Rheumatology: Current Research
Open Access
ISSN: 2161-1149 (Printed)
ISSN: 2161-1149 (Printed)
Case Report - (2021)Volume 11, Issue 6
Neurological pseudo-tumoral presentation of Behcet’s disease is rarely observed. We report the case of 23-year-old men who presented with temporo-spatial disorientation. He has also, bipolar aphtosis, right peripherical facial paralysis and ptosis. There was neither fever nor lymphadenopathies on the examination. Ophthalmological examination had objectified bilateral anterior uveitis. Serological tests and autoimmunity study were normal. The brain angio-Magnetic Resonance Imaging (MRI) showed intra parenchymal infiltrative lesion affecting right capsulothalamic region and the protuberance. The diagnosis of pseudo-tumoral Neuro-Behcet's Disease (NBD) is suspected. Treatment with corticosteroids and cyclophosphamide had improved clinical and radiological outcome after a 3-years follow-up. A history of recurrent oral and genital ulcers since 2 years, the clinical context and the significant response to steroids, confirmed that the brain mass is related to Neuro-Behcet's Disease (NBD).
Behcet's disease; Neurological involvement; Pseudo-tumoral lesion
Neurological involvement is not specific and occurs in 1% to 59% [1] of patients with Behçet's disease. They include central nervous system involvement and vascular angeitis. The pseudotumoral form of neuro-Behcet’s disease has been poorly described, and only a few cases have been reported in the literature [2,3]. Clinical features frequently consist of headache, pyramidal signs with hemiparesis, behavioural change and sphincter impotence, whereas morphological findings show inflammatory lesions in the brainstem and hemispheric area. Typical MRI findings are small scattered lesions in multiple areas of the basal ganglion region, brainstem or internal capsule, with hypersignal in T2-weighted MRI and contrast enhancement with gadolinium. We describe a new case of Pseudo-tumoral cerebral involvement during behçet's disease.
The patient was a 23-year-old man who presented with 10 days history of temporo-spatial disorientation. In the physical examination, he was found to have right-upper facial nerve palsy, ptosis, right brachial paresis and together oral and genital ulcers. There is no fever or other abnomalies in the neurological examination. Laboratory analyses showed negative results in serological tests for syphilis, hepatitis B virus, hepatitis C virus and human immunodeficiency virus, and negative findings in an autoimmunity study. Renal function test, liver function test and serum electrolyte were normal. Him erythrocyte sedimentation rate was elevated. Lumbar puncture could not perform. Computed tomography scan noted thalamo-capsular lesion enhanced by contrast with perilesional edema (Figure 1). Brain Magnetic Resonance Imaging (MRI) revealed the presence of an intra-parenchymal infiltrative lesion affecting right capsulothalamic region and the protuberance with a normal imaging of the venous and arterial system (Figures 2 and 3). Stereotactic biopsy of cerebral lesion was refused by the patient. Thoracoabdominal computed tomography was normal. Consultation with the ophthalmologist revealed bilateral anterior uveitis. After reviewing his past medical history, he reported a 2-year history of recurrent oral and genital ulcers, which suggested a diagnosis of Behcet's disease and stereotactic biopsy was not carried out. Treatment was initiated with methyl-prednisolone pulse therapy, followed by oral prednisone (1 mg/kg/day), colchicine (1 mg/ day) and monthly cyclophosphamide pulses (1 g/month). After 3 years of follow-up, the patient has no clinical neurological symptoms and brain MRI revealed considerable regression of previous lesions and persistence of wallerian degeneration in left centrum semi ovale in Figures 4 and 5. Gadolinium-enhanced axial T1-weighted images show no abnormally enhancing lesion in Figure 6.
