Gynecology & Obstetrics
Open Access
ISSN: 2161-0932
ISSN: 2161-0932
Research Article - (2023)Volume 13, Issue 2
Background: More than 52 million under five children have acute malnutrition, of which 27.8 million and 13.2 million are South Asia and Sub Saharan Africa, respectively. In addition it is estimated that 25-35 million children are severely malnourished globally which is responsible for the death of more than one million. Despite numerous advances made in improving child health and the clinical management protocols for treating severe acute malnutrition at treatment centers, evidences concerning the recoveries are scarce.
Method: A hospital based retrospective cross-sectional study was conducted to collect information from 366 records of severely malnourished children who were admitted from January 2016 to December 2019. Data were coded, entered into EPI data version 3.1 and exported to SPSS version 20 for analysis. To identify associated factors, cox proportional hazard analysis was computed p-value <0.05 at 95% confidence intervals were considered as statistically significant. Survival data analyses were carried to show the survival rate. Kaplan-Meier survival analysis was computed to estimate survival function; the log rank test was used to compare survival curves.
Results: The recovery rate of the reviewed records was 79% and the overall median recovery time was 11 days. Those children with an age of 24 onths-59 months had 3 times more likely to recover compared to those children between 6 months-11 months (AHR 2.79 (95% CI: 1.32-5.92). Children who were admitted without tuberculosis infection were 58% increased of recovery compared to those who had tuberculosis as a comorbidity (AHR: 0.422 95% CI: 0.202-0.878)., similarly children who were not presented with anemia are 73% better to recover compared to those who had anemia with (AHR: 0.269; 95% CI: 0.116-0.621). Likewise children who received IV fluids during rehabilitation are 50% more likely to recover compared to those who had not received (AHR: 0.508; 95%CI; 0.322-0.802).
Conclusion: The overall recovery and other outcome indicators were in the range of the minimum international sphere standard. Mean weight gain and mean length of hospitalization were in the acceptable range of international standards.
Severe acute malnutrition; Recovery; Inpatient; Fik hospital; Anemia
AHR: Adjusted Hazard Ratio; AOR: Adjusted Odds Ratio; CI: Confidential interval; COR: Crude Odds Ratio; EDHS: Ethiopian Demography Health Survey; MUAC: Mid-Upper Arm Circumference; OTP: Outpatient Therapeutic Program; SAM: Severe Acute Malnutrition; SC: Stabilization Center; SD: Standard Deviation; SPSS: Statistical Package for Social Science; TB: Tuberculosis; TFU: Therapeutic Feeding Unit; WHO: World Health Organization
Malnutrition is defined as a state in which the physical function of an individual is impaired to the point where he/she can no longer maintain adequate body performance processes such as growth, development, performance of physical work and recover from disease. Malnutrition remains the major cause morbidity and mortality in the world [1-3]. Malnutrition is categorized as acute or chronic or it can be either under nutrition or overnutrition (obesity) [4]. There are 3 forms of malnutrition: Wasting, stunting and under-weight. This can also be categorized as either moderate or severe malnutrition and can appear isolated or in combination, but most often overlap in one person or population.
Severe Acute Malnutrition (SAM) or wasting is defined by a very low weight for height (below-3 z scores of the median WHO growth standards), by visible severe wasting, or by the occurrence of nutritional edema. In children aged 6-59 months, additionally Mid Upper Arm Circumference (MUAC) less than 110 mm is also reveals severe acute malnutrition for children greater than six month. The world experiences a considerable malnutrition burden among its under-five population. The average global prevalence of overweight in the under-five population is 5.9% and the prevalence of stunting is 21.9%, the prevalence of wasting in the under-five population is 7.3%, only 41.2% of infants less than 6 months are exclusively breastfed, while the world's average low birth weight prevalence is 14.6%.
In 2018, Africa and Asia accounted for more than nine out of ten of all stunted children globally, which means 39.5% and 54.9% of total global wasting, respectively [5]. Due to the increasing demand for better management to the SAM patients treatment modality are updated every time, currently there are two modality for the treatment of SAM patient in which children who have medical complication and fail appetite test are admitted as impatient or Stabilization Center (SC) and those who have no medical complication and pass the appetite test are admitted as Outpatient Therapeutic Program (OTP) [6].
