Pediatrics & Therapeutics
Open Access
ISSN: 2161-0665
ISSN: 2161-0665
Research Article - (2021)Volume 11, Issue 9
Background: Preterm related complication is a critical neonatal problem in the world causes death of nearly one million neonates per each year. In Ethiopia, it is still the first leading causes of neonatal mortality accounts 37% from the total neonatal death. Identifying factors associated with preterm mortality by conducting a research is one of the mechanisms used to tackle such kinds of critical public health problems. Hence, this study aimed to assess the mortality and its associated factors among preterm neonates admitted to neonatal intensive care units of Addis Ababa public hospitals, 2021. Methods and materials: An institutional based prospective follow up study was conducted among 358 preterm neonates admitted to selected public hospitals of Addis Ababa, Ethiopia from February 12 to May 12, 2021. Systematic random sampling was used to recruit each sample and data was collected prospectively using structured questioner. Bivariable and multivariable logistic regression were computed. Variables having P-value<0.05 in bivariable logistic regression were taken to multivariable logistic regression model to adjust for possible confounders. Variables with P<0.05 (CI: 95%) in multivariable logistic regression were declared as significant factors. Result: At the end of the cohort the proportion of preterm mortality was (34.9%). Thrombocytopenia (AHR: 0.26, CI' 0.68, 0.95), dehydration (AHR: 6.00, CI: 2.1, 20.0), hospital acquired infection (AHR: 5.6, CI: 1.6, 20.8) and CPAP type (AHR: 4.0, CI: 1.5, 10.5) were statistically significant factors having P<0.05. Conclusion: In this study, the proportion of preterm mortality was high. Thrombocytopenia, dehydration, hospital acquired infection and being kept on homemade CPAP type were the associated factors for preterm death.
Proportion; Preterm; Mortality; Associated factors; Addis ababa
Preterm neonates are especial group of population born before 37 completed weeks’ (259th day) of gestation [1-3]. Preterm neonates can be sub classified as extremely preterm (less than 28 weeks), very preterm (28-32 weeks), moderate preterm (32- 33 weeks and 6 days) and late preterm (34-36 weeks and 6 days) [4]. Preterm neonates can have normal birth weight (2500-3999 gram), low birth weight (1500-2499 gram), extremely low birth weight (1000-1499 gram) and extremely very low birth weight (less than 1000 gram) [5]. Preterm neonates are risk of death and long term morbidity not only from direct complications of prematurity, such as respiratory and nutrition complications but also infections [6]. Compared to term neonates, preterm neonates have much greater risk of death and disability to immature organ system which makes them unable to tolerate the extra uterine environment [7].
Globally, 15 million babies are expected to be born preterm which is more than 1 in 10 live births and from these, approximately 1 million children die each year due to preterm complications. The first 28 days of age is the hazard time in which 909,000 preterm neonates are died in each year and more than 100,000 preterm died after neonatal period, often after long hospital stays [6]. Even if preterm related complication is a public health problem throughout the globe, the severity is worse in developing countries in which 60% of the death is from Sub-Saharan Africa and south Asia [8]. They should survive as long as careful attention is given to feeding, warmth, and early treatment of problems, including breathing problems, infections, and jaundice – all feasible in low resource settings without high tech care [9]. In low-income settings, half of the babies born at or below 32 weeks (2 months early) die due to a lack of feasible, cost-effective care, such as warmth, breastfeeding support, and basic care for infections and breathing difficulties [6].
With effective implementation of World Health Organization (WHO) also sets ten recommendations to improve survival of preterm babies, which are antenatal corticosteroids, tocolysis, magnesium sulfate, antibiotic prophylaxis, mode of preterm birth (to mother) and neonatal kangaroo mother care, plastic wraps, continuous positive airway pressure therapy, surfactant and oxygen therapy three fourth of the babies could be saved [10]. Research are also ongoing to improve and scale up interventions like antenatal corticosteroids for early and late preterm birth, Kangaroo Mother Care (KMC) including KMC initiated soon after birth even for unstable babies and community-initiated KMC for bigger, stable babies, continuous positive airway pressure (CPAP), and low-cost and easy to use lung surfactant in low and middle income countries [6].
