
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Research - (2023)Volume 14, Issue 2
Background: General anesthesia and sedation techniques with local anesthesia have been the choice in Major Ambulatory Surgery (MAS) compared to intrathecal techniques, which are used when complications of general anesthesia may be greater (difficult airway, Chronic Obstructive Pulmonary Disease (COPD) or risk of airborne infection). We currently use prilocaine, although its great individual variability can cause delays in patient discharge or unexpected admissions. Due to its more predictable pharmacokinetic profile and short duration of motor block, intrathecal 1% chloroprocaine could represent a useful tool in MAS.
Methods: 103 inguinal hernia surgery patients were randomly assigned into two groups, one receiving 50 mg of 1% intrathecal chloroprocaine and the other 50 mg of 2% hyperbaric prilocaine. The primary outcome was the percentage of patients who could start walking 2 hours after dural puncture. Secondary variables were: Percentage of patients with ambulation at 2.5 and 3 hours; delayed time to discharge; total length of stay in the MASU; unexpected admissions, complications in postoperative period, pain intensity at admission and discharge from the MASU; satisfaction with the technique used and outpatient care.
Results: 5 patients of the original 103 were excluded from the study, so 98 patients were included in the statistical analysis (prilocaine group n=44, chloroprocaine group n=54). There were no significant differences in anthropometric data nor in surgery duration time (26.99 ± 7.96 min, mean ± SD). Statistical analysis showed significant differences between the groups regarding the primary outcome. 48.1% of patients in the chloroprocaine group were ambulatory at 2 hours compared to 4.5% in the prilocaine group (p<0.0001). Moreover, significant differences were observed in the percentage of ambulation at 2.5 hours (75.9% vs. 13.6%) and at 3 hours (94.4% vs. 31.8%) in favour of the 1% chloroprocaine group (p<0.0001). We observed a longer delayed discharge time in the chloroprocaine group (108.8 ± 55.5min vs. 45.3 ± 72.8 min) (p<0.0001), meaning patients in the chloroprocaine group remained longer in the hospital once discharge criteria were met. However, no differences were observed in the total length of hospital stay, likely due to administrative management issues. No major complications were recorded.
Conclusion: Spinal anesthesia with 1% chloroprocaine was found to be a good alternative for outpatient inguinal hernia repair, due to the rapid recovery of motor block and onset of ambulation of patients compared to 2% hyperbaric prilocaine, especially in afternoon surgery. In addition, it offers advantages to patients with COPD, difficult airway, or less airway manipulation, as in COVID-19.
Spinal anesthesia; Chloroprocaine; Major ambulatory surgery; Post-anesthesia care unit
The Major Ambulatory Surgery Unit (MASU) is a multidisciplinary surgical care model that allows patients to be treated safely and effectively, without hospitalization. This is benefit to the patient, and the healthcare system. Advances in anesthetic techniques and less invasive surgical techniques have helped the development of Major Ambulatory Surgery (MAS). Spinal anesthesia is an alternative to general anesthesia in open inguinal hernia repair surgery [1-4].
This can provide advantages in certain cases such as patients with Chronic Obstructive Pulmonary Disease (COPD) or difficult airway and it reduces the risk of air bone infection in the operating room of infectious diseases transmitted by aerosols, as has occurred during the COVID-19 pandemic. However, this technique is not without its detractors in the field of outpatient surgery due to the time required for complete reversal of the motor blockade, which was increased with the use of traditional local anesthetics, as well as the occurrence of complications such as urinary retention [5]. These facts have improved with prilocaine and chloroprocaine, which have been recently reintroduced into clinical practice.
Inguinal hernia is a highly prevalent outpatient pathology, with a Replacement Rate (RR) greater than 80% [6,7]. Various anesthetic techniques can be used: General, loco regional and local anesthesia and sedation [8]. Thus, due to its prevalence it was the pathology chosen for our study. There are no any studies comparing both anesthetics in inguinal hernia surgery focused in differences on de-ambulation. Other procedures in which it has been used and comparing the use of chloroprocaine and prilocaine in spinal anesthesia for ambulatory surgery were perianal surgery [9] and knee arthroscopy [10-12].The results showed improved recovery from blockade, shorter time to discharge and greater efficiency of outpatient surgery with the use of chloroprocaine.