Treatment outcomes could be stated as recovered, defaulted, died, medical transfer, and non-respondent based on WHO management protocol [7]. Based on that, the recovery, death, and default rates were considered as acceptable when greater than 75%, less than 10% and less than 15% respectively and alarming when less than 50, greater than 15 and greater than 25%, respectively. Moreover, weight gain, length of stay, and coverage were thought of as acceptable when ≥8 g/kg/day, <4 weeks and >50%-70%, respectively, and considered as alarming when less than 8 g/kg/day, greater than 6 weeks, and less than 40% respectively [8].
Globally more than 52 million under five children are having acute malnutrition, of which 27.8 million and 13.2 million are South Asia and Sub Saharan Africa, respectively. In addition it is estimated that 25-35 million children are severely malnourished globally which is responsible for the death of more than one million [9]. In 2016, 17 million children under 5 were affected by severe acute malnutrition globally, in which more than three-fourth of them are from South East Asia and sub Saharan Africa with nearly half of under-five mortality attributable to malnutrition [10].
According to the global nutrition report in 2018, the burden of malnutrition over the world remains un acceptably high and progress of reduction is unacceptably slow, due to this malnutrition is responsible the morbidity of more than any other co-use where in globally; 150.8 million are stunted, 50.5 million are wasted and 38.3 million are overweight. Meanwhile, 20 million babies are born of low birth weight each year, which in turn manifesting childhood stunting [11].
In Ethiopia, even though the country has made tremendous effort to improve the nutrition of fewer than five children still the burden of malnutrition remains high. According Ethiopian Demography Health Survey (EDHS) 2016 in fewer than five children 10%, 24%, and 38% are wasted, under weight and stunted, respectively, highlighting the worst affect in a country. Somali region is the leading of wasting in fewer than five children in Ethiopia with prevalence rate of 23% [12].
SAM is a major public health problem in globally and at national level, The 2013 cost of hunger in Africa study in Ethiopia estimated that malnutrition cost the economy $4.8 billion USD (55.5 billion ETB) in 2009 from absenteeism, reduced physical capacity, and increased health care costs, indicating 16.5 percent of Gross Domestic Product (GDP). On the contrary, spending nutrition can have a massive return on investment compared to other global health interventions [13].
Burden and impact of acute malnutrition remain high, child deaths from malnutrition persist alarmingly high, in large part due to the extremely limited access to treatment: Only one child out of ten who suffers from the most severe form of acute malnutrition can currently access the treatment they urgently need.
Typically, children treated in the community with uncomplicated SAM have a case fatality of less than 5%, whilst children treated at health facility because of complicated SAM have a reported case fatality of 10% to 40% [14]. Different studies conducted in Ethiopia about treatment out come and recovery rate show different results including the study conducted in Jimma specialized teaching hospital showing recovery rate of 77.8%, another study conducted in Ayder referral hospital in Mekelle showed recovery rate of 43.6% and one the conducted in Diredawa Dilchora hospital showed recovery rate of 69.9% [15-17].
Since malnutrition remarked a major public health problems in the country there is also a challenges faced during while handling inpatients cases including limited inpatient capacity, lack of enough skilled staff in the hospitals to treat the large numbers needing care, serious risk of cross infections for immune suppressed children with severe acute malnutrition, so to discover contextual factors that may have positive impact on recovery rate therefore this study will assess the recovery rate and associated factors of children admitted with severe acute malnutrition at therapeutic feeding unit of Fik primary hospital. The finding of this study will help the proper implementation of nutrition rehabilitation units and may help planners and decision makers. In addition to that it will fill the knowledge gap related to recovery rate and associated factors of malnutrition among under-five children, also the information gained from this study will serve as a preliminary study for further studies in the context of Ethiopia and Somali region in particular. This study aimed to assess the recovery rate and associated factors among children aged 6-59 months with severe acute malnutrition at the inpatient unit of Fik primary hospital, Somali region Ethiopia.
Study area and period
The study was conducted at Fik hospital; the hospital is located in Fik town the Zonal city of Erer zone and provides service more than 400,000 population living the two zone of Erer and Nogob. The hospital has Therapeutic Feeding Center (TFC) or stabilization center since 2009 in line with FDRE MOH SAM management protocol in children less than five years. The study was conducted from April 1st to 31st, 2020.
Study design
A hospital based retrospective cross-sectional study design was used.
Source of population
The source of the population were all children aged 6-59 months who were admitted to the inpatient therapeutic feeding units with the diagnosis of severe acute malnutrition in Fik hospital.