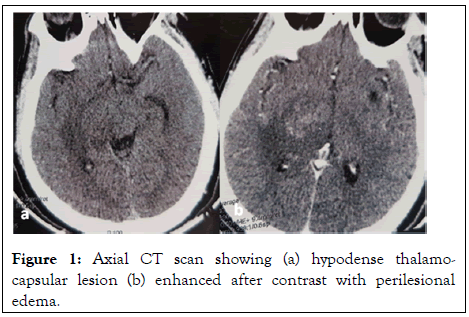
Figure 1: Axial CT scan showing (a) hypodense thalamocapsular lesion (b) enhanced after contrast with perilesional edema.
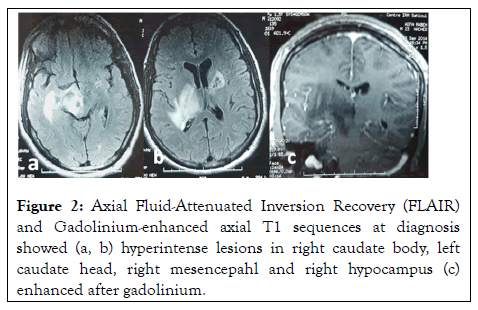
Figure 2: Axial Fluid-Attenuated Inversion Recovery (FLAIR) and Gadolinium-enhanced axial T1 sequences at diagnosis showed (a, b) hyperintense lesions in right caudate body, left caudate head, right mesencepahl and right hypocampus (c) enhanced after gadolinium.
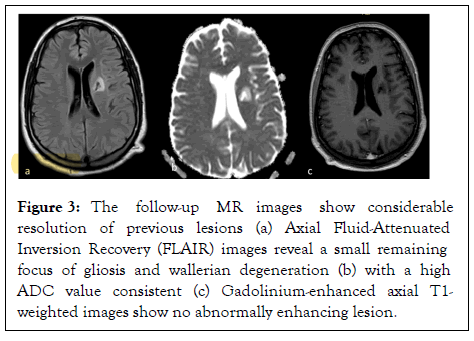
Figure 3: The follow-up MR images show considerable resolution of previous lesions (a) Axial Fluid-Attenuated Inversion Recovery (FLAIR) images reveal a small remaining focus of gliosis and wallerian degeneration (b) with a high ADC value consistent (c) Gadolinium-enhanced axial T1- weighted images show no abnormally enhancing lesion.
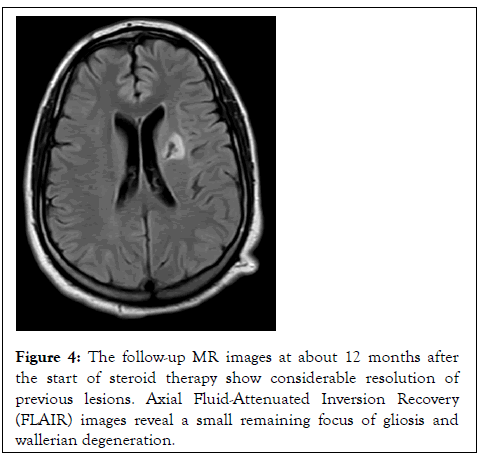
Figure 4: The follow-up MR images at about 12 months after the start of steroid therapy show considerable resolution of previous lesions. Axial Fluid-Attenuated Inversion Recovery (FLAIR) images reveal a small remaining focus of gliosis and wallerian degeneration.
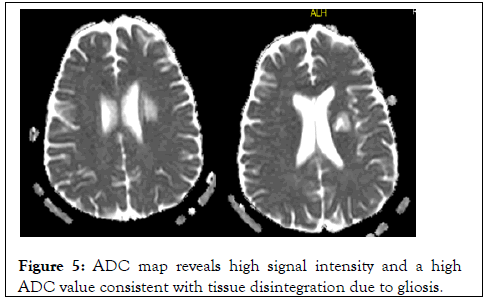
Figure 5: ADC map reveals high signal intensity and a high ADC value consistent with tissue disintegration due to gliosis.
