Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Research Article - (2024)Volume 15, Issue 3
Objectives: Little information about the prevalence of myopia in Latin America is available and this study aims to detect the prevalence of refractive errors under cycloplegia in Southern Brazil. Main goal is prevalence of myopia, including the classification in pre-myopia, low myopia and high myopia and associated risk factors. Secondary objective is to describe the prevalence of hyperopia and astigmatism and compare them to the same variables as myopia.
Materials and methods: A prospective cross sectional convenient sampling recruited 330 public school children between 2020 and 2021, aged 5 to 20 years old. All children underwent a comprehensive eye examination including cycloplegia and a detailed lifestyle questionnaire was applied.
Results: Prevalence of myopia was 17.4% (Confidence Interval (CI) 13.8-21.7%). Low myopia (-0.50 D to -5.75 D) was 15.2% (CI 11.9-19.3%) and high myopia (-6.00 D or worse) was 2.1% (CI 1.1-4.1%). The prevalence of hyperopia was 7.7% (CI 5.4-10.9%) and of astigmatism, either myopic, mixed or hyperopic, was 25.6% (CI 21.4-30.2%). The relationship between refractive errors and sex, ethnicity, age, time of electronics use/daily, axial length and corneal Kmax are presented and compared among myopia, hyperopia and astigmatism. Data on pre-myopia is also disclosed. Median, asymmetry and kurtosis were applied.
Conclusion: There is a correlation of myopia with sex, ethnicity, age and time of electronics use daily. Astigmatism was more prevalent in males and hyperopia had a higher magnitude in males too, but no association with ethnicity and electronics use was identified. This is the highest reported prevalence of myopia under cycloplegia in Brazil to date and Brazilian school children seem to be less hyperopic than in ancient publications, which represent a new reality in refractive errors distribution in the country.
Refractive errors; Myopia epidemic; Hyperopia; Astigmatism; Epidemiology; Keratoconus
Refractive errors are the product of a mismatch between the axial length of the eye and its optical power, creating blurred vision. Uncorrected refractive errors are the second leading cause of worldwide blindness. There are three main types of refractive errors are hyperopia or farsightedness and myopia or nearsightedness, which represents spherical errors, astigmatism involve an optical asymmetry and cause blurred distance and near vision. Although considered as an independent category, astigmatism may be a feature of both hyperopic and myopic eyes [1]. Both age and ethnic-related differences in the prevalence of different types of refractive errors have been described. However, it is important to recognize the potential role of shared environments, which may also vary with ethnicity [2].
The refractive error currently attracting significant scientific interest is myopia, mostly owing to the recent rise in its prevalence worldwide and associated ocular disease burden [3-15]. Myopia was recognized as a public health issue by the World Health Organization (WHO) in 2015 and is known to significantly increase the risk of complications and morbidity in the fourth decade of life, such as cataract, glaucoma, retinal detachment and myopia maculopathy. East urban Asia has the highest prevalence of myopia in the world and alongside this, a growing prevalence of sight threatening myopia related pathologies.
Japan, China, Singapore, South Korea and Taiwan report prevalence of 80% or more young adults with myopia. Countries of Europe and the United States have myopia rates of 30.6% and 25.4%, respectively, which rises to almost 50% if only the young population is considered (25-29 years old). More recently, due to the COVID-19 lockdowns, the incidence of myopia has increased approximately 4% in Chinese children aged 3 to 6 years. The prevalence of myopia is lower in middle and low-income countries ranging from 1.4% to 14.4% in Latin America and 3.4% to 11.4% in Africa [16-18].
Brazil has always been considered a hyperopic country and there is little information about myopia [19,20]. Studies about refractive errors used different methodology, examined different populations, were developed in different periods of time and regions of the country and did not all use cycloplegia [21-25]. Vilar, et al., [24] compared two studies conducted in the same ophthalmology hospital in Goiania (Goias) in the evaluation carried out between 1995 and 2000, the prevalence of myopia was 3.6% in 2014, the study found the prevalence of myopia was 9%. Garcia, et al., [23] reported the prevalence of myopia in Northeastern Brazil in 2001 was 13.3% in randomly selected students.