Our hyphothesis is that the use of chloroprocaine would result in a faster time to discharge compared to prilocaine because chloroprocaine has a faster de-ambulatory recovery time. The aim of this study whether there are differences between the percentage of patients who can de-ambulate at two, two hours and a half and three hours comparing chloroprocaine and prilocaine.
Two comparison groups were established. One group to be performed to spinal anesthesia with 1% chloroprocaine 50 mg (Braun medical, Germany) another comparison group to be subjected to loco regional anesthesia by intrathecal administration of 2% hyperbaric prilocaine hydrochloride 50 mg [6,13,14] (Braun medical, Germany). The study was approved by the Spanish Agency for Medicine and Medical Devices (AEMPS).
This manuscript adheres to the applicable CONSORT guidelines. The inclusion criteria were: 18 to 80 aged patients, ASA I-II, for outpatient inguinal hernia surgery who accepted their participation in the study and informed consent signed. Were excluded in the study if they had: Allergy to local anesthetics, there was absolute contraindication to spinal anesthesia or outpatient basis, and refusal to loco regional anesthesia.
Thus, patients who met the criteria were selected by the recruiter. A sample size with a minimum N of 90 patients was calculated according to the study objective described in the statistical study. Then patients were randomized according to their year of birth+medical record number (random hospital identification number, to mask group membership) by the coordinator: Patients identified with odd numbers were assigned to the prilocaine group, and patients with even numbers to the chloroprocaine group. The patients did not know to which group they belonged.
All patients were collected in the afternoon, according to the usual schedule at Hospital Arnau de Villanova ,Valencia, Spain. A 6-hour fasting period before anesthesia was established; clear liquids were allowed up to 2 hours before admission. After arrival at the MASU, it was verified that there were no contraindications for the anesthetic and surgical procedure. Peripheral venous catheterization (18-20G) was performed. Prior to anesthetic induction, patients were monitored by continuous electrocardiography, peripheral pulse oximetry and non-invasive blood pressure measurement at 5-minute intervals. Fluid perfusion was administered on average about 200 ml corresponding to antibiotic dilution and preoperative analgesia (1 g paracetamol/2 g metamizole+50 mg dexketoprofen). Midazolam 1-2 mg was administered as anxiolytic premedication.
Under strict aseptic conditions, a medial approach to the subarachnoid space was performed identifying the interspinous space from L3 to L4 while seated. After infiltration of subcutaneous cellular tissue with 2-3 ml of 2% lidocaine, the subarachnoid space was located with a 25-27 G Whitacre pencil needle. Continuous free flow of cerebrospinal fluid indicated the correct needle position and 50 mg of 1% chloroprocaine or 50 mg of 2% hyperbaric prilocaine was injected in the absence of paresthesia or blood reflux. Dose was determined according to the data sheet for T-10 sensorial blocking. In case of Chloroprocaine was 50 mg. In case of Prilocaine we have chosen the average dose provided by the technical data sheet for an approximated duration of 100-130 min and for it to be a balanced comparison.
The medication was provided in a sealed envelope after patient randomization had been performed and it was not reflected in the anesthetic report to maintain blindness in data collection. The exact time of puncture was specified so that data collection could be performed properly.
After the injection, patients were immediately placed in the supine position for surgery. Optionally, and at the patient's request due to their perioperative anxiety state, Intravenous (IV) propofol was infused until a level of mild sedation (-1 to 2 richmond sedation scale) was achieved. The minimum anesthesia level required to perform this type of procedure (T10) and motor and sensory blockade was checked as normal clinical practice (impossibility to move lower limbs and no pain to punction), recording any incidents related to the technique. If the necessary block was not achieved and the procedure required deep sedation or general anesthesia for pain patients were excluded from analysis.
