Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Research Article - (2022)Volume 13, Issue 1
Purpose: To describe the squamous cell carcinoma in the orbit as a primary site through systematic review and case report.
Method: A Systematic review of the literature was performed to focus on all the cases of primary squamous cell carcinoma that involves the orbit and exclude the cases that affect the ocular surface area and eye lid.
Results: Primary Squamous Cell Carcinoma (PSCC) in the orbit is extremely rare. Only 10 cases are reported in the literature including 2 atypical cases involved the orbit after retinal surgery. PSCC in the orbit are presented by vague symptoms such as headaches, fascial pain, numbness, and diplopia. Also, no standard accepted treatment exists. PSCC in the orbit can involve any tissue included the extraocular muscle, the lacrimal gland and indistinct area in the orbit.
Conclusion: Primary SCC at orbital site is very rare as only 10 cases are reported after systematic review of literatures and the common is secondary SCC through perineural invasion from a cutaneous lesion.
Squamous cell carcinoma; Orbit; Orbital tumour; Primary; Lacrimal gland; Periorbital
Myopia Squamous Cell Carcinoma (SCC) is an invasive epithelial malignancy showing keratinocytic differentiation in the ocular and periocular region; it can affect the conjunctiva, cornea, and eyelid skin. It is a rare disease in the conjunctiva with an incidence of 0.13 to 1.9 per 100,000 inhabitants, mainly affecting individuals between 50 and 75 years of age [1]. While the incidence of eyelid SCC has been reported to be between 0.09 and 2.42 cases per 100,000 population [2]. Squamous Cell Carcinoma (SCC) of the orbit is almost uniformly the result of local invasion from a cutaneous primary extension by perineural invasion, or the result of metastasis; in our knowledge of histopathology, no squamous epithelial cells in the orbit so primary squamous cell carcinoma in the orbit is very rare. This highlights the rareness of primary squamous cell carcinoma in orbital site cases.
Systematic reviews and meta-analysis guidelines were followed and the research on PubMed, MEDLINE and Web of science were conducted for all the articles that published from September 1991, the year of the first article had talked about the squamous cell carcinoma in the orbit, to the last article published in January 2021.The research “squamous cell carcinoma” combined with following terms “orbit”, “orbital”, “lacrimal gland”, “periorbital”, “adnexal”, “conjunctiva”, “eyelid” and “ocular surface area”. All articles and their references are viewed and analyzed. The case studies and reports that documented squamous cell carcinoma in the orbit as a primary lesion are included. Secondary squamous cell carcinoma, conjunctiva, ocular surface, and eyelid squamous cell carcinoma are excluded from the analysis after a complete review. The articles with inclusion criteria were reviewed and analyzed for: publication year, age, sex, laterality, presentation, signs, orbital location, systemic disorder, treatment, and outcome. Ethical Conduct for Research Involving Humans. Research adhered to the tenents of the Declaration of Helsinki as amended in 2008. Institutional Review Board approval was not required for the case report as per the Tri-Council Policy Statement.
A 99-years old, Egyptian female patient, presented with an enormous left eyelid mass extended with hall upper and lower lid, of 2 years duration and complained of severe headache, frontal numbness, and loss of vision. The history was recorded as the patient and her relevant stated that the lesion began with puffiness in the lateral site of eyelid with early proptotic eye since two years, but the patient refused to do any investigation and neglected the symptoms of 2 years until the numbness and the headaches increased and the giant mass appeared so the surrounding people started to be worried. On examination, A giant mass in the left upper lid extended to lower lid, with skin eruption, vesicle and over stretched on the mass, the eye globe can’t be assist, complete loss of vision and also the ocular motility was lost completely (Figure 1). On investigation, the CT orbit performed and shows that the mass from lacrimal gland extended to all orbital cavities, pushing the eyeball down and invading it. Also the mass extended to the whole upper and lower eyelids (Figure 2). Further investigations such as MRI scan were difficult to carry as the general condition of patient did not help. Our strategy to manage this patient was to do excision biopsy with preserving the eye globe if is it healthy. The patient and her relevant consent were taken to perform the surgery. During the surgery, skin incision at site of anatomical skin crease was firstly performed then dissection of the mass until the eye globe was reached. However, we found that the eye globe was completely invaded, and the extraocular muscle was difficult to distinguish from the invading tissue so the decision of complete orbital exenteration was decided. The large part of skin was excised as well as a complete removal of orbital tissue, periosteum, eye globe and extraocular muscle. The orbit irrigated with broad spectrum antibiotic after fine cautery and followed by closure of the upper and lower skin, total tarsorrhaphy, completely (Figure 3). Postoperative, systemic antibiotic and topical ointment dressed the wound. Unfortunately, the patient cut the sutures and opened the eyelid after 3 weeks due to her age which was not helpful; however the orbit was clear so the artificial prosthesis can be done (Figure 4). On histopathology, ulcerated epidermal covering overlying infiltrating tumor tissue formed groups of moderately pleomorphic malignant squamous cells grade II. There is a focal necrosis. The tumor infiltrating the eye globe and surrounding orbital tissue. The patient was referred to the oncology department, full-body PET-CT surveillance was performed, and detected that no lymph node involvement or evidence of any metastasis in the body and the oncologist decided that there is no need to perform systemic chemotherapy or radiotherapy. 6 months have passed since the original diagnosis and the patient is in good health.

