Journal of Women's Health Care
Open Access
ISSN: 2167-0420
ISSN: 2167-0420
Research Article - (2021)
Introduction: Despite the fact that knowledge of potential side effects of many herbal medicines in pregnancy is limited and that some herbal products may be teratogenic, data on the extent of use of herbal medicines by women during pregnancy in the study setting is unknown. Therefore, the aim of the study was to assess the prevalence of herbal medicine utilization and associated factors among pregnant women in Shashamane town, southern Ethiopia.
Methods: A community based cross sectional study was conducted among 358 pregnant women in, shashamane town, southern Ethiopia from august 1-30/2020. Data was collected using semi structured interviewer administered questionnaire, entered into Epi-data version 3.1 and exported to statistical package for social science (SPSS) version 20 for analysis. Bivariate and multivariate logistic regression analysis was performed. P-value < 0.05, at 95% confidence interval was considered as cut off point to declare the presence of statistically significant association.
Result: This study revealed that prevalence of herbal medicine utilization during current pregnancy was 16.8%% (95% CI: 13.5-19.3). Counselling about the risk of herbal medicine during antenatal care follow up (AOR=2.51, 95% CI: 1.08-5.84), history of health problem during their current pregnancy (AOR=2.34, 95% CI: 1.56-3.18), and previous experience (AOR=4.50, 95% CI: 3.67-9.46) were significantly associated with utilization of herbal medicine during pregnancy.
Conclusion and recommendation: The prevalence of herbal medicine utilization during pregnancy was found to be low compared to most of the previous studies conducted in Ethiopia. Therefore it is necessary to provide adequate counseling for all pregnant women attending antenatal care regarding the risks associated with herbal drug use on mother and fetus.
Herbal medicine, Associated factors, Pregnant women, Ethiopia
ANC: Antenatal Care; AOR: Adjusted Odd Ratio; CI: Confidence Interval; COR: Crude Odd Ratio; ETB: Ethiopian Birr; SPSS: Statistical Package for Social Science; WHO: World Health Organization.
World health organization (WHO) define self-medication as the fact of taking medicines by oneself to treat the self-diagnosed disorders without prescription or medical consultation [1].
The prevalence of self-medication is alarmingly high throughout the world. It ranges from 8.5 to 98%, showing variation with different subgroups of the population and between a developed versus developing region [2,3]. Beside conventional medicine, herbal drugs are also used for self-medication in low and middle income countries, were many users believe herbs to be more potent than conventional drugs and have no adverse effects [4,5]. Herbal medicines, which is part of traditional medicines are defined as plant-derived material or preparations perceived to have therapeutic benefits; they often contain raw or processed ingredients from one or more plants [6].
The use of herbal medicines is believed to be increasing in many developing and industrialized countries, yet little is known about their use and safety especially during pregnancy [7]. It is known that between 65 and 80% of the world's population use herbal medicines as their primary form of health care [8]. Herbal drugs are commonly used for self-medication in developing countries [9,10]. The wide use of herbal drugs in pregnancy is also observed in developed countries [5]. Evidence from the African continent suggests wide variability in use of herbal medicines during pregnancy, 20% in Uganda [7], 67.5% in Nigeria (8), and 41.8% in Egypt [11]. Approximately 80% of the population in Ethiopia use traditional medicine [12].
Studies have found that, prevalence of herbal medicine use during pregnancy shows inconsistent variation from region to region in Ethiopia ranging from 10.9% in Addis Ababa [13] to 73.1% in Hossana town [14]. Pregnant and breastfeeding women are especially vulnerable to harmful effects from herbal medicines as the safety profiles and appropriate dosages of most herbal medicines in these groups are not well established [5,15,16]. Herbs may contain substances that can cause abortion, premature birth, uterine contractions or injury to fetus due to the fact that the composition and safety parameters of these products are unknown [4,7].
There are different factors associated with herbal medicine utilization among pregnant women in different countries including age, income, education level, access to medicines, long waiting time in health facilities, perception towards risk of self-medication, previous medication use, gestational age and occupation [5,11,13].
There are several studies on herbal medicine use in Ethiopia among general population. However, very few studies were conducted among pregnant women. Moreover, Despite the fact that knowledge of potential side effects of many herbal medicines in pregnancy is limited and that some herbal products may be teratogenic, data on the extent of use of herbal medicines by women during pregnancy in the study setting is unknown and there is no scientific evidence on current prevalence and factors associated with herbal medicine utilization during pregnancy in study area. Therefore, the aim of the study was to assess the prevalence of herbal medicine use and associated factors among pregnant women in shashamane town, southern Ethiopia.