As antiemetic prophylaxis, droperidol (0.0625 mg) and dexamethasone (4 mg) had been established for all patients [15,16]. However, due to stock out of droperidol it was changed to ondansetron 4 mg [17,18]. Before the end of surgery, the surgical wound was infiltrated as postoperative analgesic treatment with 20 ml of 0.25% levobupivacaine and 1 g of IV Paracetamol+IV Dexketoprofen 50 mg was administered to all patients, except those allergic to one of both, in which IV Metamizole 2 g was substituted.
After the surgery, all patients were transferred to the Post-Anesthesia Care Unit (PACU) [19-21]. A nurse/anesthetist outside the study different of the surgery room (for blinded data collection) recorded the time of lower limb mobilization (foot flexion-extension, Bromage scale grade 3) of the patients, at which point they were transferred to the MASU. There, 2 hours after the puncture (time recorded by the anesthesiologist who performed the technique in the data collection notebook), in accordance with the previously established discharge criteria [19-21], (patients can move both legs, Bromage scale grade 1) the patient was encouraged to ambulate aided by an MASU nurse help and to check if the patients can ambulate spontaneously, recording the cases in which it was possible (primary outcome), and if not, a new attempt was made every 30 minutes up until 3 hours (data recorded by an MASU nurse), (secondary outcomes).
We also recorded adverse effects (nausea/vomiting, hypotension, urinary retention, etc), post-operative pain and its intensity (Visual Analogue Scale (VAS): 0 for no pain, 10 for worst pain), whether analgesia was required and the administered medication, and the time of patient discharge from the MASU. Moreover, an optional survey was carried out to assess patient satisfaction with the anesthetic technique and the overall outpatient surgery process [22,23]. After discharge, no patient included in the study requested attention for pain, nausea, urinary retention or post dural puncture headache [24].
Statistical analysis
Sample size was calculated with EPIDAT v4.2 PROGRAM based on the primary, quantitative and binary qualitative outcome variable. We presumed that a difference of 18 min between the two groups would be clinically important. Assuming an SD of 30 min, α=0.05 and a power of 0.8, we obtained a total sample size of n=45 for each group. We were not able to account for possible exclusions for the rejection of the technique, malfunction of loco regional anesthesia in some patients and the need of conversion to general anesthesia. Moreover, as we could not ensure that the data would be normally distributed, we increased the estimated sample size by 10%, which is 113 patients in total distributed randomly in both groups. Statistical analysis was carried out by a member who was not involved in data collection using the SPSS statistical system. For qualitative data, absolute and relative frequencies are given. Normally distributed, quantitative data are presented as mean ± SD. Differences between the groups were analyzed using a Chi-squared test for qualitative data and a Student’s t-test for quantitative data (Kolmogorov-Smirnoff test was used to check for normality). P values less than 0.05 were considered as statistically significant.
After inclusion of 113 patients (from November 2020 to January 2022), statistical analysis of the data collected showed the results to be robust. Differences between both groups regarding the primary outcome (de-ambulation after 2 hours) and secondary outcomes (de-ambulation after 2.5 and 3 hours) were precise enough to demonstrate significance. As a result of the COVID-19 pandemic we decided to stop patient recruitment due to the difficulty of doing this kind of surgical procedures in our outpatient unit without increasing recruitment period. Of the 113 patients recruited, 10 refused loco regional anesthesia, so 103 were randomly allocated into two groups. However, in 5 cases there was a malfunction of loco regional anaesthesia (T-10 block was not achived, pain test positive), and it was necessary to perform a deep sedation or general anesthesia to complete the surgical procedure. This resulted in a total number of analyzed patients of 98 (Prilocaine=44, Chloroprocaine=54) (Figure 1).