Even though lots are being done, preterm related complications are the leading cause of neonatal mortality in the world, its impact is severe in developing countries like Ethiopia causing 37% of total neonatal death [11]. Different studies abroad the globe in different times reported the magnitude of preterm mortality as 31.6% Tertiary Hospital in Western Uganda [12], (30.9%) in Ethiopia [13], 29.7% in TASH Ethiopia [14].
Although the causes of preterm mortality is multifactorial, available studies have identified different associated factors like, GA<32 weeks, birth weight<1000 g, birth defects, respiratory distress syndrome, necrotizing enterocolitis [15], maternal age ≥ 35 years, no antenatal care, singleton pregnancy,<28 weeks’ gestation, respiratory distress syndrome, apnea, hypothermia and small for gestational age [12], low gestational age, low birth weight, being female, feeding problem, no antenatal care visits.
In spite of all international, national and scientific efforts to decrease preterm mortality, the recent neonatal mortality report in Ethiopia (33 deaths per 1, 000 live births) reflects a worsening situation of the problem compared to the EDHS 2016 report (29 deaths per 1, 000 live births). From this preterm related complication is still the leading causes which should be reinvestigated. Therefore, this study aimed to determine preterm mortality and its associated factors among preterm neonates admitted to neonatal intensive care unit of Addis Ababa public hospitals.
Study area, design and study period
The study was conducted in Addis Ababa, the capital and largest city of Ethiopia. It is located on a well-watered plateau surrounded by hills and mountains, in the geographic center of the country with a total population of 4.8 million people. It is the political capital of Africa, where the African Union is headquartered and based. It is also the sit for the United Nations Economic Commission of Africa. The city has 12 public hospitals among these, six hospitals Gandhi memorial hospital (GMH), Yekatit 12 hospital medical college (Y12HMC), Zewditu memorial hospital, Ras-Desta Damtew memorial hospital (RDDMH), Menillik II referral hospital, Tirunesh Beijing general hospital) are governed by Addis Ababa health bureau and the rest five (St’ peter Specialized hospital (SPSH), St’ Paul’s Hospital millennium medical college hospital, Amanuel hospital, Alert hospital and Eka Kotebe hospital are governed by federal ministry of health and one university hospital (Tikur Anbessa Specialized Hospital (TASH). All of these hospitals except Amanuel hospital have their own neonatal intensive care unit. So, the study was conducted in five randomly selected public hospitals of Addis Ababa. These are TASH, GMH, RDDMH, Y12HMC and SPSH.
An institutional based prospective cohort follow up study was conducted from February 12-May 12, 2021.
Population
All preterm neonates admitted to neonatal intensive care unit (NICU) in selected public hospitals of Addis Ababa are sources of population and all preterm neonates admitted to NICU of selected public hospitals in Addis Ababa in the study period (from Feb 12 to May 12, 2021) were study population.
Inclusion and exclusion criteria
All alive neonates admitted to NICU by the diagnosis of preterm in selected public hospital with in the study period were included whereas preterm neonates diagnosed with major congenital anomaly (neural tube defect, congenital cardiac disease, gastrointestinal or abdominal wall defect and syndromic babies) were excluded.
Sample size and sampling procedure
Sample size was calculated for both for the general and specific objectives. Based on this the maximum sample size including ten percent none response rate was 365 from the specific objectives computed by using factors from previous literatures. This sample size was proportionally distributed to the five randomly selected hospitals by using three-month average base line preterm admission data from patient registration log book. Based on the data GMH had 180, Y12HMC had 118, TASH had 130, RDDMH had 87, and SPSH had 45 average preterm admissions per three months. The total population was less than twice of the sample size with k value of 1.53. Therefore, by using systematic sampling technique, from each three consecutive preterm admissions that full fulfill the inclusion criteria, two participants were selected randomly by lottery method until the required sample size was achieved in each hospital. If the recruited sample index mother refuses to participate the next admission was recruited. By using proportional allocation formula 117, 85, 77, 57 and 29 preterm neonates were recruited from TASH, GMH, Y12HMC, RDDMH and SPSH.