Study Setting and Period
Study was carried out in Shashamane town. The town is located 251 kilometre away from Addis Ababa, the capital of Ethiopia. There were eight kebeles (small administrative unit) in the town. According to Shashamane town health administration report; the health system of the town consists of two government hospitals (one general and one comprehensive specialized hospital), one private hospital, four health centers, 72 private pharmacy, 1 private health center and 71 medium private clinics. Based on the projection of figures published by central statistical agency in 2007, the total population of the town in 2020 was projected to be 279,814, of whom 141,150 were male and 138,665were female. The female population, within the reproductive age (15-49) accounts 44.7% (61,923) of the total female population and there were 9710 pregnant women in the town.
The study was conducted from August 1-30/2020.
Study Design and Population
Community based cross sectional study was employed. All pregnant women who have been residing for at least six months in Shashamane town, southern Ethiopia during the study period were source population while randomly selected pregnant women was study population.
Sample Size Determination and Sampling Procedure
Sample size was determined by using single population proportion formula considering P= prevalence of self-medication among pregnant women in Harar town which was 69.4% [16], 95% confidence level, 5% desired degree of accuracy. By considering 10% non-response rate, the final sample size was 360 Systematic random sampling technique was employed to select the study participants. Shashamane town has eight kebeles (small administrative unit in Ethiopia). From all these kebeles the list of pregnant women was obtained from health extension workers registration book with their respective address including the town house number. The determined sample size (N=360) was proportionally allocated to these kebeles based on the total number of pregnant women in each kebeles. It has been determined that the pregnant women were selected every 27th interval (i.e. by dividing the total number of pregnant women to the calculated sample size). The first pregnant woman interviewed was randomly selected using lottery method for each kebeles and continued every sampling interval. In the absence of eligible women in that household after three visits the next nearby higher house hold was interviewed.
Data Collection Tools and Procedures
Data was collected using semi-structured and pretested interviewer administered questionnaire which was adapted after reviewing previous literatures [13,16-19] and modified to fit the current study. The questionnaire was prepared in English language and translated to local language (Afan Oromo) including all relevant variables based on the study objectives. Data was collected by four BSc midwives and supervised by two master’s holders in reproductive health.
Data Quality Control
To verify the consistency of the questionnaire, it was prepared in English and translated in to Afan Oromo language by language experts, then back to English to check its consistency. Before printing the final version of the questionnaire, a pretest was done in Arsi Negele town on 5% (18 women) of the participants. According to the results of the pretest, the questionnaire was further modified (such as addition of more questions, reordering and clarity of the questions). Data collectors and supervisors were given training for two days before data collection on objective of the study, procedure of data collection, art of interviewing, confidentiality of information and clarification was given. Every day after data collection, questionnaires was reviewed and checked for completeness and relevance by supervisors and principal investigator.
Data Processing and Analysis
The data was checked for completeness manually and then coded, entered into Epi Data version 3.1software and exported to SPSS version 20 software for analysis. Descriptive statistics was computed to determine frequencies and summary statistics (mean, standard deviation, and percentage) to describe the study population in relation to socio-demographic and other relevant variables. Data was presented using tables, graphs and figures. Bivariate logistic regression analysis was employed to check crude association between self- medication and independent variables. Variables with P-value <0.25 in bivariate logistic regression analysis were entered to multivariable logistic regression analysis to control the possible effect of confounders and identify significant predictors of herbal medicine utilization. Odds ratio and the corresponding 95% confidence interval were used to quantify the degree and direction of association between dependent and independent variables. P-value < 0.05 was considered as cut point to declare the presence of statistically significant association.
Socio-demographic Characteristics
Out of 360 study participants, 358 pregnant women were participated in the study making the response rate of 99.4%. The Mean age of the study participants were 26.09 years with the standard deviation of ± 5.72 years (26.09 ± 5.72). Majority of the respondents, 129 (36%) were in the age range of 20-24 years and 163 (45.5%) of the women had attended primary school. Almost all, 353 (98.6%) of the study participants were married and nearly three-fourth, 274 (76.5%) of women were housewife in occupation. On the other hand nearly about one-fourth, 89 (24.9%) of the study participants have health insurance (Table 1). Previous Pregnancy and Gestational Age of Current
| Variables | Frequency (N=358) | Percentage (%) |
|---|---|---|
| Age of respondents in years | ||
| 15-19 20-24 25-29 30-34 35-39 40 and above |
33 129 101 54 35 6 |
9.2 36 28.2 15.1 9.8 1.7 |
| Marital status | ||
| Married Divorced Widowed |
353 3 2 |
98.6 0.8 0.6 |
| Occupation | ||
| housewife Government Employee NGO employee Merchant |
274 32 10 42 |
76.5 8.9 2.8 11.8 |
| Educational status of women | ||
| Can’t read and write Can read and write Primary Secondary College and above |
59 32 163 56 48 |
16.5 8.9 45.5 15.6 13.4 |
| Educational status of husband | ||
| Can’t read and write Can read and write Primary Secondary College and above |
42 36 126 77 77 |
11.7 10.1 35.2 21.5 21.5 |
| Average monthly income** | ||
| = 1,380 1,381-6,900 6,901-13,800 |
116 215 27 |
32.4 60.1 7.5 |
| Total | 358 | 100% |
Table 1. Socio-demographic characteristics among pregnant women in Shashamane town southern Ethiopia, 2020 (N=358).