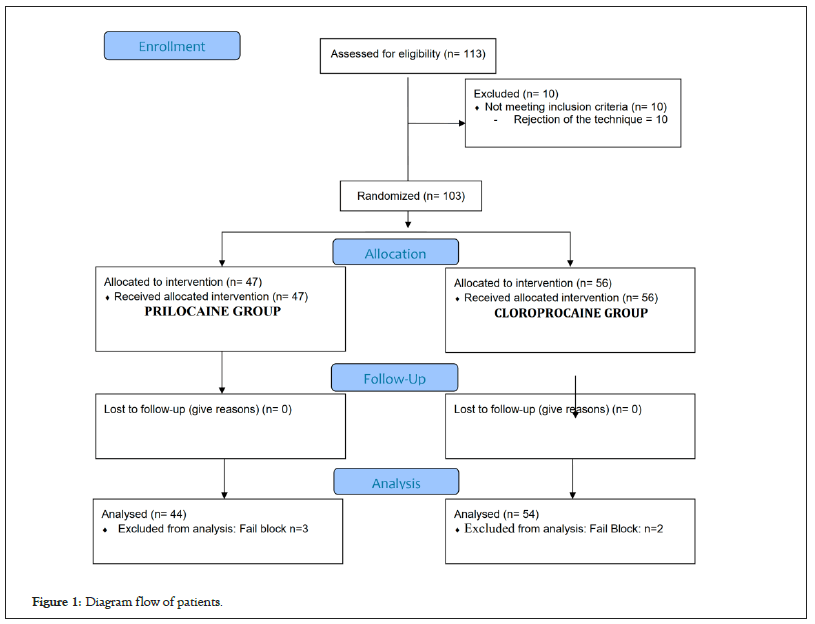
Figure 1: Diagram flow of patients.
There were no significant differences in personal data between the groups (Table 1). Surgery took place without any surgical complications, lasting between 18-35 minutes, (mean surgery duration 26.99 ± 7.96 min.) without significant differences (p=0.269) (Table 2).
| Characteristics | aLA (Prilocaine) | LA (Cloroprocaine) | p value |
|---|---|---|---|
| Sex (M/F) | 41/3 | 47/7 | 0.318 |
| Age (Years) | 57.93 ± 13.5 | 60.85 ± 13.4 | 0.288 |
| Body Weight (kg) | 74 ± 10.33 | 76.5 ± 12,92 | 0.3 |
| Body Height (cm) | 171.7 ± 7 | 170.8 ± 8.2 | 0.579 |
| ASA I/II | 24/20 | 21/33 | 0.122 |
Note: Quantitative data are given by mean ± SD or median (range) qualitative by frequencies, aLA ( Loco-regional Anesthesia).
Table 1: Personal data.
| Characteristics | aLA (Prilocaine) | LA (Cloroprocaine) | p Value | |
|---|---|---|---|---|
| Surgery time (min) | 26 ± 8.3 | 27.8 ± 7.6 | 0.269 | |
| De-ambulation 2 h | Yes/No(%) | 2(4.5%) /42(95.5%) | 26(48.1%) /28(51.9%) | 0.0001 |
| De-ambulation 2,5 h | Yes/No(%) | 6(13.6%)/38(86.5%) | 41(75.9%)/13 (24.1%) | 0.0001 |
| De-ambulation 3 h | Yes/No(%) | 14(31.8%)/30(68.2%) | 51(94.4%)/3 (5.6%) | 0.0001 |
| Fluid tolerance ( min ) | 25.2 ± 13.5 | 25 ± 15.3 | 0.958 | |
| Initiate dorsiflexion feet (min) | 82.5 ± 24.3 | 58.6 ± 19.2 | 0 | |
| Total Time in Hospital (min) | 308.2 ± 54.1 | 256.5 ± 43.7 | 0.123 | |
| Delayed to discharged (min) * | 45.3 ± 72.8 | 108.8 ± 55.5 | 0 | |
| Unexpected Admission No/Yes | 40/4 | 54/4 | 0.76 | |
| Admission to anesth technique | 40/4 | 54/0 | 0.732 | |
| Nausea and Vomiting | 0 | 0 | - | |
| Postpunction headache | 0 | 0 | - | |
| Urinary Retention | 0 | 0 | - | |
| Hyptension** | 0 | 1 | 0.134 | |
| Legs discomfort (***anxiety) | 4(1) | 0 | 0.864 | |
| Satisfaction LA: Bad-Regular-Well | 05-02-1931 | 01-06-1935 | 0.15 | |
| Satisfaction Circuit Yes/No | 31-May | 35/1 | 0.08 | |
Note: Quantitative data are given by mean ± SD or median (range), qualitative by frequencies. aLA (Loco regional Anesthesia). (*) Time calculated since patients are to be able to walk without help and leave Hospital. (**) Hypotension with Vasopressor drugs needed. (***) Anxiety generated for unknown legs position.