A recent review paper reported that the prevalence of myopia in Brazil was 3.6% to 9.6% but it was based on those publications from several decades ago. Recent papers describe higher prevalence, with rates that varied between 15.2% and 20.4%. The first, a retrospective study carried out in Sao Paulo, evaluated school children under cycloplegia. The second, a prospective cross-sectional study carried out in the equatorial region, evaluated school children under no cycloplegia.
Myopia prevalence seems indeed to be growing over the decades in Brazil, which inversely affects hyperopia rates. Prevalence of astigmatism seems to be stable. Population-based eye health data at the country level is needed to develop strategies for public health interventions [26].
The present study discloses data on all ametropias detected in public school children from the metropolitan region of Porto Alegre, southernmost capital of Brazil. It also associates them to different variables and compares risk factors between myopia, hyperopia and astigmatism.
This convenience sample cross-sectional study was conducted in children from public schools in the region of Porto Alegre, Rio Grande do Sul, Brazil. The study was approved by the Hospital de Clinicas de Porto Alegre Ethics Committee, which adhered to the tenets of the Declaration of Helsinki. The children's guardians provided written informed consent. All children underwent a comprehensive ophthalmologic examination and were not previously screened with visual acuity. A questionnaire on sociodemographic characteristics was completed by participants.
Sampling
Participants were public school children in the region of Porto Alegre and the study was part of a charitable program that provided spectacles for refractive disorders. Schools were selected by the Public Ministry and the entire classes were referred for evaluation. Considering the prevalence of myopia in Brazilian school children was 20.4%, a sample size of 250 students was needed to achieve a 95% confidence level and a confidence interval of 10%. The final number of participants determined was 278 to allow for up to 10% non-participation [27].
The study began in 2020 and resumed in 2021. Children included in the study were aged 5 to 20 years. Exclusion criteria were severe neuro psychomotor developmental disorders, subjects with congenital eye disorders (cataract, an ophthalmic cavity, strabismus and glaucoma) and contact lens wear on the date of the exam. The examinations were conducted by medical residents and staff using a standardized protocol at 5 different medical centers: Hospital de Clínicas de Porto Alegre, Hospital Nossa Senhora da Conceicao, Complexo Santa Casa, Centro de Olhos Rio Grande do Sul and Instituto Ivo Correa Meyer. A questionnaire on sociodemographic characteristics was completed by participants.
Measurements
Binocular Uncorrected Visual Acuity (UCVA) and Best-Corrected Visual Acuity (BCVA) for distance were determined using a standard snellen chart. School children with UCVA of 0 Logarithm of the Minimum Angle of Resolution (LogMAR) without complaints did not undergo cycloplegia. School children with visual acuity of 0.10 LogMAR or worse or 0 LogMAR with visual complaints, were instilled with 1% tropicamide (1 drop in each eye, repeated 5 minutes later) and evaluated after 25-30 minutes, with auto-refraction (3 measurements per eye), followed by binocular subjective refraction. Closed-field, non cycloplegic refraction was measured with an autorefractor (Huvitz 7000, South Korea), with at least 3 measurements per eye. In hyperopic patients, binocular subjective dynamic refraction was performed prior to pupil dilation with mydriatic eye drops. All participants underwent corneal tomography using Galilei G4 (Ziemer, Germany) for eventual keratoconus diagnosis. Keratometric keratoconus was defined as maximum keratometry>47.2 D. Ocular biometry using ultrasonic AL-100 biometer (Tomey, Japan) was used for axial length measurement, 3 measurements per eye. Subsequent evaluation consisted of retinal mapping and slit lamp bio-microscopy to exclude other ocular pathologies.
A questionnaire about demographics and time of electronics use daily was completed by the participants and their guardians.