Study variables
The outcome variable for this study was death coded as (death=1, and not died=0). Independent variables include: Maternal socio demographic related predictors; (residence, maternal age, educational status, marital status and occupation), maternal obstetrical and medical predictors; multiple pregnancies, preterm prolonged rupture of membrane (PPROM), mode of delivery, preeclampsia, abruption placenta, antenatal care (ANC) follow up, steroid administration, hypertension, DM, human immune virus/acquired disease syndrome (HIV/AIDS) and sepsis), Preterm demography related predictors (age at admission, sex, weight, gestational age and weight for gestational age), preterm admission diagnosis and new problem diagnosed in the follow up (APGAR score, diagnosis at admission, new medical between the follow up) and treatment and health service related predictors; (antibiotics, feeding, CPAP, CPAP type, kangaroo mother care (KMC), nurse to patient ratio and feeding).
Data collection tool and procedure
Data collection tool was adapted from different studies with some modification. Study participants were recruited at admission by the data collectors and followed during their stay in the facility, taking note of all significant clinical events until either they become survived or dead. Readmitted neonates were managed according to their previous participation status in the study. In each study site trained nurses collected the data and those data collectors were mentored by the supervisors. The principal investigator followed the data collection process. Maternal data were collected by using direct interview and medical chart review. Neonatal data were collected from medical record prospectively until the study participant was died or survived. The maximum time of follow up in the ward was 28 days from birth. To assure the quality of data, the data collection tool was evaluated by neonatologists and research experts, two days training was given to the data collectors and supervisors about general research protocols, pretest was done on 5% preterm neonates at Minillik II Memorial hospital for its applicability and appropriateness. Place of delivery and ways of survived type were added to the tool after pretest. Supervisors inspected all the activities of the data collectors and assessed data quality daily. Before the data entry, it was checked for completeness and consistency by the principal investigator.
Data analysis procedure
The collected data was cleaned and sorted using Epi-Data software version 4.6. Entered data was exported and analyzed using STATA version 16. Descriptive statistics like frequency, measure of central tendency and standard deviation was computed to describe the study variable in relation to the population. Hosmer and Leeshawn goodness of fit test and omnibus tests of model coefficients were done to test the fitness of the logistic regression in the final model, then it was found good (statistically insignificant value, P value>0.05). Bivariate and multivariable logistic regression carried out to see associations between dependent and independent variables. Those variables that have p<0.05 in bivariable logistic regression were taken to the multivariable logistic regression model to adjust for possible confounders. The strength of the association declared at p-values<0.05 with 95% CI.
Socio-demographic factors of the study participants with their index mothers
During the study period, there were a total of 593 preterm admission, of those 43 were excluded due to congenital anomaly. A total of 365 preterm neonates with their index mothers were involved initially but, 7 preterm neonates were diagnosed with the exclusion criteria after they had been recruited to the study. Response up to the end of the outcome was obtained from 358(98.1%) participants. From these preterm neonates, males were 190 (53.07%) and females were 168 (46.9%). The mean age of the mother was 27.4 ± 4.7 SD years. The maximum and minimum maternal ages found in this study were 18 and 40 respectively. In this study 89(24.8%) mothers had no formal learning, 90(25.1%) primary education, 31(8.7%) secondary education 79(22.1%) technical/vocational and 69(19.3%) higher educational level. Most 313(87.4) mothers are living in urban. More than half 221 (61.73%) of the neonates were admitted at the age of less than 24 hours and the rest 137 (38.27%) were admitted at the age of 24 and above. The smallest weight and the youngest gestational age recorded in this study were 600 gm and 27 weeks respectively (Table 1).