Table 2: Results: Recovery times, complications and satisfaction.
Regarding the primary outcome, time to ambulation was significantly shorter at 2 h, in the chloroprocaine group compared to the prilocaine group (p=0.0001) (Figures 2-4). Regarding the secondary outcome, time to ambulation was significantly shorter at 2.5 h, and 3 h (p=0.0001), and time to initiate foot dorsiflexion was shorter in the chloroprocaine group compared to the prilocaine group (58.6 min vs. 82.5 min, p=0.0002).
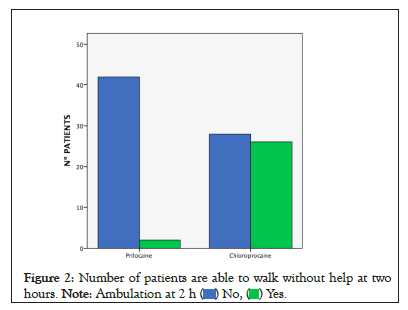
Figure 2: Number of patients are able to walk without help at two
hours. 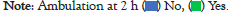
Figure 3: Number of patients are able to walk without help at two
hours and a half. 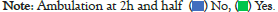
Figure 4: Number of patients are able to walk without help at three
hours. 
The postoperative patient analysis showed that none of the patients experienced postoperative nausea and vomiting. However, 8 patients were admitted to the hospital: 4 patients in the prilocaine group (due to insufficient time to restore anaesthesic blockade before closing of the MASU), and 4 patients in chloroprocaine group (1 due to social issues, as the patient was living alone, and 3 due to surgical complications). Pain scores were similar in both groups (p=0.564). No differences were observed in both groups in time to be discharged. Nevertheless, if we consider the time in which patients can walk spontaneously (without help) as the time at which the patient can be discharged, we observe an increased delay to discharge in the chloroprocaine group (108.8 vs. 45.3 min, p=0.0002). This is a variable that we have called delayed discharge time. This variable was calculated by determining the time the patient remained in the unit from the time they were able to ambulate until the time they left the hospital. The quality of recovery and Grade of Satisfaction of Outpatient Circuit (p=0.08) and Loco regional Anesthesia (p=0.150) was similar in both groups.
In order to improve patient discharge after MAS, it is essential to know the factors that influence the time elapsed between leaving the operating room and hospital discharge [1,2]. The use of an opiate-free anesthetic technique, especially in patients with pulmonary pathology [3], peripheral nerve plexus blocking techniques or neuroaxial blocking opioids free 3 could be very useful.
The intrathecal use of medium or long-acting local anesthetics generates an imbalance between the surgical time and the maintenance of motor and sensory blockade, frequently making their outpatient use impossible. This fact is partially improved with the introduction of prilocaine.
Prilocaine hydrochloride is an amide-type hyperbaric local anesthetic characterized by intermediate potency and duration. It was synthesized in 1953 and has been used in Europe since 2005. 2% hyperbaric prilocaine has a rapid onset of action and low incidence of transient neurological symptoms. Thus, it was presented as a viable alternative to lidocaine and mepivacaine for anesthesia of intermediate or short duration in ambulatory surgery. The mean time to discharge occurs in approximately 4 hours after spinal administration [16,22], but it presents a great interindividual variability, with some case of longer blockade (Fosters et al. 2011 and 2014) [25-26] causing unexpected admissions and doubts about its use in outpatient surgery (afternoon programs or last scheduled patients).