Figure 1: Left orbital giant mass.
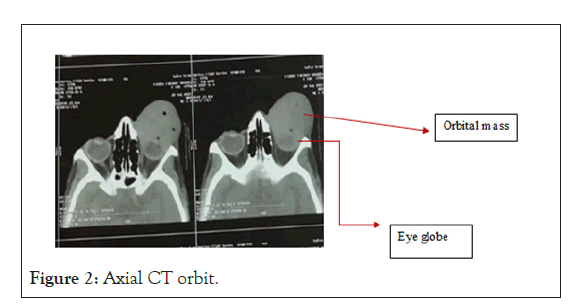
Figure 2: Axial CT orbit.

Figure 3: At the end of orbital exenteration, total tarsorrhaphy.
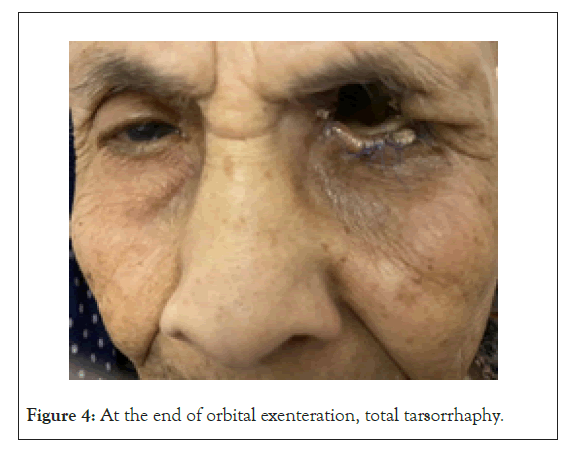
Figure 4: At the end of orbital exenteration, total tarsorrhaphy.
Systematic reviews and meta-analysis on PubMed, MEDLINE, and Web of Science databases, with reference searching and google scholar, were performed and 479 non-duplicate results of which 10 articles were included representing 10 patients (Figure 5).
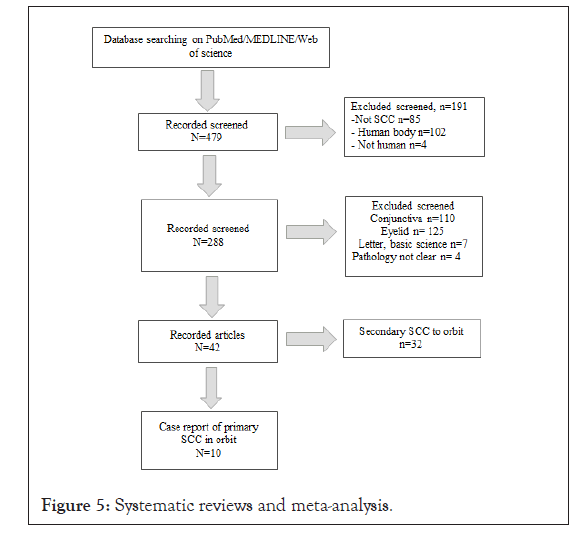
Figure 5: Systematic reviews and meta-analysis.
Both primary and secondary Squamous Cell Carcinoma (SCC) of the orbit are rare entities, though cystic SCC is even more, so it may provide a significant diagnostic conundrum to oculoplastic surgeons [3].The systematic review in the literatures detect that only 10 cases were reported with primary SCC in orbital site [4-7] but only 2 reported cases were non-apical primary SCC in the orbit [8,9]; it occurs after retinal surgery with proposed transplanted conjunctival epithelium and subsequent malignant transformation of a conjunctival cyst [10]. All special manifestation about all the reported cases is mentioned in Table 1. The symptoms of numbness, intermittent pain, puffiness of lid and mass in the orbit increase in size within 1-2 years duration are similar to our reported case, the only differences are in the size of mass and eye globe symptoms as in our reported case the huge size is very characteristic to a degree that covers completely the eye globe and obscured the all-eye globe signs. The occult cutaneous lesion that producing perineural invasion and so secondary SCC in the orbit are excluded by history as no right facial lesions and none were seen on examination also by dermatology records, dermatopathology reports and with the histopathology of tumor reported no neural invasion. All cases reported were between the age of 50-78 years old while the patient in our study is 99 years old which is not common nowadays so it may increase the incidence of the unusual cancer [11].