Study population
All children aged 6-59 months who were admitted to the inpatient therapeutic feeding units with the diagnosis of severe acute malnutrition from January 2016 to December 2019.
Eligibility criteria for sample population
Inclusion criteria: All children aged 6-59 months who have been admitted Fik hospital based on Federal ministry of health of Ethiopia admission criteria for severe acute malnutrition from January 2016 to December 2019.
Exclusion criteria: Records with incomplete information were excluded.
Sample size determination
The sample size for recovery rate was calculated using single population proportion formula. A study conducted in Dilchora referral hospital, Eastern Ethiopia showed recovery rate 69.9% (33) which gives us below sample size.
Where,
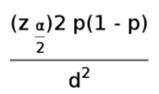
n=Sample size derived from estimation formula.
Zα/2=Value of z at the confidence level of 95%=1.96.
P=Recovery rate of children who had been managed for SAM=0.699 (69.9%).
d=Margin of error to be tolerated and taken as 5%.
Using the above formula the sample size is 323.
By considering 10% of compensation for missing or incomplete data, the final sample size of this study will be 356.
Two population proportion formulas were used to determine a sample size for the second objective that is associated factor identification, two key predictors from the previous study was selected according to the following assumptions and computed by EPINFO version 7.
Since the sample size of the second objective is greater than the first one which is 366 the greater one will be our final sample size of this study which is 366.
Sampling procedure
The study participants were selected by simple random sampling technique from registration log book based on their unique identification number.
All records from January 2016 to December 2019 were reviewed; records were collected from the card store by using the card number then were cross checked with SC registration book.
Data collection method
Data collection tool: A check list was developed from standard treatment protocol for managing severe acute malnutrition, SAM registration log book, SAM monitoring multi chart and reviewing related literatures to collect the required individual information from the relevant documents. The checklist includes, demography (age, sex and residency), anthropometry (weight and height/length, MUAC), presence or absence of edema, immunization status, medical diagnosis at admission (co morbidities) and treatment outcome of severe acute malnutrition.
Data collection procedure: Four data collectors (diploma nurses), who have experience and trained on SAM management, two supervisors have been recruited then two days of training were given. Records of eligible children were retrieved from the registration book; records with incomplete information were excluded. Records that have admission type, sex, place of residence, age of the child, anthropometry measurements medical complications, routine medications and outcome of the child were retrieved. All data were collected using a pre-tested checklist.
Study variables
Dependent variable: Recovery rate, (recovered, and not recovered).
Independent variables: Socio-demographic variables (sex, age), immunization, medical comorbidities, type of malnutrition, routine medication and length of stay in hospital.
Operational definitions: Recovered: children with severe acute malnutrition declared as cured recovered in the log book of inpatient therapeutic feeding units.
Not recovered: defined as children discharged from inpatient therapeutic feeding units with outcome other than recovery in this study (death, default, and non-responder, on treatment).
Severe Acute Malnutrition (SAM): Weight for height ratio of less than minus 3 standard deviations below the median WHO growth standards or presence of nutritional edema.
Inpatient management: Management of SAM of children of 0-59 months with medical complications or poor/fail appetite.
Defaulter: A SAM patient who becomes absent continuously from the therapeutic feeding program inpatient care for 48 hour.
Non-responder: SAM patient admitted to in patient that do not reached discharge criteria after 40 days in the inpatient program.
Died: Admitted children with SAM discharged whose treatment outcome ended with dead.
Unknown: Patients that has left the program but his outcome (actual defaulting or death) is not confirmed/verified by a home visit.
Medical transfer: Patient that is referred to a health facility/ hospital for medical reasons and that health facility will not continue the nutritional treatment.
Weight gain: Discharge weight minus minimum weight divided by minimum weight times the number of days between minimum weight and discharge day.
Average weight gain: The sum of weight gains divided number of 6-59 months cured.
The length of stay: Number days that the patient stayed in an impatient during a single episode in the TFU.
Average length of stay: Sum of length of stay divided number of 6-59 months children cured.
The type of malnutrition: Grouped as marasmus (no edematous), kwashiorkor (edematous), marasmus kwashiorkor (both edema and severe wasting) and visible severe wasting.
Data quality control
Check list was prepared after reviewing different literature to record the necessary information from the registration book. Prior to the start of data collection, two days training were given for the data collectors about study objectives and how to fill the check list. Pretest was conducted on 5% of the total sample size to test consistency of the check list. During data collection, close super vision were carried out by supervisor and principal investigator. Before receiving the filled checklist every two data collector has been checked by one supervisor to ensure consistency and completeness.