Chloroprocaine is an ester local anesthetic synthesized even earlier than prilocaine and used around 1950. It was discontinued in 1980 due to allergic reactions in patients with hypersensitivity to para-amino-benzoic acid (present in cosmetic products), and sodium bisulphite responsible for its increased neurotoxicity. However, an improved preservative-free formulation was introduced in 2006, which maintained its pharmacokinetic profile, a rapid onset of sensory and motor blockade similar to the amino-amide local anesthetics and a shorter time for reversal of its effects, but with a low rate of adverse effects [27].
1% Chloroprocaine could be an alternative to prilocaine, and a very useful tool as an alternative to general anesthesia [28-30], especially in patients with pulmonary disease, difficult airway or its predictive criteria. Moreover, there is a new advantage for loco regional anesthesia which was made evident during the COVID-19 pandemic: The reduced possibility of transmission between hospital staff and patients in the operating room when community transmission is possible. Patients can remain with their face mask on during the process, and no aerosols are generated since ventilation techniques are not required. Additionally, the use of intrathecal chloroprocaine as an anesthetic technique has a lower cost than general anesthesia [31].
In our hospital, hyperbaric prilocaine was already widely used in open inguinal hernia surgery and when chloroprocaine was introduced, the need arose to compare them.
Our main objective was to determine the percentage of patients who could ambulate 2 hours after lumbar puncture, so they could be discharged if the rest of the criteria for post anesthetic discharge scoring system (PADSS) [32] were met. In the case in which they could not ambulate we continued monitoring them at 2,5 and 3 h. We established these periods because they are the most useful in practice due to the operation of our unit, since the more patients are under care the more difficult it becomes to determine the exact moment of complete reversal of motor and sensory blockade. Comparing the results obtained from both groups (Table 2), a significant difference was established.
There are no any studies comparing both anesthetics in inguinal hernia surgery focused in differences on de-ambulation. Other procedures in which it has been used and comparing the use of chloroprocaine and prilocaine in spinal anesthesia for ambulatory surgery were perianal surgery [9] and knee arthroscopy [10] In anorectal surgery, prilocaine may be particularly useful because of its hyperbaricity [30]. Regarding knee arthroscopy we can find recent studies, such as those by Gebhardt and Wesselink (2019) [10,11], Gebhardt's study [32], and Guntz (2021) [12]. In these studies, the use of chloroprocaine showed improve recovery from the blockade and a shorter time to discharge, so the efficiency of outpatient surgery was greater.
However, despite we obtained in our results that more patients had an early de-ambulation, these differences did not have an impact on the total length of hospital stay (Table 2), Table 2 shows a variable that we have called delayed discharge time. This variable was calculated by determining the time the patient remained in the unit from the time they were able to ambulate until the time they left the hospital. In this case we did find significant differences between the groups, as there was a delay in discharge time of 108 ± 55.5 minutes for chloroprocaine and 45.3 ± 72.8 minutes for prilocaine. Thus, patients in the chloroprocaine group remained in the hospital longer once the discharge criteria had been met.
Regarding the possible causes of the hospital stay being the same in both groups, due to the way the unit operates, the patients in the afternoon session are admitted at similar times (between 14 h and 16 h in the afternoon) and all are discharged at the end of the surgical session. It is therefore an administrative issue that patients have a similar hospital stay regardless of when they meet discharge criteria. This data can help us adapt the operation of the MASU to increase its efficiency.
We did not find significant differences in unexpected admissions between the two groups (Table 2). However, when we analyze the causes of these admissions, we can establish two groups, those related to social and surgical factors, and those related to the anesthetic technique. The latter group is the one we find most interesting, since despite not finding significant differences, we found unexpected admissions only in the prilocaine group, and none in the chloroprocaine group. Moreover, since all surgeries are performed in the afternoon and the MASU closes at 22 h, patients that did not meet the discharge criteria will be necessarily admitted. And this is the most important limitation in this study, the limited hours of hospital stay in MASU on afternoon.
On the other hand using chloroprocaine 94.4% of the patients could ambulate after 3 hours compared to 31.2% of the patients who were administered prilocaine. Thus, using chloroprocaine might be favourable in late afternoon surgeries, as it will increase the likelihood of the patient being discharged before the MASU closes.
