Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Case Report - (2024)Volume 15, Issue 4
Background: The aim of the study was to present clinical symptoms and provide results of optical coherence tomography examination of the anterior segment in patients who underwent iridotomy for the treatment of pseudophakic reverse pupillary block.
Case presentation: The analysis focused on two patients who, during postoperative follow-up after previously performed sutureless scleral fixation of a foldable three-piece intraocular lens, were found to have a very deep anterior chamber, a concave iris configuration and contact between the Intraocular Lens (IOL) optics and the iris. Based on clinical imaging and optical coherence tomography examination, pseudophakic reverse pupillary block was diagnosed. In both cases, laser iridotomy was performed.
Results: Improved anatomical relationships and resolution of symptoms associated with reverse pseudophakic pupillary block were confirmed in clinical and optical coherence tomography examinations.
Conclusion: Laser iridotomy in cases of pseudophakic reverse pupillary block allows restoration of normal anatomical relationships, reduces lens-iris contact, regulates intraocular pressure and avoids unnecessary surgical interventions. Optical coherence tomography technology enhances clinical imaging quality and facilitate managing this complication.
Pupillary block; Scleral sutureless fixation; Iridotomy; Optical coherence tomography
Pseudophakic Reverse Pupillary Block (PRPB) is a rare but serious complication of scleral fixation of Intraocular Lens (IOL). It can lead to recurrent episodes of IOL optics entrapment in the pupil, recurrent intraocular hemorrhages, pigment dispersion due to increased iris-lens contact and elevated IOP [1-3]. This condition results in a concave iris configuration associated with a pressure gradient between the anterior and posterior segments of the eye. It can manifest as significant deterioration of Visual Acuity (VA) and may require immediate intervention.
Previously described cases of PRPB occurred in patients after IOL implantation into the ciliary sulcus, into the capsular bag or after IOL scleral fixation [4-6]. This study presents two cases of PRPB following IOL sutureless fixation with the technique described by Yamane [7]. The aim of this article is to describe the clinical presentation, management approach and the role of Anterior Segment Optical Coherence Tomography (AS-OCT) in diagnosing and evaluating treatment outcomes of this complication.
Case 1
A 55-year-old male treated with scleral fixation of a three-piece IOL with Yamane technique on the first postoperative visit presented with Best Corrected Visual Acuity (BCVA) 0.8 and Intraocular Pressure (IOP) 8 mmHg. The lens was displaced anteriorly in the nasal quadrant. After pharmacological mydriasis, the lens was repositioned by horizontal positioning of the patient and the application of pilocarpine topically. Routine postoperative management was maintained. On the second postoperative day, the IOL was correctly positioned behind the iris, the anterior chamber was deep and IOP was 18 mmHg. On the following days, BCVA improved to 1.0 according to Snellen chart.
After 10 months, during a follow-up visit, deep anterior chamber, erythrocytes in the aqueous humour and concave iris configuration were observed together with the rise of IOP to 28 mmHg. AS-OCT confirmed the posterior bowing of the iris and the apposition of the IOL to the iris as shown in Figure 1A. PRPB was diagnosed. Laser Peripheral Iridotomy (LPI) was performed. After laser procedure, AS-OCT imaging revealed the proper iris configuration, increased distance between the IOL and the iris and a normal anterior chamber depth as shown in Figure 1B. Over the subsequent months, the patient was regularly controlled and no further IOL displacement was observed. The IOP returned to normal and good visual acuity was maintained. Visual field examination and retinal nerve fiber layer OCT showed no defects. Figure 1C shows there was no bleeding into the anterior chamber and normal anatomical conditions in the eye remained after 8 months (Figure 1).
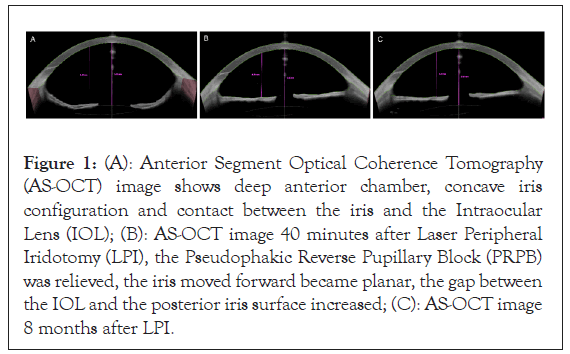
Figure 1: (A): Anterior Segment Optical Coherence Tomography (AS-OCT) image shows deep anterior chamber, concave iris configuration and contact between the iris and the Intraocular Lens (IOL); (B): AS-OCT image 40 minutes after Laser Peripheral Iridotomy (LPI), the Pseudophakic Reverse Pupillary Block (PRPB) was relieved, the iris moved forward became planar, the gap between the IOL and the posterior iris surface increased; (C): AS-OCT image 8 months after LPI.
Case 2
A 66-year-old male, 2 months after sutureless scleral fixation of the IOL with Yamane technique reported a deterioration of vision in his left eye. In the AS-OCT examination, a posterior bowing of the iris was observed, the mechanism of PRPB was diagnosed as shown in Figure 2A. LPI was performed, resulting in the improvement of iris configuration as shown in Figure 2B. During the 6-month follow-up, the patient remained under clinical care, IOP remained normal and BCVA was 0.9 according to Snellen chart. Figure 2C, shows repeated AS-OCT examinations confirmed the correct iris configuration and IOL position (Figure 2).
