Journal of Hepatology and Gastrointestinal disorders
Open Access
ISSN: 2475-3181
+44-77-2385-9429
ISSN: 2475-3181
+44-77-2385-9429
Case Report - (2022)Volume 8, Issue 2
Pyogenic Granuloma (PG) typically presents as a benign vascular lesion of the skin and mucosal surfaces, however, cases in the Gastrointestinal (GI) tract have been reported. It is a form of lobular capillary hemangioma that can easily bleed on endoscopic intervention and can be misdiagnosed as a malignant lesion based on appearance. We report a case of a 73-year-old male who presented with a couple of days of hematochezia and was found to have approximately 5 cm polypoid mass of ascending colon that eventually required hemicolectomy for management of persistent lower GI bleed. We review the literature on PG cases of the colon and rectum to understand the presenting symptomatology, endoscopic findings, therapeutic intervention, and surveillance data.
Pyogenic granuloma; Colon; Colonoscopy; Lower gastrointestinal bleed
Pyogenic Granuloma (PG) or granuloma pyogenicum is a type of benign vascular lesion [1]. First discovered in 1897 and was originally thought to be caused by bacterial infection, however, the term PG is a misnomer because it is not caused by or associated with infection and neither is it a true granuloma [2]. Pyogenic granuloma is a benign subtype of lobular capillary hemangioma, which is an inflammatory vascular lesion [3]. The underlying pathogenesis is unclear but it is believed to arise from a reactive process against mucosal irritation, such as trauma [1]. There is also increased association in pregnant females indicating a role of hormonal imbalance in the pathogenesis [2]. It can start as a tiny erythematous papule or nodule that is susceptible to bleeding and ulceration, and typically progresses in size over a period of a few weeks [2]. It typically affects the skin and mucosal surfaces, but rarely the gastrointestinal tract. Here we report a case of PG of the colon and review the literature of PG in the colon and rectum.
A 73-year-old African American male was admitted to the hospital with 2 days of melena and anemia. His past medical history was significant for hypertension, heart failure with preserved ejection fraction, end-stage renal disease on hemodialysis. Current medications were significant for clopidogrel. Physical examination was unremarkable. Labs showed hemoglobin of 5.0 (reference range 13.5 to 17.5 gm/dL) from 12.4 two months prior, platelet count, and coagulation profile was normal. He was admitted to the ICU for close monitoring and stabilization. EGD showed no source of bleeding but noted fundic type gastric mucosa with moderate gastritis. Random biopsies showed Helicobacter pylori infection for which he completed treatment. Colonoscopy showed a friable, hard mass involving 75%-80% of the ascending colon wall proximally and circumferential encasement distally (Figure 1). It was nonobstructing and spread over an area of 5 cm. multiple biopsies were acquired which revealed fragments of pyogenic granuloma without evidence of neoplasm (Figures 2 and 3). He continued to have lower GI bleeding which required massive transfusion protocol and finally a right hemicolectomy. The pathology report confirmed a large area of ulcerated pyogenic granulomatous tissue to the depth of submucosa, in ascending colon, with scattered patches of residual adenomatous colonic mucosa. The patient had an uneventful postoperative hospital course. He presented 2 weeks after discharge with melena. Repeat colonoscopy showed an erythematous anastomotic site with tiny clean-based ulcerations and one polypoid area that were biopsied. Pathology showed only granulation tissue. The patient has been doing well afterward with no recurrence of GI bleeding.
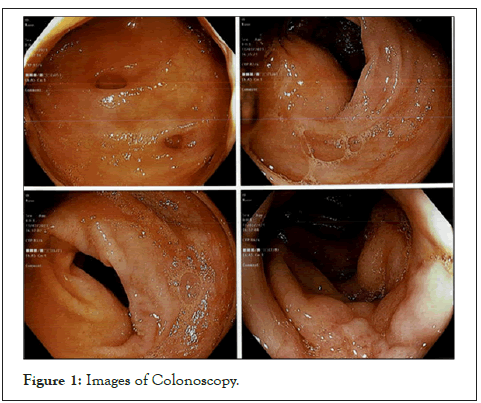
Figure 1: Images of Colonoscopy.
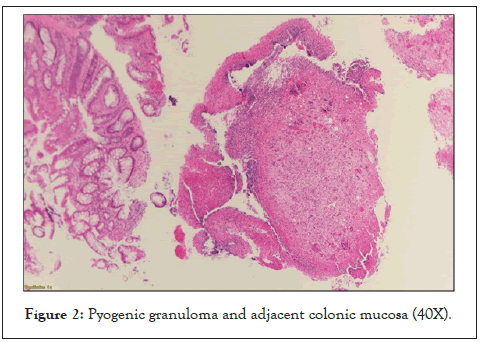
Figure 2: Pyogenic granuloma and adjacent colonic mucosa (40X).