| Variables | Categories | Total | Status | |
|---|---|---|---|---|
| Number (%) | Died (%) | Survived (%) | ||
| Marital Status | Single | 23(6.4) | 10(8) | 13(5.5) |
| Married | 330(92.2) | 112(89.6) | 218 (93.5) | |
| Divorced | 5(1.4) | 3(2.4) | 2(0.8) | |
| Governmental | 92(25.6) | 27(21.6) | 65(27.9) | |
| Private | 87(24.3) | 33(26.4) | 54(23.2) | |
| Occupation | Merchant | 32(8.9) | 12(9.6) | 20(8.5) |
| Farmer | 4(1.1) | 1(0.8) | 3(1.3) | |
| House wife | 113(31.6) | 42(33.6) | 71(30.5) | |
| Other | 30(8.4) | 10(8) | 20(8.6) | |
| Average household monthly income | Under extreme Poverty | 31(8.7) | 15(12) | 16(6.8) |
| Under poverty | 51(14.2) | 15(12) | 36(15.5) | |
| Above Poverty | 276(77.1) | 95((76) | 181(77.7) | |
| Birth Weight | EVBW | 15(41.8) | 13(10.4) | 2(0.9) |
| VLBW | 99(27.7) | 69(55.2) | 30(12.8) | |
| LBW | 211(58.9) | 41(32.2) | 170(73) | |
| NBW | 33(9.2) | 2(1.6) | 31(13.3) | |
| Gestational age | Extreme Preterm | 7(1.9) | 7(5.6) | 0(0) |
| Very Preterm | 109(30.5) | 79(63.2) | 30(12.9) | |
| Moderate Preterm | 59(16.5) | 19(15.2) | 40(17.2) | |
| Late preterm | 183(51.1) | 20(16) | 163(69.9) | |
Table 1: Socio-demographic related factors of preterm neonate and their index mothers among those admitted to neonatal intensive care unit of Addis Ababa public hospitals, Ethiopia, 2021. *Other: student, labor work
Maternal medical, pregnancy and obstetrics related predictors
Almost all 349 (97.5%) index mothers of this study had ANC follow up, of whom around three quarter 238(66.5%) of them had four or more antenatal visit whereas only 39(10.9%) of the mothers have less than four antenatal visits. Around quarters 100 (27.9%) of the mothers had multiple pregnancies, the rest 258(72.1%) had single pregnancy type. From the total index mothers, 144(40.2%) had took steroid of them 74(51.4%) got full doses. Almost all 349(97.5%) of the mother had delivered in health institution and only 9(2.5%) gave birth at home. Nearly half of 188(52.5%) the neonates were born via spontaneous vaginal delivery (SVD) and 161(45%) of them were via c-cesarian section (C/S), the rest 9(2.5%) were born instrumentally. Significant majority 316(88.3%) of the mothers had risk for preterm delivery. Around one-third 109(30.4%) of the mothers were preeclamptic and/or eclamptic, 22(6.2%) had oligo/polyhydramnios, 124(34.6%) PPROM and 32(8.9%) had antepartum hemorrhage (APH).
Neonatal admission diagnosis and new medical problem after developed between the follow up
Most 313(87.4%) neonates were appropriate for gestational age, only 42(11.7%) and 3(0.8) of preterm neonates were SGA and LGA respectively. In this study early onset neonatal sepsis (EONS) was found in significant majority of the neonates 309(86.8%) followed by RD 275(76.8%). More than half 192(53.6%) of the neonates were hypothermic at admission. In-between the follow up period, majority 277(77.4%) of the neonate’s had developed new medical problem during the follow up. Of those new medical problems observed during the follow up, 170(47.5%) of the neonates developed hyperbilirubinemia, 98(27.3%) preterm develop hospital acquired infection (HAI), 87(24.3%) develop necrotizing enterocolitis (NEC), 120(33.5%) develop apnea, 136(38%) develop thrombocytopenia and 84(23.5%) were diagnosed for dehydration (DHN) (Table 2).