Statistics
The data were entered into the Excel program and later exported to the International Business Machines corporation (IBM) Statistical Package for the Social Sciences (SPSS) version 20.0 for statistical analysis. Categorical variables were described by frequencies and percentages. The normality of the variables was checked using the Kolmogorov Simonov test. Quantitative variables with normal distribution were described by the mean and standard deviation and those with asymmetric distribution by the median and interquartile range. Kurtosis and asymmetry measurements were calculated for cycloplegic myopia, hyperopia and astigmatism. Quantitative variables with normal distribution were compared between groups using student's t test for independent samples and those with asymmetric distribution using the mann-whitney test. Categorical variables were associated using the chi-square test and fisher's exact test. The correlation between quantitative variables was performed using spearman's correlation coefficient. To evaluate the relationship between different factors and the prevalence of myopia, hyperopia and astigmatism, poisson regression with robust variance was used and the crude and adjusted prevalence ratios were calculated. A significance level of 5% was considered for the comparisons established.
Definitions
Myopia: Myopia was defined as a cycloplegic spherical refraction equal to or worse than -0.5 D. The cut off for high myopia was defined as -6.00 D or worse [28].
Pre-myopia: Pre-myopia was defined as cycloplegic refraction between -0.50 D and +0.75 D.
Hyperopia: Spherical refraction greater than or equal to +2.00 D was defined as hyperopia.
Astigmatism: 20 astigmatisms was defined as -1.00 D cylindrical diopters or more [29].
Keratoconus: Kmax of 47.2 D or more would be considered keratoconus [30,31].
Participants
A total of 333 school children were evaluated in this study and 52% of those were males. Ethnicity based on self-classification was 37.5% white, 39% afro-descendants (black+mixed) and 0.4% other; 23.1% did not classify themselves. Mean age was 12.74 years (95%, CI: 12.38-13.10). More than half were aged 10-15 years (53.4%); 20.4% were younger than 9 years and 26.1% were older than or equal to 16 years. Most participants were from the hospital de Clinicas de Porto Alegre (52%). Three children were excluded from the analysis due to technical difficulties during the measurements (Table 1).
| Participants | Number | Rate (%) |
|---|---|---|
| Sex | ||
| Male | 173 | 52 |
| Female | 160 | 48 |
| Skin color | ||
| White | 125 | 37.5 |
| Afro-descendant | 131 | 39 |
| Not referred | 77 | 23.1 |
| Age | ||
| ≤ 9 | 68 | 20.4 |
| 10 to 15 | 178 | 53.4 |
| ≥ 16 | 87 | 26.1 |
| Medical center | ||
| HCPA | 174 | 52% |
| HNSC | 40 | 12% |
| CSC | 39 | 12% |
| CORS | 43 | 13% |
| IICM | 37 | 11% |
Note: HCPA: Porto Alegre Clinical Hospital; HNSC: Hospital Nossa Senhora da Conceicao; CSC: Complexo Santa Casa; CORS: Centro de Olhos do Rio Grande do Sul; IICM: Instituto Ivo Correa Meyer.
Table 1: Demographics of the 333 study participants.
Approximately 51% of children achieved UCVA 0 LogMar bilaterally and 34.5% wore spectacles. Average screen time use was 4.92 hours (95%, CI: 4.48-5.35).
Prevalence of refractive errors
Prevalence of myopia was 17.4% (CI: 13.8-21.7%). Low myopia corresponded to 15.2% (CI: 11.9-19.3%), while high myopia was present in 2.1% (CI: 1.1-4.1%). Hyperopia prevalence was 7.7% (CI: 5.4-10.9%) and astigmatism prevalence was 25.6% (CI: 21.4-30.2%). Median, asymmetry and kurtosis for all refractive errors (Tables 2 and 3).
| Refractive errors | Rate (%) | 95% CI |
|---|---|---|
| Myopia (≥ -0.5 D) | 17.4 | 13.8-21.7 |
| High myopia (≥ -6.0 D) | 2.1 | 1.1-4.1 |
| Low myopia (-0.5 D-5.75 D) | 15.2 | 11.9-19.3 |
| Hyperopia (≥ +2.00 D) | 770.00% | 5.4-10.9 |
| Astigmatism (<-1.0 D) | 25.6 | 21.4-30.2 |
Note: CI: Confidence Interval.