Data processing and analysis
Data were entered in to Epi info version 3.1 statistical software and then exported to SPSS version 20 for analysis. Crosstabulation and frequency tables were used to report the descriptive data. The recovery rate from SAM was estimated using Kaplan-Meier procedure. The log-rank test was used to test whether the observed difference of recovery between different groups of predictor variables is significant or not. Multivariate Cox proportional hazard regression analysis was carried out to identify predictor variables. Variables having a P-value ≤ 0.25 during binary variable Cox proportional hazard regression analysis were entered into multivariate analysis. P-value <0.05 was considered statistically significant. Both Crude Hazard Ratio (CHR) and Adjusted Hazard Ratio (AHR) with 95% Confidence Interval (CI) were used to show the strength of association.
Dissemination of research findings
The study results will be submitted and presented to Jigjiga university, school of graduate studies, public health department. The summary and recommendations will be shared to Fik hospital, zonal health bureau and regional health bureau.
Socio-demographic, admission type category, SAM category, breast feeding and referral status of the child characteristics
Records of 366 children between the age of 6-59 months with the diagnosis of Severe Acute Malnutrition (SAM) admitted to TFU from January 2016 to December 2019 in Fik primary hospital; 99 (27%) were between the age of 6-11 months, 142 (38.8) between 12-23 months and 125 (34.2%) were in 24-59 months respectively. The mean (± SD) of the age of the admitted children was 18.23 (± 11.769) months. Almost more than half 199 (54.4%) of the admitted children were Male. More than half 208 (56.8%) came from the rural areas. The majority of the children 290 (79.2%) were newly admitted whereas 76 (20.8%) were readmitted to the program. About breast feeding on admission children in the age of 6-23 months less than half 113 (46.9%) were on breast feeding.
Severe wasting was the topmost cause of admission 262 (71.6%), 15 (4.1%) were admitted only for edema, 40.9 (10.9%) were admitted for MUAC of less than 11 cm and the remaining 49 (13.4%) were admitted for both wasting and edema. Most of the admitted children in the program were self-referred 225 (61.5%) (Table 1).
| Variables | Category | Frequency | Percent (%) |
|---|---|---|---|
| Age | 6-11 months | 99 | 27 |
| 12-23 months | 142 | 38.8 | |
| 24-59 months | 125 | 34.2 | |
| Sex | Male | 199 | 54.4 |
| Female | 167 | 45.6 | |
| Residence | Urban | 158 | 43.2 |
| Rural | 208 | 56.8 | |
| Breast feeding on admission | Yes | 119 | 32.5 |
| No | 247 | 67.5 | |
| Admission type | New admission | 290 | 79.2 |
| Re admission | 76 | 20.8 | |
| Referral status | Health center | 51 | 13.9 |
| Health post | 85 | 23.2 | |
| Outreach | 5 | 1.4 | |
| Self-referral | 225 | 61.5 | |
| Admission criteria | Only edema | 15 | 4.1 |
| Only wasting | 262 | 71.6 | |
| Both edema and wasting | 49 | 13.4 | |
| Only MUAC | 40 | 10.9 |
Table 1: Socio-demographic characteristic, admission type category, SAM category breast feeding and referral status of the record review of children 6-59 months at Fik primary hospital, Somali region, Ethiopia from January 2016 up to December 2019.
Medical comorbidity
All children admitted at the stabilizing center had at least one form of comorbidity. The most common medical comorbidities accompanied with SAM children at time of admission were pneumonia (56.8%) followed by diarrhea (41.8%), tuberculosis (TB) (17.5%), vomiting (16.7%) and anemia (15.1%). about the HIV status of the children were unknown. Regarding on the (TB) (17.5%), vomiting (16.7%) and anemia (15.1%). about the HIV status of the children were unknown. Regarding on the appetite almost (76.5%) had poor appetite based on standard SAM protocol (Table 2).