| Variables | Categories | Total (%) | Status | |
|---|---|---|---|---|
| Died (%) | Survived (%) | |||
| 1st minute APGAR score | <3 | 20(5.6) | 13(10.6) | 7(3.1) |
| 03 Jun | 142(40.2) | 59(47.9) | 83(35.9) | |
| >=7 | 192(54.2) | 51(41.5) | 141(61) | |
| <3 | 3(0.8) | 3(2.4) | 0(0) | |
| 5th minute APGAR score | 03-Jun | 59(16.7) | 29(23.6) | 30(12.9) |
| >=7 | 292(82.5) | 91(73.9) | 201(87.1) | |
| Hypothermia | Yes | 192(53.6) | 87(69.6) | 105 (45.1) |
| No | 166(46.4) | 38(30.4) | 128(54.9) | |
| RDS | Yes | 275(76.8) | 121(96.8) | 154(66.1) |
| No | 83(23.2) | 4(3.2) | 79(33.9) | |
| EONS | Yes | 309(86.3) | 116(95.1) | 190(81.5) |
| No | 49(13.7) | 6(4.9) | 43(18.5) | |
| NHB | Yes | 38(10.6) | 2(1.6) | 10(4.3) |
| No | 320(89.4) | 123(98.4) | 223(95.7) | |
| PNA | Yes | 80(22.3) | 52(41.6) | 28(12) |
| No | 278(77.7) | 73(58.4) | 205(88) | |
| HAI | Yes | 98(27.4) | 61(48.8) | 37(15.9) |
| No | 178(50) | 64(51.2) | 114(48.9) | |
| NEC | Yes | 87(24.3) | 65(52) | 22(9.5) |
| No | 189(52.8) | 60(48) | 129(55.4) | |
Table 2: Neonatal admission diagnosis and new medical problem developed between the follow up related factors among neonates admitted to neonatal intensive care unit of Addis Ababa public hospitals, Ethiopia, 2021
Treatment related factors of preterm mortality
More than half of neonates 233(65.1%) were cared by greater than 1 to 2 patient nurse ratio in their hospital stay. Among those preterm babies 232(64.8%) had received CPAP for respiratory support the rest 126(35.2) didn’t get CPAP. Initiation of CPAP in nearly half of the neonates 123(53%) was after admission and only 2(0.8%) of neonates had started CPAP in delivery room before transportation to NICU. The most widely used CPAP type in this study was homemade (homegrown) CPAP. Significant majority 337(94.1%) of preterm neonates had received antibiotics. Among neonates who didn’t start feeding within the first 24 hours of admission, 50 (87.7%) were died and only 7(12.3%) survived.
Overall mortality of preterm neonates
In this study a total of 358 preterm neonates were followed for up to 28 days of postnatal age starting from admission up to the occurrence of outcome. Among those preterm neonates followed during the study period 125(34.9%) were died (Figure 1). From these deaths, 7(5.6%) neonates were<28 weeks, 79(63.2%) were between 28-32 weeks, 19(15.2%) neonate were between 32-33+6 weeks and 20(16%) were 34-36+6 weeks of gestation. Regarding about birth weight with deaths, 13(10.4%) neonates were<1000 gm, 69(55.2%) neonates were 1001 gm-1499 gm, 41(32.8%) neonates were 1500 gm-2499 gm and only 2(1.6%) preterm neonates were ≥2500 gm weighted preterm neonates.
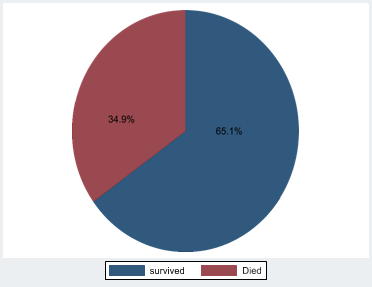
Figure 1: Over all out-come of preterm neonates admitted to neonatal intensive care unit of Addis Ababa public hospitals, 2021.