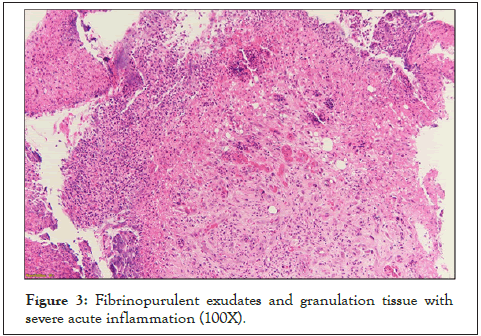
Figure 3: Fibrinopurulent exudates and granulation tissue with severe acute inflammation (100X).
A type of benign vascular lesion is known as Pyogenic Granuloma (PG) or granuloma pyogenicum [1]. Pyogenic granuloma is a benign subtype of lobular capillary hemangioma, which is an inflammatory vascular lesion [3]. It can start as a tiny erythematous papule or nodule that is susceptible to bleeding and ulceration, and typically progresses in size over a period of a few weeks [2]. It typically affects the skin and mucosal surfaces, but rarely the gastrointestinal tract. The histopathological findings of PG of the skin and oral mucosa and the gastrointestinal tract are the same. They are characterized by capillary hemangioma arranged in a lobular pattern and filled with clusters of small capillary vessels and a single layer of endothelial cells [4].
For PG of the whole Gastrointestinal (GI) tract PG, the median age at diagnosis is 59-64 years, with an almost equal sex distribution [5]. The most reported anatomical locations are the esophagus and the sigmoid colon. The median PG diameter was 15 mm and rarely above 20 mm [1]. There is data indicating the under diagnosis of GI PG possibly due to incorrect diagnosis as an inflammatory and/or hyperplastic polyp [1]. Here we review the case of patients with PG of the colon or rectum (Table 1). In our review, the median age of patients with polygenic granuloma involving the colon or rectum is 54 years. The gender distribution was almost equal with males 12 out of 22 (55%) and female 10/22 (45%). The most common presentation is with signs or symptoms of lower GI bleed or iron deficiency anemia. On endoscopy, the lesions can appear sessile or polypoid with or without a stalk. There has been reported overlying hyperemia and whitish deposit/exudate. Appearance resembling malignancy has been reported [6]. The use of magnifying endoscopy with narrow bend imaging can show many microvessels with a congested network [6,7]. Endosco- pic ultrasound may reveal the lesion extending to the mucosal layer and rarely to the submucosal layer [8]. Attempts at biopsy or resection can lead to bleeding which has required hemostatic clips for homeostasis [1]. In addition to the histological finding, immunohistochemistry for CD31 or CD34 can be used to identify endothelial cells. In our review, all of the lesions in adult patients were removed via endoscopic polypectomy except in three cases [9,16,21]. One patient required treatment for her large hepatic cysts therefore laparoscopic resection of polygenic granuloma was pursued [9]. The other two patients had relatively larger lesions, one measuring approximately 3 × 2 cm, which needed surgical resection [16]. There was no recurrence except for 1 patient with recurrence 13 years later closer to the previous resection site [2]. Overall, none of the lesions showed an increased risk or tendency for colon malignancy.
| Author | Age | Gender | Presentation | Location | Size/description | Treatment | Follow up |
|---|---|---|---|---|---|---|---|
| Lui et al. [15] | 74 years | M | Hematochezia | Ascending colon | Size N/A. ‘malignant looking’ whitish coating and easy contact bleeding | Endoscopic polypectomy | N/A |
| Val-Bernal et al. [16] | 72 years | M | Anemia, change in bowel habit, weight loss | Ascending colon | 30x20 mm. Polypoid lesion | Hemicolectomy | N/A |
| Thibault et al. [11] | 54 years | M | Months of minor rectal bleed | Descending colon | 20-mm. Pedunculated polyp with large white-coated head. | Endoscopic polypectomy | N/A |
| Nakaya et al. [9] | 59 years | F | Melena and fecal occult blood test (FoBT) positive | Descending colon | 15 mm. Light-red, sessile lesion | Endoscopic biopsy followed by laparoscopic procedure. | No recurrence at 1-year |
| Meyer-Herb et al. [17] | 54 years | M | 2 days hematochezia | Descending colon | 10-mm. Patelliform, wide-based polyp with central scarring and partial ulcerated surface | Repeated Endoscopic polypectomy | 3 months follow-up colonoscopy showed polyp recurrence and polypectomy repeated. 8-week follow up with no recurrence |
| Field et al. [13] | 80 years | F | 1-week history of rectal bleeding | Rectum | Size N/A. Red nodular lesion at the recto-sigmoid junction, | Endoscopic polypectomy | N/A |