| Medical comorbidity | Category | Frequency | Percentage (%) |
|---|---|---|---|
| Pneumonia | Present | 208 | 56.8 |
| Absent | 158 | 43.2 | |
| Temperature | Fever (>37.5) | 39 | 10.7 |
| Hypothermia (<35) | 21 | 5.7 | |
| Normal | 306 | 83.6 | |
| Vomiting | Present | 61 | 16.7 |
| Absent | 305 | 83.3 | |
| Appetite at admission | Good | 86 | 23.5 |
| Poor | 280 | 76.5 | |
| Diarrhea | Present | 153 | 41.8 |
| Absent | 213 | 58.2 | |
| Type of diarrhea | Watery | 137 | 89.5 |
| Dysentery | 16 | 10.5 | |
| TB | Present | 64 | 17.5 |
| Absent | 302 | 82.5 | |
| HIV/AIDS | Present | 0 | 0 |
| Absent | 0 | 0 | |
| Unknown | 366 | 100 | |
| Anemia (pale conjunctiva and palmer pallor and/or a hemoglobin count of <11 g/dl | Present | 58 | 15.8 |
| Absent | 206 | 56.3 | |
| Un known | 102 | 27.9 | |
| Malaria | Present | 21 | 5.70% |
| Absent | 345 | 94.3 |
Table 2: Distribution of medical comorbidity information on record review of SAM children 6-59 months at Fik primary hospital, Somali region, from January 2016 up to December 2019.
Routine medication and treatment
Almost all (98.4%) admitted children were received IV antibiotics like ampicillin, gentamicin and ceftriaxone. 97.8%, 84.4% and 59.8% received amoxicillin, vitamin A and measles respectively. Additionally 78.7% of the reviewed records received folic acid. On the other hand 63.7% of the reviewed records received deworming either Albendazole or mebendazole, where the number of fully immunized children was less than one-third which was 27% of the records (Table 3).
| Treatment given | Category | Frequency | Percent (%) |
|---|---|---|---|
| IV fluid | Yes | 132 | 36.1 |
| No | 234 | 63.9 | |
| IV antibiotic | Yes | 360 | 98.4 |
| No | 6 | 1.6 | |
| Amoxicillin | Yes | 358 | 97.7 |
| No | 8 | 2.2 | |
| Vitamin A | Yes | 309 | 84.4 |
| No | 57 | 15.6 | |
| Deworming (Albendazole or Mebendazole) | Yes | 233 | 63.7 |
| No | 133 | 36.3 | |
| Measles | Yes | 219 | 59.8 |
| No | 110 | 30.1 | |
| Not applicable | 37 | 10.1 | |
| Folic acid | Yes | 288 | 78.7 |
| No | 78 | 21.3 | |
| Fully immunized | Fully Immunized | 99 | 27 |
| Partially Immunized | 229 | 62.6 | |
| Not started | 38 | 10.4 |
Table 3: Information of the treatment given on record review of SAM children 6-59 months at Fik primary hospital, Somali region, Ethiopia, from January 2016 up to December 2019.
Recovery rate from SAM
The 366 of SAM children admitted from January, 2016 up to December 2019, in the stabilization center of Fik primary hospital were reviewed. Overall proportion of recovery 289 (79%), death 32 (8.7%), defaulter 34 (9.3%) and medical transfer 11 (3%) were observed. The overall observed average length of stay was 9.05 days SD (5.41) (Table 4).
| Variable | Frequency | Percent (%) |
|---|---|---|
| Recovered | 289 | 79% |
| Not recovered | 77 | 21% |
Table 4: Recovery rate of reviewed records of SAM children admitted in Fik primary hospital from January 2016 to December 2019.
Survival function of the overall recovery rate indicates that; as time increases in hospitalization of the SAM children the recovery rate also increases.
Survival estimates for cure rate
Overall recovery rate of the reviewed records was 289 (79%) Kaplan-Meir survival curves were showed. Log-rank test were tested the significance of the observed difference. There is significantly different survival time among children with and without severe anemia (log-rank test, x2 20.65, p-value 0.000), Tuberculosis (TB) (log-rank test, x2: 19.62, p-value 0.000), provision of IV fluid (log-rank test, x2: 10.36, p-value 0.001),Vitamin A (log-rank Test, x2: 5.3, p-value 0.021) deworming (log-rank test, x2: 4.47, p- value 0.034), folic acid (logrank test, x2: 5.18 p-value 0.023) and finally children with age category of 12-23 months had higher mean survival time compared to children age 6-11 months with (log-rank test x2: 5.13, P-value 0.058) (Table 5).