Table 2: Prevalence of refractive errors.
| Refractive errors | Median (IQR) | Asymmetry | Kurtosis | |
|---|---|---|---|---|
| Myopia | -1,75 (-3,50-(-1,00)) | -1,84 | 3,06 | |
| Hyperopia | 2,75 (2,00-4,00) | 1,58 | 2,03 | |
| Astigmatism | -1,75 (-3,00-(-1,00)) | -1,19 | 1,05 | |
| Myopia SE | -0,63 (-1,63-(-0,13)) | -3,09 | 11,08 | |
Note: IQR: Interquartile Range; SE: Spherical Equivalent.
Table 3: Median, asymmetry and kurtosis for refractive errors under cycloplegia.
Risk factors associated with refractive errors
Mean myopia was -2.73 (Standard Deviation (SD) 2.69), with no difference in magnitude between males and females, but the prevalence of myopia was higher in females (41% in females and 22.2% in males with p<0.01). Females presented a relative risk of myopia of 1.6 (CI: 1.00-2.57%) (p=0.047) and each additional hour of screen time increased a child's chance of having myopia by 6.5% (CI: 1.01-1.12%) (p=0.01). Hyperopia was lower in females with p=0.006 (+2.50 for females and +3.50 for males), but the prevalence was not different between sexes (p=0.039). Astigmatism was more prevalent in males (49.5% in males and 31.6% in females with p<0.01) (Table 4).
| Refractive errors | Female | Male |
|---|---|---|
| Myopia | -2.00 dp | -1.50 dp |
| 41,0% | 22,2% | |
| Hyperopia | +2.50 dp (+2.00-(+3.00)) | +3.75 dp (+2.56-(+5.88)) |
| 14,4% | 13.3% | |
| Astigmatism (either myopic, mixed or hyperopic) | -1.50 cil dp | -2.00 cil dp |
| (-2.50-(-1.00)) | (-3.00-(-1.25)) | |
| 31.6% | 49.5% |
Table 4: Myopia, hyperopia and astigmatism median, CI and their differences among sexes.
The prevalence of myopia, hyperopia and astigmatism and their relationship with skin color, age (categorized as above and below 12 years old) and screen time (categorized as below and above 4 h) was also evaluated. In a poisson regression model adjusted for sex, color, age and screen time, it is possible to detect that female had 2.26 times the prevalence of myopia as male Caucasians and mixed have 1.66 times the prevalence of blacks those aged 12 or over had 1.68 times the prevalence of those under 12 and those who watched 4 hours or more of screen time had 2 times the prevalence of those who watched less than 4 hours. All factors were found to be significantly related to myopia. There was a significant association between skin color and myopia (p=0.027, chi-square test). By the analysis of standardized residues adjusted in the white category has more myopia than expected and less than expected in the black category (adjusted residuals of 2.6 for whites and -2.2 for blacks). Of the eyes corresponding to patients aged 5 to 8 years, 53.6% had pre myopia, while in the group aged 9 to 11 years 68.6% had pre-myopia, with a statistically significant difference (p=0.027). Nevertheless, of the eyes corresponding to patients aged 5 to 8 years, 27.7% had myopia, while in the group aged 9 to 11 years, 21.4% had myopia, with no statistically significant difference (p=0.510) (Tables 5-7).
| Hyperopia | Prevalence (%) | CPR (CI 95%) | APR (CI 95%) | P |
|---|---|---|---|---|
| Sex | ||||
| Female | 14,4 | 1.08 (0.65-1.80) | 1.36 (0.79-2.35) | 0.273 |
| Male | 13.3 | - | - | |
| Skin color | ||||
| Caucasian | 12.4 | 0.77 (0.43-1.38) | 0.74(0.41-1.34) | 0.323 |
| Afro-descendant | 16.1 | - | - | |
| Age | ||||
| 12 years or more | 11.4 | 0.68 (0.41-1.13) | 0.73(0.42-1.27) | 0.264 |
| Less than 12 years | 16.9 | - | - | |
| Time of electronics use daily | ||||
| 4 h or more | 13.6 | 0.87 (0.52-1.44) | 0.95 (0.54-1.68) | 0.863 |
| Less than 4 h | 15.7 | - | - | |
Note: CI 95%: Confidence Interval of 95%; CPR: Crude Prevalence Rate; APR: Adjusted Prevalence Rate.