Pregnancy
Out of 358 pregnant women participated in the study, 166 (46.4%) were in the second trimester of pregnancy. Most of the respondents, 275 (76.8%) were multi-gravida and 180 (50.3 %) were multi-parous. About 32 (8.9%) pregnant women had encountered previous pregnancy- and delivery-related problems while 117 (32.7%) of pregnant women experienced health problem during current pregnancy.
Anc Service Utilization of the Study Subjects
Majority of the respondents, 313 (87.4%) were following the ANC service for the current pregnancy while 45 (12.6%) were not. Majority of them, 150 (41.9%) were following the ANC service at health center while 135 (37.7%) were at Hospital. Only 28 (7.8%) were following ANC at private clinic or hospital in the study area. Regarding health education on risk of hernal medicine use during pregnancy, about 180 (52.5%) was given the education about the risk of associated with herbal drug use (Table 2).
| Variables | Frequency (N=358) | Percentage (%) |
|---|---|---|
| Gravidity (n=358) | ||
| Primi-gravida multi-gravida |
83 275 |
23.2 76.8 |
| Parity (n=358) | ||
| Nulli-para Primi-para Multi-para |
92 86 180 |
25.7 24 50.3 |
| History of abortion (n=358) | ||
| No Yes |
285 75 |
79.1 20.9 |
| Number of Children (n=358) | ||
| No child 1-3 >3 |
93 202 63 |
26 56.4 17.6 |
| ANC follow up (n=358) | ||
| No Yes |
45 313 |
12.6 87.4 |
| Health education about risk of self medication during pregnancy (n=313) | ||
| No Yes |
125 188 |
39.9 60.1 |
| Experienced health problem during previous pregnancy (n=289) | ||
| No Yes |
257 32 |
88.9 11.1 |
| Experienced health problem during this pregnancy (n=358) | ||
| No Yes |
241 117 |
67.3 32.7 |
Table 2. Distribution of pregnancy related conditions and ANC service utilization pattern among pregnant women in Shashamane town, southern Ethiopia, 2020.
Prevalence of Herbal Medicine Utilization during Pregnancy
Among 358 pregnant women interviewed, 60 (16.8%) (95% CI: 13.5-19.3) used herbal medicines during their current pregnancy and from a total of 275 pregnant women with two and above gravida, 119 (33.2%) had a history of herbal medicine use during a previous pregnancy. Among the 60 pregnant women who used herbal medicines, the reasons reported were easily availability of herbal medicines without physician prescription (53/60; 88.3%), fewer cost (29/60; 48.3%), believing that herbal medicines carry less risk than modern medicines (16/60; 26.7%) and herbal medicines are more effective than conventional medicines 13 (21.7%)
Among the 60 pregnant women who used herbal medicines, 11 (18.3%) believe that the use of herbal medicine during pregnancy could cause harm to fetus and mother and 4 (6.7%) experienced side effect like difficult labor, abdominal cramp, decreased fetal movement, nausea and vomiting after using herbal medicine during their current pregnancy.
The most widely used herb was ginger (Zingiber officinale) 34 (56.7%) followed by garlic (Allium sativum) 31 (51.7%) and moringa (Lepidium sativum) 29 (48.3%) (Table 3).
| Herbal medicine* | Scientific name of herbal medicines | Frequency (n=60) | Percentage (%) | Trimester | ||
|---|---|---|---|---|---|---|
| 1st | 2nd | 3rd | ||||
| Ginger Kosso Garlic Tena adam Sabanaki Damakassie Feto Moringa Others** |
Zingiber officinale Hagenia abyssinica Allium sativum Ruta chalepensis Tyumen Ocimum lamiifolium Lepidium sativum |
34 21 31 24 21 16 27 29 3 |
56.7 35 51.7 40 35 26.7 45 48.3 5 |
2 4 3 1 5 2 1 9 0 |
14 11 11 10 9 7 10 8 2 |
18 6 17 13 7 7 16 12 1 |
Table 3. Herbal medicines used by the pregnant women by trimester, shashamane town, 2020 (n = 60).
