Pediatrics & Therapeutics
Open Access
ISSN: 2161-0665
ISSN: 2161-0665
Case Report - (2024)Volume 14, Issue 3
Hyper IgE syndrome is a rare primary immunodeficiency disorder characterized by cold staphylococcal abscesses, recurrent respiratory infections, skeletal and coarse facial features and dentition abnormalities associated with high serum IgE levels. However, some cases remain asymptomatic or present with few or atypical manifestations of the disease. This is a report of a 14-year-old boy presented with delayed teeth eruption and coarse facies in addition to several asthma attacks. Further investigations revealed elevated serum IgE levels. Hyper IgE syndrome was considered due to recurrent sinus infections and retention of his primary teeth which was later confirmed by mutation analysis.
Hyper-IgE syndrome; STAT3; Primary teeth retention; Medicine
Hyper IgE syndromes are a group of primary immunodeficiency disorders which are characterized by refractory eczema, recurrent respiratory tract infections, cold abscesses, skeletal and coarse facial features and primary teeth retention in addition to elevated levels of serum IgE [1]. Mutations in STAT3 and DOCK8 are responsible for autosomal dominant and recessive forms of the disease respectively.
Here, we report a sporadic case of Hyper IgE, with few atypical manifestations of the disease including refractory sinusitis, and primary teeth retention without pulmonary infections which required a high index of suspicion for diagnosis [2]. The association of dermatitis beginning early in life, positive skin prick test, recurrent asthma exacerbations and anaphylaxis were confounding manifestations leading the diagnosis toward atopy.
A 14-year-old boy was referred to allergy and immunodeficiency clinic due to recurrent episodes of acute asthma attacks and a previous history of eczema. He was the third child of nonrelative parents. His problems began at the age of ten days when he developed acute erythematous papules associated with excoriations and vesicles over the glans skin following his circumcision procedure. Shortly thereafter, facial dermatitis appeared and continued to involve other parts of his body until he became 6 months of age. At this age a skin prick test was performed for him which was indicative of sensitivity reactions to milk, egg and wheat [3]. Therefore, an elimination diet including milk, egg and wheat was recommended and started for him. Beginning at the age of 18 months, he had two episodes of cough, dyspnea and wheezing, resembling asthma attacks which were followed by more exacerbations at older ages. These exacerbations were all successfully controlled with inhaled corticosteroids. At the age of 12 years, the patient experienced an episode of anaphylaxis. He also had recurrent episodes of sinusitis. Growth and development were normal at the age of 14 except for the retention of his primary teeth which was significantly unusual for this age (Figure 1). Based on these findings, an underlying immunodeficiency disorder was considered [4,5]. Laboratory workup showed a normal blood count (WBC: 7100 (poly-75%, lymph-24%), Hb: 15 mg/dl, Plt: 280000/mm3), normal IgA (57 mg/dl), normal IgM (48 mg/dl) and normal IgG (889 mg/dl). Serum IgE level was markedly elevated (1320 IU/ml) which in association with his previous history raised the possibility of hyper IgE syndrome. Genetic study (performed by the Centre of Chronic Immunodeficiency (CCI) laboratory, Germany) demonstrated heterozygous mutation in STAT3 with a nucleotide exchange of 1909G>A in exon 21 of STAT3 leading to an amino acid change (V637M) known as the cause of autosomal dominant type of HIES [6,7].
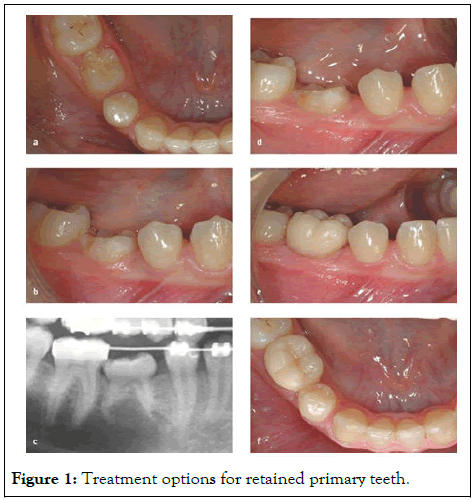
Figure 1: Treatment options for retained primary teeth.
The hyper IgE syndromes are a category of primary immunodeficiency disorders. The initial presentation is often a newborn rash which may progress to an eczematoid dermatitis [8]. Refractory eczema may resemble atopic dermatitis although with an atypical distribution [9]. The inheritance of the disorder is in autosomal dominant, autosomal recessive or sporadic manners Signal Transducer and Activator of Transcription 3 (STAT 3) signaling, Dedicator of Cytokinesis 8 (DOCK 8) signaling and Tyrosine Kinase 2 (TYK2) signaling alterations are known as responsible mutations for 3 forms of HIES, leading to the effect on TH17 cell and neutrophil responses. Recently Grimbacher, et al. found a novel hypomorphic homozygous mutation in Phosphoglumutase 3 (PGM3) in two families with hyper IgE syndrome phenotype associated with developmental delay and psychomotor retardation but without previous known mutations including STAT3 and DOCK8 [10].
Autosomal dominant HIES is mainly due to STAT3 mutations that impairs the development of IL-17 producing TH17 effector T-cells. STAT3 participates in transmission of intracellular signals with implications for fetal development, cancer, wound healing, angiogenesis and immunity. Many cytokines including IL-6, IL-10, IL-21, IL-22 and IL-23 signal through STAT3.
Abnormalities in the dentition are frequently seen in AD-HIES although with an unknown underlying mechanism [7]. Among the above mentioned cytokines which their signaling pathways is mediated via STAT3, IL-6 has definitive roles in bone hemostasis. Thus impaired STAT signaling may result in increased bone resorption by osteoclasts. This enhanced osteoclastogenesis may induce osteoporosis and decreased bone volume which may explain the retention of primary teeth in HIES. Grimbacher et al evaluated 30 patients with HIES and 70 of their relatives and reported primary teeth retention in 72% of them. Sinopulmonary infections occur frequently in these patients. Our patient had recurrent sinus infections but the atypical aspect of our patient’s history was that he had never experienced a pneumonia before.
Asthma was also another atypical presentation in this patient because according to literature allergic manifestations including allergic rhinitis, asthma, urticaria and anaphylaxis are not common clinical features in these patients despite their high serum IgE concentrations. Positive findings regarding an allergic background in this patient including neonatal dermatitis with positive skin prick test to milk, egg and wheat and a favorable response to an elimination diet including these three food allergens, recurrent asthma exacerbations and a history of anaphylaxis may denote an underlying atopic predisposition.
To conclude, the diagnosis of primary immunodeficiency entails combining the observed clinical phenotype with immunological and genetic analyses. This combination of clinical and basic scientific approach is now a prerequisite for gaining new insights into immunological mechanism and therefore provide information for better diagnosis and management of these rare disorders. Keeping in mind that a high index of suspicion has a key role in this regard and it is considered as the initial step for further evaluations.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Darougar S, Ramezanali A, Gharagozlou M, Chavoshzadeh Z, Arani MH (2024) Primary Teeth Retention as the Sole Presentation of Hyper IgE Syndrome: A Case Report. Pediatr Ther. 14:557.
Received: 08-Jun-2020, Manuscript No. PTCR-24-4854; Editor assigned: 11-Jun-2020, Pre QC No. PTCR-24-4854 (PQ); Reviewed: 25-Jun-2020, QC No. PTCR-24-4854; Revised: 15-May-2024, Manuscript No. PTCR-24-4854 (R); Published: 12-Jun-2024 , DOI: 10.35841/2161-0665.24.14.560
Copyright: © 2024 Darougar S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.