| Hamada et al. [7] | 59 years | M | Altered bowel habit | Rectum | 10 mm. Reddish, irregular shaped, semi-pedunculated polyp in the rectum | Endoscopic mucosal resection | N/A |
| Devrim et al. [14] | 49 years | F | Surveillance colonoscopy | Rectum | Size N/A. Polypoid structure | N/A | N/A |
| Asayama et al. [6] | 57 years | F | Fecal occult blood test ( FoBT) positive | Rectum | 5 mm. A reddish, irregular-shaped, protruding lesion, covered with white exudate | Endoscopic mucosal resection (EMR) | N/A |
| Sinha et al. [18] | 18 years | M | 1 year of bleeding per rectum | Rectum | Multiple reddish polypoidal lesions of variable sizes. Some superficial ulceration | 3 sessions of endoscopic polypectomy followed by argon plasma coagulation (APC). | Repeat sigmoidoscopy showed minimal residual lesion |
| Giaccaglia et al. [2] | 43 years | F | Hematochezia | Rectum | 30x20 mm. Polypoid lesion | Transanal endoscopic microsurgery | 13-year recurrence, new rectal 3x2 cm polypoid lesion, removed with transanal endoscopic microsurgery |
| Moparty et al. [8] | 26 years | F | Asymptomatic. Follow-up endoscopy for polyp resection | Rectum | 5 mm. Reddish-colored sessile polyp | Endoscopic polypectomy | N/A |
| Blanchard et al. [22] | 5 years | F | 2-month painless rectal bleed | Rectum | 4 mm. Polypoid lesion in the rectum | Endoscopic polypectomy | N/A |
| Castle et al. [23] | 16 years | M | Hematochezia | Rectum | Contiguous, near-circumferential exophytic friable masses | Transanal mucosal sleeve resection | No recurrence at 2 years |
| González-Vela et al. [10] | 62 years | M | Hematochezia | Sigmoid Colon | 20 mm. A polypoid lesion with ulceration on top and covered with a white exudate | Endoscopic polypectomy | No recurrence at 8 months |
| Garrido et al. [5] | 64 year | M | Iron deficiency anemia | Sigmoid colon | 14 mm. Pedunculated polyp, short wide stalk, lobulated and reddish head with an adherent whitish deposit | Endoscopic polypectomy | N/A |
| Chen et al. [19] | 36 years | M | 1 year of loose stool, and weight loss. | Sigmoid colon | 4 to 8 mm. Ten sessile polyps with hyperemic overlying mucosa | Endoscopic polypectomy | No recurrence at 1 month |
| Seo et al. [20] | 44 years | F | 2 weeks of rectal bleeding | Sigmoid colon | 12 mm. Polypoid lesion with hyperemic overlying mucosa | Endoscopic mucosal resection | No recurrence at garof6 months |
| Garofalo et al. [24] | 4 months | M | Colicky abdominal pain, vomiting, and rectal prolapse | Sigmoid colon | 20 x 19 mm. Tumor-like lesion | Segmental resection with anastomosis of sigmoid colon | N/A |
| Yan et al. [12] | 40 years | M | 3-month history of rectal bleeding | Transverse colon | 25 mm. Pedunculated reddish polyp with a short wide stalk and an adherent whitish deposit on the head | Endoscopic polypectomy | No recurrence at 3 months |
| Hocke et al. [21] | 60 years | F | Screening | Transverse colon | Size N/A. Large, vulnerable circular growing tumor, pseudopolypoid-like region next to it | Right hemicolectomy | N/A |
| Blanchard et al. [22] | 18 months | F | Fever and rectal bleed | Transverse colon | Size N/A. Circumferential black necrosis. | Endoscopic polypectomy | Repeat colonoscopy in 2 weeks without necrosis |
Table 1: Reports of pyogenic granuloma of colon and rectum.
Here we report the largest size of a pyogenic granuloma case presenting with brisk lower GI bleeding that required surgical intervention with colectomy. In review of literature, PG or LCH of the colon and rectum is a rare entity but important for the clinician to properly recognize as it can be overdiagnosed as a suspected malignant lesion on endoscopy evaluation. The management can be challenging as the lesions are vascular and can easily bleed with intervention. Lastly, the follow-up surveillance period still remains unclear but they seem to be devoid of malignant potential.
Citation: Ullah H, Searls L, Iqbal S (2022) Pyogenic Granuloma of the Colon Presenting as Brisk Lower GI Bleed: Case Representation. J Hepatol Gastroint Dis. 8:201.
Received: 10-Feb-2022, Manuscript No. JHGD-22-15818; Editor assigned: 15-Feb-2022, Pre QC No. JHGD-22-15818 (PQ); Reviewed: 02-Mar-2022, QC No. JHGD-22-15818; Revised: 08-Mar-2022, Manuscript No. JHGD-22-15818 (R); Published: 15-Mar-2022 , DOI: 10.35248/2475-3181.8.22.201
Copyright: © 2022 Ullah H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.