Indication for Using Herbal Medicines during Pregnancy
Among the 60 pregnant women who used herbal medicines, constipation 48(80%) was mentioned as the main reason followed by common cold 16 (26.7%) and heart burn 14(23.3%) (Figure 1).
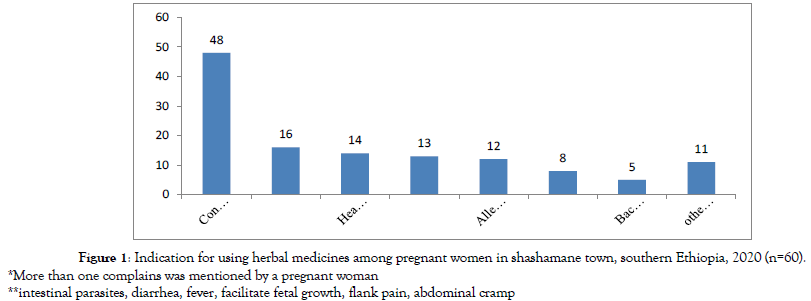
Figure 1: Indication for using herbal medicines among pregnant women in shashamane town, southern Ethiopia, 2020 (n=60).
*More than one complains was mentioned by a pregnant woman
**intestinal parasites, diarrhea, fever, facilitate fetal growth, flank pain, abdominal cramp
Regarding the source of herbal medicine, the most common sources were market or shop 49 (81.7%), home 48 (80%), friend 27 (45%) and neighbor 24 (40%).
Factors Associated With Utilization of Herbal Medicines during Pregnancy
In bivariate analysis counseling at ANC visit about the risk of herbal medicine during pregnancy, history of health problem during the current pregnancy, history of health problem during the previous pregnancy, previous experience, lack of enough and skilled health professionals at government health institutions and long waiting time at government health institutions were significantly associated with utilization of herbal medicine during pregnancy. The result of multivariate logistic regression revealed that the odd of using herbal medicine was found to be high if the pregnant women were not counseled about the risk of herbal medicine during pregnancy (AOR= 2.51, 95% CI=1.08-5.84). Pregnant women with history of health problem during their current pregnancy were 2.34 times more likely to use herbal medicine (AOR= 2.34, 95% CI=1.56- 3.18). Moreover, the finding of this added that the odds of using herbal medicine was about 4.5 times higher if the pregnant women had previous experience of using herbal medicines (AOR= 4.50, 95% CI= 3.67-9.46) (Table 4).
| Variables | Utilization of herbal medicine | COR (95% CI) | AOR (95% CI) | ||
|---|---|---|---|---|---|
| No (%) | Yes (%) | ||||
| Counseling at ANC visit about risk of herbal medicine | No | 96(76.2%) | 30(23.8%) | 2.34(1.29-4.32) | 2.51(1.08-5.84)** |
| Yes | 166(88.3%) | 22(11.7%) | 1.00 | 1.00 | |
| history of health problem during current pregnancy | No | 215(89.2%) | 26(10.8%) | 1.00 | 1.00 |
| Yes | 83(70.9%) | 34(29.1%) | 3.39(1.92-5.99) | 1.34(1.56-3.18)* | |
| history of heath problem during previous pregnancy | No | 216(84%) | 41(16%) | 1.00 | 1.00 |
| Yes | 20(62.5%) | 12(37.5%) | 3.16(1.44-6.96) | 2.65(0.85-8.23) | |
| Previous Experience | No | 221(92.5%) | 18(7.5%) | 1.00 | 1.00 |
| Yes | 77(64.7%) | 42(35.3%) | 6.69(3.64-12.35) | 4.50(3.67-9.46)** | |
| Is there enough and skilled professionals at government health institutions | No | 87(75%) | 29(25%) | 2.27(1.29-3.99) | 1.76(0.72-4.31) |
| Yes | 211(87.2%) | 31(12.8%) | 1.00 | 1.00 | |
| Waiting time at government institutions | Normal | 182(87.5%) | 26(12.5%) | 1.00 | 1.00 |
| Short | 23(95.8%) | 1(4.2%) | 0.34(0.04-2.35) | 0.01(0.91-10.91) | |
| Long | 93(73.8%) | 33(26.2%) | 2.48(1.40-4.39) | 1.21(0.49-2.94) | |
| Do community drug retail pharmacies sell drug without physician prescription | No | 238(85.3%) | 41(14.7%) | 0.37(0.18-0.77) | 0.49(0.18-1.39) |
| Yes | 28(68.3%) | 54(16.9%) | 1.00 | 1.00 | |
Table 4. Factors associated with herbal medicines utilization among pregnant women in shashamane town, Southern Ethiopia, 2020.