Most neonates 105 (84%) died in the first weeks of admission, 8 (6.4%) died before one days after admission, 48(38.4%) between one and three days from admission, above three days up to 7 days of admission 49 (39.2%) and the rest 20(16%) of the neonates died between 7 and 28 days of life (above seven days of admission). The minimum follows up times observed in this cohort was 2 hour and the maximum was 28 days. There were no survivors observed in the cohort of less than 28 weeks of gestational age and the survivors of those preterm neonates having less than 1000 gm were only two from a total of 15 preterm neonates. The immediate causes of death were, for 55(44%) of the preterm neonates was multiorgan failure secondary to overwhelming sepsis, 43(34.4%) respiratory failure secondary to respiratory distress, 18(14.4%) respiratory failure secondary to pulmonary hemorrhage and 9(7.2%) others (shock, sudden infant death).
Factors associated with preterm mortality
After bivariate logistic regression, variables having p-value less than 0.05 were transported to multivariable logistic regression which yields (Table 3). Based on this, thrombocytopenia (AHR: 0.26), dehydration (AHR: 6.00), hospital acquired infection (AHR: 5.6) and CPAP type (AHR: 4.0) were statistically significant associated factor with p value<0.05 for preterm death. This means that neonates with thrombocytopenia had 74% (CI: 0.68, 0.95) more likely to die compared with preterm neonates without thrombocytopenia. Preterm neonates diagnosed with dehydration during the follow up period had six times (CI: 2.1, 20.0) more risk of mortality compared with their counter parts. Similarly, preterm neonates developed hospital acquired infection had 5.6 times (CI: 1.6, 20.8) more risk of death than neonates without HAI. Preterm neonates who were kept on homegrown or home-made type of CPAP had 4 timees (CI: 1.5, 10.2) more risk of death compared to preterm treated with Dimedica CPAP type.
| Variables | Categories | Bi-variable result | Multi-variable result | Remark | ||
|---|---|---|---|---|---|---|
| P- value | CHR (95% CI) | P- value | AHR (95% CI) | |||
| Thrombocytopenia | Yes | 0.02 | 0.56(0.35,0.92) | 0 | 0.26(0.068,0.95) | *** |
| No | 1 | |||||
| Apnea | Yes | 0 | 17.5(9.6,31.9) | 0.1 | 7 (2.5,20.1) | |
| No | 1 | |||||
| Dehydration | Yes | 0 | 9.5(5.17.5) | 0 | 6(2.1, 20.0) | *** |
| No | 1 | |||||
| NEC | Yes | 0 | 6.4(3.6, 11.3) | 0.4 | 1.8(.51, 6.2) | |
| No | 1 | |||||
| HAI | Yes | 0 | 2.9(1.8, 4.9) | 0 | 5.6(1.6, 20.8) | *** |
| No | 1 | |||||
| Preeclampsia/eclampsia | Yes | 0 | 3(1.9, 5.00) | 0.5 | 1.4(.47, 4.4) | |
| No | 1 | |||||
| APH | Yes | 0.03 | 2.3(1.09, 4.83) | 0.1 | 4.3(0.70, 26.3) | |
| No | 1 | |||||
| CPAP type | Home made | 0.02 | 1.9(1.1, 3.13) | 0 | 4(1.5,10.2) | *** |
| Dimedica | 1 | |||||
| Hypothermia | Yes | 0 | 2.7(1.8, 4.4) | 0.4 | 1.7(.58, 4.7) | |
| No | 1 | |||||
| RD | Yes | 0 | 15(5.5, 43.5) | 0.6 | 1.8(.27, 11.5) | |
| No | 1 | |||||
| EONS | Yes | 0 | 4.5(1.9, 10.8) | 0.6 | 1.6(.3, 8.5) | |
| No | 1 | |||||
| PNA | Yes | 0 | 5.2(3.1, 8.9) | 0.1 | 3.3(.95, 11.5) | |
| No | 1 | |||||
| Birth Weight | <1000 | 0 | 100(12.8,79) | 0.1 | 71(1.15, 444) | |
| 1001-1499 | 0 | 35(8.0, 158) | 0.1 | 56(1.6, 191) | ||
| 1500-2499 | 0.08 | 3(.85, 16.3) | 0.1 | 14(0.44, 476) | ||
| >=2500 | 1 | |||||
| APH | Yes | 0.03 | 2.3(1.09,4.8) | 0.1 | 4.3(0.7,26.3) | |
| No | 1 | |||||
| Steroid administration Dose | One Dose | 0.13 | 2.2(0.79, 6.12) | 0.5 | 1.8(0.26,15.1) | |
| Two Dose | 0 | 4.6(1.80, 11.68) | 0.1 | 6.9(0.96, 43.7) | ||