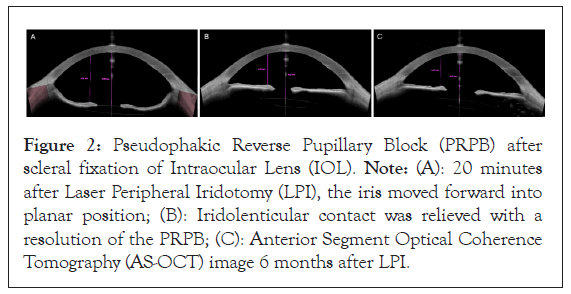
Figure 2: Pseudophakic Reverse Pupillary Block (PRPB) after scleral fixation of Intraocular Lens (IOL). Note: (A): 20 minutes after Laser Peripheral Iridotomy (LPI), the iris moved forward into planar position; (B): Iridolenticular contact was relieved with a resolution of the PRPB; (C): Anterior Segment Optical Coherence Tomography (AS-OCT) image 6 months after LPI.
In most cases, IOL sutureless scleral fixation is a safe and effective procedure. However, one of the rare complications following this type of surgery is PRPB. In the classic form of pupillary block, there is an obstruction to the flow of aqueous humor from the posterior chamber to the anterior chamber. This leads to increased pressure in the posterior chamber, causing the peripheral part of the iris to shift forward and narrowing the iridocorneal angle. Instead, in the case of PRPB, the IOP in the anterior chamber becomes higher than that in the posterior chamber, resulting in a concave iris configuration.
This condition is uncommon and was first described by Karickhoff [6]. Previously reported cases of PRPB mainly occurred in patients with the ciliary sulcus implanted IOL. Sulcus IOL implantation is a common procedure performed in complicated cataract surgery. A few reports of pseudophakic reverse pupillary block were described after scleral-fixated IOL implantation [8]. Later, isolated cases of this complication were described after sutureless fixation of a scleral three-piece intraocular lens using the Yamane technique. Bharathi, et al. [9], regarded potential causes that may contribute to PRPB suggested too close distance between scleral fixated IOL and the posterior iris surface due to short haptics or excessive tension during IOL fixation. Abushanab, et al. [10], described PRPB after phacoemulsification with in-thebag implantation of a single-piece IOL and underscore the value of ultrasonic biomicroscopy in the diagnosis and posttreatment follow-up. Moreover, the literature reports that PRPB may occur even several years after IOL implantation.
The characteristic iris configuration, deep anterior chamber and IOL apposition to the iris and in some cases, lens edge displacement anteriorly, can be visualized using AS-OCT, which facilitates diagnosis and treatment planning. In this report in both cases AS-OCT was helpful in confirming the diagnosis and evaluating the effectiveness of the applied treatment (reversal of PRPB signs after LPI). AS-OCT was used to assess changes in the depth of the anterior chamber as well as the distance between the IOL and the iris during follow-up.
The management of PRPB involves creating a pathway for aqueous humour flow between the chambers to eliminate the pressure gradient and reduce the posterior bowing of the iris. The use of LPI in our cases was effective and has a long-lasting effect.
Higashide, et al. [4], recommend intraoperative prophylactic peripheral iridectomies to prevent reverse pupillary block and help reduce the related postoperative complications. Given the rarity of this complication and the high efficacy of laser peripheral iridotomy in the postoperative period, we do not routinely use prophylactic peripheral iridectomy in patients with scleral fixation of an IOL using the Yamane technique.
Possible modifications of the technique described earlier by Yamane or specially designed three-piece IOLs may reduce the frequency of this complication in the future.
PRPB is characterized by the apposition of the IOL optic to the iris and its potential anterior displacement, posterior bowing of the peripheral iris and obstruction of aqueous humour flow from the anterior chamber to the posterior chamber through the pupil. This can lead to long-term consequences, including elevated IOP or recurrent hemorrhages into the anterior chamber or vitreous cavity. VA deterioration may result from lens displacement anteriorly, microhemorrhages or changes associated with elevated IOP. AS-OCT allows quantitative assessment of biometric parameters (anterior chamber depth, IOL distance from the iris) and observation of iris configuration changes after LPI. Early diagnosis and appropriate management of PRPB are essential to prevent potential complications and maintain good visual function. The choice of treatment method should be tailored to the individual case and LPI is an effective procedure that not only normalizes the pressure gradient between the chambers but also restores the correct iris configuration and IOL position at an appropriate distance from the iris. This study confirms the possibility of this complication occurrence after scleral fixation using the Yamane technique, which is currently widely used due to its shorter surgical time and good outcomes compared to methods employed previously.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Krix-Jachym K, Blagun N, Naszkiewicz-Blachnio K, Rekas M (2024) Pseudophakic Reverse Pupillary Block Following Sutureless Scleral Fixation of Intraocular Lens: Diagnostics and Treatment. J Clin Exp Ophthalmol. 15:982.
Received: 01-Jul-2024, Manuscript No. JCEO-24-32445; Editor assigned: 03-Jul-2024, Pre QC No. JCEO-24-32445 (PQ); Reviewed: 17-Jul-2024, QC No. JCEO-24-32445; Revised: 24-Jul-2024, Manuscript No. JCEO-24-32445 (R); Published: 02-Aug-2024 , DOI: 10.35248/2155-9570.24.15.982
Copyright: © 2024 Krix-Jachym K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.