done among patients with both type one and T2DM.
Regarding factors associated with depression among type 2 diabetic patients, age of participants was significantly associated with depression. This was also true for prior studies conducted in Pakistan [14], Malaysia [32], Bangladesh [33], Iran [25] and Ethiopia [31] in which odd of having depression were significantly higher in older participants. This could be due to physical inactivates among elder patients. It is the fact that physical activity is a protective barrier against depression and the development of other psychological illnesses due to an increased release of endorphins and brain neurotransmitters during exercise. The other possible explanation is older patients faces many challenges including family or social isolation, different co-morbid diseases and disabilities. The odds of developing depression among diabetic patients who had no family or social support were 1.7 times more likely at risk to develop depression when compared with participants who had family or social support. This finding was similar with the finding of prior studies in which patients with poor social support were more likely depressed than their counter parts [24,30,34]. This might be due to the fact that social support reduces depression. Having poor social support may leads to delayed diabetic treatment.
In the present study patients who had diabetic complications were almost four times more likely to have depression than their counterparts. The reason might be due to the fact that diabetic complications might leads to more burdens to patients from multiple medications, unemployment, less chance to get social relationships which may predispose the patient to develop depression. Earlier studies conducted in Pakistan [14,25] and Iran revealed that level of FBS was most strongly associated with depression. In agreement to these findings the current study showed that participants with FBS ≥ 126 were 5 times more likely depressed than those with FBS of between 100 and 125.
There are some potential limitations of this study that should be kept in mind when interpreting the findings. First, the participants were represented only type 2 diabetic patients attending hospitals. This limitation did not allow for generalizability of the findings to the entire diabetic patients in the community. Second, the cross-sectional nature of the study design limits the ability to draw conclusions about definitive cause and effect relationship. Lastly since this study was based on participants’ reports of data there may be recall bias.
The present study found that relative to global estimation prevalence of depression was high among patient with type 2 diabetes. This suggests that for the better health outcomes of diabetic patients, it is needed to reduce prevalence of depression through fully integrating mental health services into primary health care in line with medical care. Age, having family or social support, having diabetic complications and level of FBS were the factors significantly associated with depression. Therefore, health care providers need to give emphasis to diabetic patients with diabetic complications, no social support and uncontrolled glycemia in order to prevent further problems. Lastly, early diagnoses and treatments of depression primarily to improve self-care and medication adherence which in turns reduce risk of disability and early death were recommended.
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethical approval was obtained from Mettu University, College of health sciences, and department of nursing. Supportive letter was given, and permission was obtained from each hospital. Informed consent was obtained from participants after they were informed about the objectives of the study. Confidentiality and privacy of participants was also ensured.
Our deepest gratitude goes to Mettu University, College of Health sciences, department of Nursing for giving us the opportunity to conduct this study. We would also like to extend our sincere gratitude to the data collectors, supervisors and the study participants for being involved in the study.
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data. All authors also approved the final version for submission.
This study was conducted in collaboration with Mettu University. Every step of the study was followed by Mettu University, College of Health sciences, department of Nursing. The university has no role in designing, analysis and writing of the study.
The authors declare that they have no competing interests.
Citation: Geleta BA, Dingata ST, Emanu MD, Kebede EB, Eba LB, Abera KB, et al. (2021) Prevalence of Depression and Associated Factors among Type 2 Diabetes Patients attending hospitals in Ilu AbaBor and Bunno Bedelle Zones, South West Ethiopia, 2020: A Cross Sectional Study. J Depress Anxiety. 10:389.
Received: 19-Nov-2020 Accepted: 17-Feb-2021 Published: 24-Feb-2021 , DOI: 10.35248/2167-1044.21.10.388
Copyright: © 2021 Geleta BA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.