| Author/Year | Age | Sex | Characteristic symptoms | Investigation | Site of lesion | Management |
|---|---|---|---|---|---|---|
| Ruff et al. 1985 | 53 | F | Left fascial pain | CT face | Inferotemporal orbit | Gallium scan, orbital radiation |
| Saha et al. 2011 | 56 | F | Right forehead, cheek numbness, diplopia, right eye pain, blurry vision |
MRI brain, orbit sinus (Initially negative), repeat MRI orbit a year later |
Orbital apex | Primary orbital radiation therapy |
| Peckinpaugh 2012 | 43 | F | A common symptom: Diplopia | Full-body CT/PET scan | Orbital apex | Orbital radiotherapy, adjuvant chemotherapy |
| 63 | M | Ophthalmoplegia Forehead numbness |
||||
| 67 | M | |||||
| Hromas and Sokol, 2014 | 43 | M | Left decrease vision limited ocular motility |
MRI orbital, lateral orbitotomy with excisional biopsy Full body CT/PET scan |
Inferior interconal space between inferior rectus and optic nerve | Left orbital exenteration adjuvant orbital radiation |
| Choi et al. 2014 | 74 | F | Left upper eyelid swelling, eye pain, double vision, left forehead, cheek numbness |
MRI orbit | Superomedial obit | Left orbital exenteration adjuvant orbital radiation |
| Arbulu et al. 2017 | 73 | F | Headache, right periorbital pain, parenthesis, right ptosis, diplopia |
CT orbit MRI orbit Incisional biopsy Full body CT/PET scan |
Superior orbit abutting | Craniofacial resection with orbital exenteration with adjuvant orbital radiation |
| Blandford et al. 2018 | 63 | M | Right forehead, numbness, right ptosis, diplopia |
MRI brain MRI orbit Incisional biopsy Full body CT/PET |
Superomedial orbit | Right orbitotomy with excisional biopsy adjuvant chemotherapy Orbital radiation |
| Zho et al. 2021 | 78 | F | Right painless mass, Puffiness eye lid |
CT orbit | Superolateral orbit | Removal of lacrimal gland bloc with adjuvant orbital radiation |
| Elsamkary 2022 (our study) |
99 | F | Left puffiness eyelid, giant lid mass, facial numbness |
CT orbit/PET scan | Superolateral orbit | Left orbital exenteration |
Table 1: Literature data collection for case study. Literature data collection for case study.
As the primary SCC in site the orbit is extremely rare, the ideal strategy for the management were unclear, in the reported cases, the treatment ranged from primary orbital radiation and observation to orbital exenteration with adjuvant chemotherapy and orbital radiation. The incision biopsy of tissue with frozen section is performed if SCC is detected and then the decision of complete excision even exenteration with adjuvant chemo- radiation therapy after taking the consent of the patient and explaining the condition to the patient and his relevant is the ideal strategy. So in our case, the decision of complete excision with exenteration after explaining the condition and taking consent from the patient and her relevant for performing the surgery with photographic and video recording the operation.
The drawback, in our case that the general condition of the patient didn’t help to perform an MRI investigation preoperative, as done in other reports where repeated radiological MRI were carried to help in following up the lesion, and to explain the radiological appearance of the lesion.
Our case may aid to the idea of how to deal with a very rare presentation of an enormous primary SCC in site the orbit with this age group and focused on systemic review about such cases. Primary SCC at orbital site is very rare as only 10 cases are reported after systematic review of literatures and the common is secondary SCC through perineural invasion from a cutaneous lesion.
Patient consent
The patient(s) described herein consented to publication of the case in writing.
Disclosure statement
None of the authors have a proprietary interest in this study or any conflicts of interest to disclose and our study aren’t supported by any source of funding.
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
Citation: El Samkary M, Eliwa T, El Sherif R (2022) Primary Squamous Cell Carcinoma, Orbital Site: A Case Study and Systematic Review. J Clin Exp Ophthalmol. 13:905
Received: 10-Jan-2021, Manuscript No. JCEO-21-14919; Editor assigned: 13-Dec-2021, Pre QC No. JCEO-21-14919 (PQ); Reviewed: 27-Dec-2021, QC No. JCEO-21-14919; Revised: 03-Jan-2022, Manuscript No. JCEO-21-14919 (R); Published: 10-Jan-2022 , DOI: 10.35248/2155-9570.22.13.905
Copyright: © 2022 El Samkary M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.