| Three Dose | 0.75 | 1.2(0.423,3.29) | 0.2 | 0.24(.024, 2.32) | ||
Table 3: Multivariate cox proportional hazard regression result of preterm neonates admitted to neonatal intensive care unit of Addis Ababa public hospitals, Ethiopia, 2021. ***, statistically significant
Whereas variables NEC, Preeclampsia/eclampsia, APH, Hypothermia, RD, EONS, PNA, Birth, steroid administration dose, weight and APH were statistically insignificant in multivariable regression with p-value>0.05 (Table 3).
Preterm related complication remains the first leading causes of neonatal death. According to the 2019 Ethiopia Demographic and Health Survey, neonatal mortality was 33 per 1,000 live births. This study aimed to assess proportion of preterm death and its associated factors among preterm neonates admitted to neonatal intensive care unit of Addis Ababa public hospitals to tackle the problem of preterm health by including possible risk factors as abasement tool.
In this prospective cohort study, the proportion of mortality was 125(34.9%) with the incidence rate of 36.4/1000 neonateday observation. The proportion of mortality in this study was similar with the finding done in Jimma university specialized hospital and Bahr Dar university hospital 34.9% and 36.1%. The possible explanation of these similarities could be the study areas were referral hospitals in which high risk mothers can be referred from different parts of the country leads to high flow of preterm birth and intra-partum complication may leads to preterm death. It can be also explained similarity of NICU setups which haven’t different sophisticated materials used to save preterm neonates.
This finding was higher than the result of studies conducted in Western Uganda 31.6%, Dessie 30.9%, University of Gondor Hospital (28.8%), Debretabor General Hospital, Northwest Ethiopia 31.2% and TASH (29.7%). The possible reason for this difference might be due to the fact that this study was conducted in multicenter institution unlike other. Being used multicenter institution may elevate the proportion of death in which there might be difference in care, professional distribution and more high-risk mothers could be found from different parts of the areas possibly increase unfavorable outcome of preterm neonates. In addition, this study was conducted prospectively which didn’t miss any death due to chart incompleteness, usually encountered problem in retrospective studies.
Preterm neonates diagnosed with hospital acquired infection during their hospital stay had 5.6 times more risk to die compared to their counter parts. This finding was in agreement with the conclusion of a study conducted in Felege Hiwot specialized hospital, Bahir Dar, Ethiopia. The possible scientific justification for this could be in fact that preterm neonates are vulnerable since they often undergo invasive and repeatable procedures, and also are dependent on central catheters to deliver nutrition and on ventilators for respiratory support for prolonged time period. Each and every invasive procedure especially respiratory and intravenous related procedures had more risk of infection. Hospital acquired infection for preterm neonates could be danger due to less immune system to fight against microorganism unlike term neonates. Such reasoning may lead to preterm death. Similarly, the nature of microorganisms causing hospital acquired infection mostly resistant for broad-spectrum antibiotics difficult to treat easily might be another possible justification.