Table 5: Multivariable analysis of factors associated with hyperopia (poisson regression with robust variance).
| Astigmatism | Prevalence | CPR (CI 95%) | APR (CI 95%) | P |
|---|---|---|---|---|
| Sex | ||||
| Female | 31.6 | 0.64 (0.50-0.81) | 0.61 (0.46-0.82) | 0.001 |
| Male | 49.5 | - | - | |
| Skin color | ||||
| Caucasian | 36.9 | 0.96 (0.71-1.31) | 0.95 (0.70-1.31) | 0.772 |
| Afro-descendant | 38.3 | - | - | |
| Age | ||||
| 12 yr or more | 39.4 | 0.93 (0.74-1.18) | 1.06 (0.78-1.43) | 0.718 |
| Less than 12 yr | 42.2 | - | - | |
| Time of electronics use | ||||
| 4 h or more | 38.7 | 0.95 (0.74-1.21) | 1.14 (0.85-1.53) | |
| 0.391 | ||||
| Less than 4 h | 41.0 | - | - | |
Note: CI 95%: Confidence Interval of 95%; CPR: Crude Prevalence Rate; APR: Adjusted Prevalence Rate.
Table 6: Multivariable analysis of factors associated with astigmatism (poisson regression with robust variance).
| Myopia | Prevalence (%) | CPR (CI 95%) | APR (CI 95%) | P |
|---|---|---|---|---|
| Sex | ||||
| Female | 41.0 | 1.85 (1.34-2.54) | 2.26 (1.50-3.40) | <0.001 |
| Male | 22.2 | - | - | |
| Skin color | ||||
| Caucasian | 32.4 | 1.60 (1.02-2.53) | 1.66 (1.09-2.55) | 0.019 |
| Afro-descendant | 20.2 | - | - | |
| Age | ||||
| 12 years or more | 37.9 | 1.64 (1.18-2.28) | 1.68 (1.17-2.40) | 0.005 |
| Less than 12 years | 23.2 | - | - | |
| Time of electronics use | ||||
| 4 h or more | 38.7 | 1.91 (1.33-2.75) | 2.01 (1.31-3.09) | 0.001 |
| Less than 4 h | 20.3 | - | - | |
Note: CI 95%: Confidence Interval of 95%; CPR: Crude Prevalence Rate; APR: Adjusted Prevalence Rate
Table 7: Multivariable analysis of factors associated with myopia (poisson regression with robust variance).
Axial length showed significant differences between low (23.58 mm-SD 1.03) and high myopia (26.62 mm-SD 1.01) (p<0.01). The low myopia group had a significantly smaller mean axial diameter than the high myopia group (23.58 ± 1.01 vs. 26.62 ± 1.01, p<0.001). Kmax was not significantly different, with a mean of 45.24 D in the low myopia group (SD 1.93) and 45.92 D in the high myopia group (standard deviation of 2.58) (p=0.371). Myopic eyes had significantly higher values of axial diameter than hyperopic eyes (p<0.001) and Kmax was higher in eyes with myopia compared to hyperopia (p=0.019) (Figures 1 and 2).