This study revealed that prevalence of herbal medicine during pregnancy was 60 (16.8%). This is in line with the study conducted among pregnant women in Hispanic, Texas 19% [20], Effutu and Agona Municipalities of Ghana 19% (21). It is lower than the study conducted in Palestine 72.3%(22), Jeddah, Saudi Arabia 40% (4), Alexandria, Egypt 41.8% (11), Nigeria 67.5%(8), and Harar, Eastern Ethiopia 40.6% (16), Hossana town, southern Ethiopia 73.1% (14), However it is higher than study carried out in Iran 10% (23) and Addis Ababa, Ethiopia 10.9% (13). This discrepancy could be due to the difference in study setting, availability of herbal medicines, and socio-cultural difference in the study population.
The main reasons reported for self-medication using herbal medicines were easily availability of herbal medicines without physician prescription and fewer costs. This is consistent with finding of the study done in Addis Ababa, Ethiopia [20-23].
Ginger (Zingiber officinale), garlic (Allium sativum) and Moringa (Lepidium sativum) were the most common herbs used during pregnancy. This is consistent with two studies conducted in Ethiopia. This study indicated that pregnant women who didn’t counseled about the risk of herbal medicine were about 2.51 times more likely to use herbal medicines compared to those who were counseled by health care providers during their ANC follow up. This could be due to the health education provided during their ANC follow. This shows use of herbal medicine could be minimized if pregnant women were given proper health education on possible risk of herbal medicine on fetus and mother during antenatal care follow up.
Pregnant women with history of health problem during their current pregnancy were 2.34 times more likely use herbal medicine. This is supported by the result of study conducted in Goba, south east Ethiopia (19). Finally the finding of this study added that the odds of using herbal medicine was about 4.5 times higher if the pregnant women had previous experience of using herbal medicines compared to their counter parts. This is in line with study conducted in Goba, Ethiopia and Uganda where previous history of herbal use where significantly associated with their current herbal medicine utilization.
The limitation of this study might be the study being prone to recall bias that may affect the result of this study, because the pregnant women might not remember the types of drug they used. The other possible limitation could be women in early pregnancy might not have the chance yet to use medications consequently affecting the reported results on drugs commonly used in pregnancy.
Prevalence of herbal medicine utilization during pregnancy was found to be low compared to most of the previous studies conducted in Ethiopia. The finding of this study showed that receiving counseling during antenatal care follow up, history of health problem during current pregnancy and previous experience were significantly associated with using herbal medicines. Therefore it is necessary to provide adequate counseling for all pregnant women attending antenatal care regarding the risks associated with using herbal medicine during pregnancy on mother and fetus.
We would like to express our heartfelt gratitude to Hawassa University for the fund support to carry out the research.
We are also grateful to the staff of Shashamane town health office for their cooperativeness and providing important information.
It is also our pleasure to acknowledge data collectors, supervisors and study participants for giving their time during study period.
Gemechu Gelan Bekele (GGB) conceived the idea and drafted proposal. Both authors (GGB and DNG) contributed to the design of the study and the interpretation of data. GGB performed the data analysis and drafted the manuscript. Both authors critically revised the manuscript and approved the final version.
Hawassa University and the funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
The authors declare that they have no conflict of interests.
Not applicable
Full data for this research is available through the corresponding author up on request.
Formal letter of cooperation was obtained from Hawassa University College of medicine and health sciences ethical institutional review board (reference number, IRB/092/12) to Shashamane town health office. The town health office sent letter of permission to all kebeles in which the actual data collection was undertaken. Informed verbal consent was obtained from all study participants by reading written informed consent form, prior to starting of the interview.
Citation: Bekele GG, Gonfa DN (2021) Prevalence of Herbal Medicine Utilization and Associated Factors among Pregnant Women in Shashamane Town, Southern Ethiopia, 2020; Challenge to Health Care Service Delivery. J Women's Health Care 10:551. doi: 10.35248/2167-0420.21.10.551.
Received: 03-Sep-2021 Accepted: 17-Sep-2021 Published: 23-Sep-2021 , DOI: 10.35248/2167-0420.21.10.551
Copyright: © 2021 Bekele GG, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.