Regarding to thrombocytopenia, preterm neonates diagnosed with thrombocytopenia during their hospital stay had 74% more likely to die compared to neonates without thrombocytopenia. This finding was similar with the conclusion of a multicenter study conducted in United Kingdom, Netherlands, and Ireland and another multicenter study conducted in Dera Ghazi Khan and Nishtar Medical University. The possible scientific justification for this might be thrombocytopenia in preterm neonate is very common and is frequent due to prenatal complications (pregnancy induced hypertension, intrauterine growth restriction, placental insufficiency in which most are risk factors for preterm birth). Additionally, thrombocytopenia leads bleeding, hyperbilirubinemia, anemia, apnea, pulmonary hemorrhage, too much bleeding can be dangerous and can affect the brain and other body systems, this complication together or in single might causes preterm death.
Dehydration was another associated factor identified in this study which increases the risk of preterm death by six folds. This finding is supported by the scientific ground that preterm neonates are vulnerable for dehydration due to greater portion of their bodies is made of water, have high metabolic rate need more water, preterm neonates kidneys do not conserve water like term babies, preterm natural defense system that helps fight infection (immune system) is not fully developed, which increases the chance of getting illness, preterm neonates have immature skin resulting for evaporation through the immature epithelial layer and preterm are risk for neonatal hyperbilirubinemia which should be treated by phototherapy and phototherapy causing risk for dehydration. Another possible reason for these might be poor clinical practice of fluid monitoring system shown almost in all of the study areas leads to dehydration. Due to these risks, dehydration leads to organ failure ends up with preterm death or sever morbidity.
In the study areas of this cohort, two types of CPAP were utilized to treat respiratory distress. These CPAP types were Dimedica and Homemade/homegrown CPAP. Regarding that, being puton home-made CPAP type increases the risk of preterm death by four times compared to preterm neonates kept on Dimedica CPAP. This might be in fact that homemade types of CPAP can’t control the amount of Fio 2 delivered to the neonates which may over or under deliver compared to Dimedica CPAP type which has self-contained unit generates 95% oxygen and its own medical air, humidifier ensures appropriate warmth and moisture for the air and oxygen delivered to the patient and clear oxygen/air mixing chart allows for easy setting of flow rates. In fact, most participants of this study were treated by home grown/ homemade type of CPAP which could inflate the number. This might be another possible justification.
In conclusion, the proportion of preterm mortality found to be 34.9%. Thrombocytopenia dehydration, hospital acquired infection and kept on home-made CPAP type were statistically significant associated factors for preterm death. From this study we can conclude that preterm mortality was high which needs urgent intervention. Therefore, intervening on the identified associated factors of preterm mortality timely and appropriately could have significant advantages in the working process of improving preterm neonatal survival.
Ethical approval was obtained from Institutional Review Board (IRB) of AAU, college of health science. Permission was sought from each hospital. Written informed consent was obtained from each participants index mother or care givers. The privacy of the study participants and confidentiality of information was strictly maintained by omitting any personal identifier during the data collection.
The data and other documents used in this study are available from the corresponding author.
The authors declare that they have no conflict of interest.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
DB: conceptualization, methodology, data entry, data cleaning, data analysis, writing original draft, AS, YG and NM, validation, tool evaluation, methodology, reviewing and editing. Finally, all authors approved the manuscript.
We would like to acknowledge staff working in neonatal intensive care unit of TASH, SPSH, GMH, RDDMH and Y12HMC for their cooperativeness. Our heartfelt thanks also go to all the data collectors for their valuable contribution to the realization of this study. Last but not least we would like to say thank you for all study subjects together with their index mothers/care givers as this couldn’t happen without them.
Received: 27-Aug-2021 Accepted: 10-Sep-2021 Published: 17-Sep-2021 , DOI: 10.35248/2161-0665.21.11.397
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.