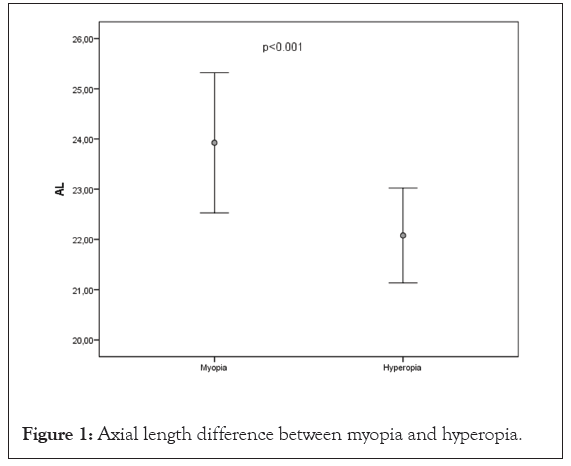
Figure 1: Axial length difference between myopia and hyperopia.
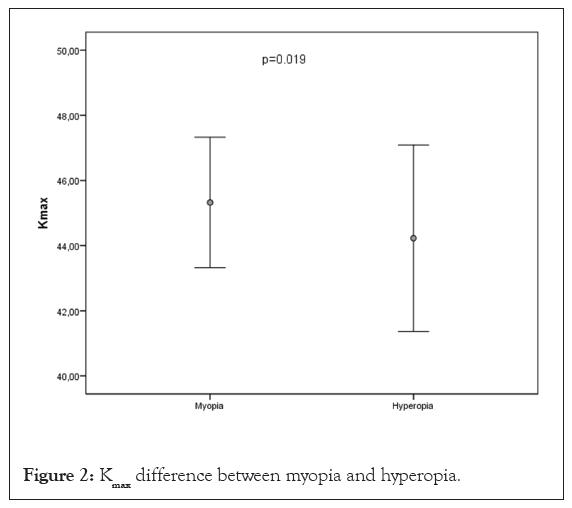
Figure 2: Kmax difference between myopia and hyperopia.
Of the eyes corresponding to patients aged 5 to 8 years, 68.6% had pre myopia while 21.4% had myopia; in the group aged 9 to 11 years, 53.6% had pre myopia and 27.7% had myopia, with a statistically significant difference for pre-myopia (p=0.027) and myopia (p=0.510).
There was a significant, inverse and weak correlation between age and spherical equivalent of myopia (Correlation Coefficient (rs)=-0.18; p=0.001). Regarding the correlation between age and astigmatism, there was a significant inverse and weak correlation (rs=-0.11; p=0.024) too. No difference was found between age and hyperopia.
There is limited information regarding the prevalence of myopia in Brazil and this is the first study on myopia prevalence in southern Brazil. Papers about refractive errors in other regions of the country were conceived in different periods of time and used different methodology (no cycloplegia; retrospective analysis; adults included and patients from ophthalmology centers). The data collected in Porto Alegre is representative of public school children from the entire country in terms of the ethnic mix, since the proportion of Caucasians and afro descendants is similar to the national distribution.
No previous Brazilian papers have compared Caucasians and afro descendants with blacks. This difference was not found among the other refractive errors and ethnic distribution. This is the first time that kurtosis and asymmetry are calculated for ametropias data in Brazil [32-37].
Myopia was more prevalent in females, which agrees with the literature. Astigmatism was more common in males, which also agreed with previous publications, newborns and toddlers tend to have more astigmatism than older children. Hyperopia did not differ in prevalence among sexes, but the degree was higher in males, which is novel information. Hyperopia and astigmatism classification in mild, intermediate and high was not done because the focus of the present work was to detail myopia and its possible future overload to the health system [38].
Axial length was different between myopia and hyperopia, myopic eyes were longer than hyperopic, as expected, as much as low and high myopia also differed in axial length [39,40]. The present study used ultrasonic biometry because it was the available device in the hospital. Although optic biometry is preferred, previous studies demonstrated similar reliability between ultrasonic and optic biometers in measuring axial length in children [41].
Maximum keratometry was higher in myopes than in hyperopes, but we found no keratoconus. Since progressive myopia and astigmatism are usually the first sign of keratoconus and both keratoconus and myopia might affect the same age population, the authors decided to rule out this diagnosis by performing scheimpflug tomography in all participants. Those are novel data in papers about refractive errors in Brazil and among worldwide literature in the field.