About complications, no case of urinary retention was recorded. This result can be explained by the restrictive fluid therapy used during the procedure (about 200 ml), since it is a surgery with little blood loss and the patients remain well hydrated since they can drink water up to 2 hours before the intervention. A similar result was also found in the study by urinary retention was not observed in the group of patients under spinal anesthesia [15].
We detected the appearance of leg discomfort during the motor blockade reversal process in several patients in the prilocaine group (Table 2), with no significant differences. In fact, one patient required anxiolytic treatment for this reason during their stay in the PACU. Further studies are needed to assess whether this effect could be related to the drug in question.
Due to the COVID-19 pandemic, during the periods in which no non-urgent or preferential surgical activity (oncologic surgery) was performed in our hospitals, the study had to be interrupted. However, since it was ambulatory surgery, it was one of the first non-preferential programmed surgeries to be restarted when the personnel were not required to attend COVID patients. Likewise, and although the study design was carried out before the pandemic began, the fact that it was a study in which loco regional anesthesia was used was an advantage, since these techniques allow for the mask to be kept on the patient during the procedure, minimizing the generation of aerosols in high risk communitary transmission that could cause transmission between the staff and the patient and vice versa [33-37].
Another aspect to consider when choosing a modality and an anesthetic drug is the economic aspect [9]. In our case, both local anesthetics have a very similar price, so the cost of the technique would not be a relevant factor. However, costs would increase if the drug used in intradural anesthesia had a higher risk of unexpected admission. In summary, the use of chloroprocaine in spinal anesthesia allows earlier ambulation than the use of prilocaine in major ambulatory surgery for inguinal hernias, since 48.1% ambulate 2 hours after lumbar puncture when using chloroprocaine compared to 4.5% in the case of prilocaine and at 3 hours after the puncture, 94.4% of the patients in the chloroprocaine group were able to ambulate compared to 31.8% in the prilocaine group and only 5.6% of patients in the chloroprocaine group were unable to ambulate compared to 68.2% of patients in the prilocaine group (Figures 3 and 4). With no differences in the appearance of complications or degree of patient satisfaction. There were also no significant differences in the number of unexpected admissions, even when assessing those specifically related to the anesthetic technique and the drug used. However, the fact that admissions for this reason were found only in the prilocaine group is worth considering, and carrying out more extensive studies on this issue may be beneficial as it could influence the drug used for spinal anesthesia in afternoon interventions near the MASU’s closing time.
All in all, spinal anesthesia with 1% chloroprocaine may be a good alternative to consider in major outpatient surgery procedures such as inguinal hernias due to the rapid recovery of motor block and onset of ambulation of patients compared to 2% hyperbaric prilocaine, especially in afternoon surgery. Moreover, in some cases chloroprocaine could become the anesthesia of choice as it offers advantages in patients with COPD, difficult airway, or less airway manipulation, or risk of airborne infection. New studies could be proposed in the future that compare spinal anesthesia with 1% chloroprocaine with other anesthetic techniques, general anesthesia or local anesthesia and sedation.
We would like to thank all colleagues from the anesthesiology service and the nursing service who have participated in the study for their contribution.
The authors declare no competing interests.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Forés I, Lloria E, Asensio I (2023) Prospective Randomized Study: Intrathecal 1% Chloroprocaine Versus 2% Hyperbaric Prilocaine in Major Outpatient Inguinal Hernia Surgery Performed During the COVID-19 Pandemic. J Anesth Clin Res.14:1102.
Received: 01-Mar-2023, Manuscript No. JACR-23-21990; Editor assigned: 03-Mar-2023, Pre QC No. JACR-23-21990 (PQ); Reviewed: 17-Mar-2023, QC No. JACR-23-21990; Revised: 24-Mar-2023, Manuscript No. JACR-23-21990 (R); Published: 31-Mar-2023 , DOI: 10.35248/2155-6148.23.14.1101
Copyright: © 2023 Forés I, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.