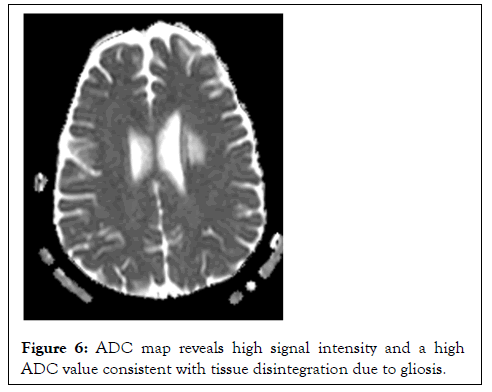
Figure 6: ADC map reveals high signal intensity and a high ADC value consistent with tissue disintegration due to gliosis.
Behçet’s disease is a multisystem inflammatory disorder of unclear aetiology. It is characterized by recurrent oral and genital ulcers, skin lesions and uveitis. Other manifestations include arthritis, gastrointestinal ulcerations, thrombophlebitis, and central nervous system disease can be observed. Neurological involvement is uncommon in Behçet’s disease, and has a highly variable prevalence. An atypical rare form with pseudotumoral lesions has been described in literature and only a few cases have been reported. The main difficulty in our case was to relate the mass to neuro-Behçet disease or other central nervous system disease. Neuro-Behçet’s disease can mime neurologic manifestations of multiple sclerosis, systemic lupus erythematosus, cerebral tumors or abscesses, or stroke in young adults [4,5]. Neuro-Behçet’s disease can mime neurologic manifestations of multiple sclerosis, systemic lupus erythematosus, cerebral tumors or abscesses, or stroke in young adults. Some authors do stereotactic biopsy to rule out these diagnoses but it is unnecessary for the diagnosis of neuro- Behcet’s disease [6,7]. Likewise, the histological findings are not specific. Brain MRI is the most sensitive exam during NBD [8]. The common lesions of NBD are located at the mesodiencephalic junction, followed by the pontobulbar region [9]. The lesions are bilateral in approximately one-third of the cases, and hemispheric lesions are not commonly seen. Treatment with glucocorticoids and cyclophosphamide is accompanied by a considerable regression of the lesion. Even though brain tumor can respond to steroid, the history of recurrent oral and genital ulcers, the clinical context and the significant response to steroids, indicated that the mass is rather related to neuro-Behcet’s disease [10,11]. Twenty-seven cases were described in literature, with predominance in men and a median age of 38 years-old ranging from 16 to 59 years old. The most frequent lesion localization was in the thalamus described in our 3 cases and the basal nuclei. All the patients, in literature, were initially treated with high-dose glucocorticoids, orally or intravenously. Others associated immunosuppressants such as azathioprine, cyclophosphamide, methotrexate and chlorambucil [1]. The neurological prognosis may be assessed by the Rankin’s score. The Rankin’s score was higher at diagnosis of pseudotumoural NBD compared with classical NBD, confirming the more severe neurological presentation of the former. The prognosis of pseudotumoural NBD may thus be worsened because of more severe presentation, longer time to diagnosis and/or delayed treatment because of diagnostic difficulties.
Pseudotumoural NBD is a rare but severe manifestation of behcet’s disease. It should be evoked in front of cerebral mass as a differential diagnosis. Rapid and early recognition of this condition is important in order to improve functional and vital prognosis by instituting an adequate early treatment. A pseudotumor in NBD should be considered in the differential diagnosis of brain masses. Biopsy is not necessary to confirm the diagnosis of behcet’s disease unless extra-neurological manifestations are absent.
Citation: Atig A, Thabet M, Guiga A, Yahia WB, Ghannouchi N (2021) Pseudo-Tumoral Cerebral Involvement during Behcet’s Disease. Rheumatology (Sunnyvale). 11: 289.
Received: 09-Jul-2021 Accepted: 23-Jul-2021 Published: 30-Jul-2021 , DOI: 10.37421/2161-1149.2021.11.289
Copyright: © 2021 Atig A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.