Demanding education and many hours of near work are known to strongly relate to myopia [42]. Public schools in Brazil generally have weak academic outcomes. Although Brazil spends about 5% of its Gross Domestic Product (GDP) in public education, high staff workload and relatively poor remuneration generally lead to weak academic results.
Public schools tend to have one four-hour session of classes per day. Nevertheless, this paper presents the same prevalence of myopia as a relatively recent Canadian paper published by Yang, et al., [43] which is impressive. No private school children were included in this study to avoid a possible bias, since they had access to education online during the pandemic and have a better quality of education overall, with more hours of schooling per day and more home activities. Private school children represent a small proportion of students in Brazil, 17%. The authors plan to perform another study in private schools.All social classes have access to cellular phones in Brazil and the children spend most of their spare time indoors, using near work electronics for recreation. The publication of Lanca, et al., [44] suggests that in countries where the prevalence of myopia is lower, it might be associated with the number of hours of electronics use daily, which the authors believe to be a reality for Brazilian school children. The use of electronics for 4 hours or more was associated with a higher prevalence of myopia and this might also explain the apparent growing prevalence of myopia over the decades and the higher risk of 6.5% for additional hours of near work. Although the children are not studying in the opposite shift, they are still using near vision for many hours. Hours of electronics use did not correlate with hyperopia or astigmatism.
Environmental risk factors are known to be important in myopia development. An important difference between the south and the equatorial region of Brazil is the level of insolation along the year. It is hot and sunny in the north and northeast for the entire year, while the south has four seasons. We found mean myopia was higher in the south compared to the equatorial Brazil (-2.73 D with cycloplegia in the south and -0.50 D with no cycloplegia in the northeast), although both are still low. The variation in weather and temperature, as much as better schooling and less severe poverty in the south, might explain the difference in myopia magnitude among these two regions.
Most school children had excellent uncorrected visual acuity. Students over 12 years old tended to have a higher prevalence of myopia and the incidence of pre-myopia was higher before reaching 12 years old. It seems that children in Brazil start to develop myopia older than Asians. The main possible bias of this study is the non-randomly selected sample. However, no children had previously had a vision screening and the eye exam was comprehensive, with cycloplegic refraction, making the evaluation reliable. National estimates are needed to detect the prevalence of myopia in the entire country in the same period and based on the same methodology. Public health initiatives that aim to prevent myopia from increasing further are needed to address the increasing prevalence of myopia in Brazil and its potential impact on future vision impairment.
The authors acknowledge hospital de Clinicas Central Administration and Outpatient Coordination, the employees and staff members of ophthalmology of Hospital de Clinicas de Porto Alegre, the financial support of Financiamento e Incentivo a Pesquisa (FIP)/Hospital de Clinicas de Porto Alegre (HCPA) , the Biostatistics of Grupo de Pesquisa e Pos-Graduacao (GPPG) HCPA, the medical students, residents and fellows of Ophthalmology from all facilities, the public ministry of Porto Alegre and Viamao, Sorigs (Sociedade de Oftalmologia do Rio Grande do Sul(SORGS)) and the International Myopia Institute(IMC). Their support was essential for collecting data during the coronavirus pandemic and for helping to disseminate Brazilian myopia prevalence to the world in the International Myopia Conference 2022.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Gus PI, de Maman RS, Lengler AD, Marinho D, Tartarella MB, Pakter H, et al (2024) Prevalence of Refractive Errors under Cycloplegia and Associated Factors with Focus on the Myopia Epidemic among Public School Children from Southern Brazil. J Clin Exp Ophthalmol. 15:976.
Received: 29-Apr-2024, Manuscript No. JCEO-24-30125; Editor assigned: 01-May-2024, Pre QC No. JCEO-24-30125 (PQ); Reviewed: 15-May-2024, QC No. JCEO-24-30125; Revised: 22-May-2024, Manuscript No. JCEO-24-30125 (R); Published: 30-May-2024 , DOI: 10.35248/2155-9570.24.15.976
Copyright: © 2024 Gus PI, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.