| Variable | Chi-square | Df | P-value |
|---|---|---|---|
| Age category | 5.68 | 2 | 0.058 |
| Sex | 3.13 | 1 | 0.77 |
| Residence | 0.59 | 1 | 0.44 |
| BF on admission | 0 | 1 | 0.99 |
| Admission type | 2.69 | 1 | 0.1 |
| Referral type | 2.25 | 3 | 0.52 |
| Admission criteria | 3.1 | 3 | 0.37 |
| Pneumonia | 0.45 | 1 | 0.49 |
| Vomiting | 5.07 | 1 | 0.02 |
| Diarrhea | 0.95 | 1 | 0.32 |
| Type of diarrhea | 1.85 | 1 | 1.71 |
| TB | 19.24 | 1 | 0 |
| Malaria | 0.06 | 1 | 0.79 |
| Anemia | 20.4 | 1 | 0 |
| IV fluid | 10.9 | 1 | 0.001 |
| Antibiotic | 3.64 | 1 | 0.056 |
| Amoxicillin | 2.3 | 1 | 0.12 |
| Vitamin A | 5.305 | 1 | 0.021 |
| Deworming | 4.47 | 1 | 0.034 |
| Measles | 0,99 | 2 | 0.6 |
| Folic acid | 5.18 | 1 | 0.023 |
| Immunization status | 1.49 | 2 | 0.47 |
Table 5: Log-rank test table of recovery rate of SAM children admitted in Fik primary hospital from January 2016 to December 2019.
Kaplan-Meier recovery estimates for severely malnourished children with anemia and without anemia.
Kaplan-Meier recovery estimates for severely malnourished children with TB and without TB.
Kaplan-Meier recovery estimates for severely malnourished children With IV fluid given and without IV fluid.
The median survival time is 11.5 days (Table 6).
| Interval start time | Number entering interval | Number withdrawing during interval | Number exposed to risk | Number of terminal events | Proportion terminating | Proportion surviving | Cumulative proportion surviving at end of interval |
|---|---|---|---|---|---|---|---|
| 0 | 366 | 30 | 351 | 74 | 0.21 | 0.79 | 0.79 |
| 7 | 262 | 28 | 248 | 141 | 0.57 | 0.43 | 0.34 |
| 14 | 93 | 10 | 88 | 59 | 0.67 | 0.33 | 0.11 |
| 21 | 24 | 6 | 21 | 14 | 0.67 | 0.33 | 0.04 |
| 28 | 4 | 3 | 2.5 | 1 | 0.4 | 0.6 | 0.02 |
Table 6: Life table analysis of severe acute malnutrition children treated at Fik hospital stabilization center Somali region Ethiopia from January 2016 up to Dec 2019.
Factors associated with recovery rate of reviewed records from January 2016 up to December 2019 in Fik primary Hospital, Somali Region Ethiopia.
Bivariate cox regression analysis was run for the following independent variables, sex, age, residence type of malnutrition, breast feeding at admission, appetite at admission, medical comorbidities like pneumonia, diarrhea, malaria anemia, TB and routine medications like IV fluids, IV antibiotics, amoxicillin, vitamin a, measles, deworming and folic acid.
Bivariate analysis showed that age category of the child at admission 12-23 months (CHR; 1.358 95% CI: 1.003-1.839), 24-59 months (CHR; 1.333 95% CI (0.982-1.810), sex of the child (CHR; 1.207 95% CI: 0.955-1.525), residence (CHR: 0.923 95% CI: 0.730-1.165) breast feeding on admission (CHR: 1.015 95% CI: (0.790-1.304), appetite at admission (CHR: 0.801 95% CI: 0.613-1.047) Vomiting (CHR: 0.706 95% CI:0.499-0.997), Diarrhea (CHR; 0.904 95% CI:0.711-1.149), TB (CHR: 0.478 95% CI: 0.335-0.681), anemia (CHR: 0.451 95% CI: 0.310-0.655), malaria (CHR 1.060 95% CI: 0.657-1.711), IV fluid (CHR: 1.469 95% CI: 1.144-1.886), Vitamin A (CHR: 1.469 95% CI: 1.144-1.886), measles (CHR: 0.888 95% CI: 0.681-1.158), folic acid (CHR: 0.731 95% CI: 0.540-0.991), deworming (CHR: 0.788 95% CI: 0.617-1.007) were carried out in bivariate cox regression then; multivariable cox regression was carried out for variables verified as significant at p-value, <0.25 by bivariate cox regression [18].
Accordingly after adjusting different variables age between 24-59 months, tuberculosis, anemia and provision of IV fluid were found as independent predictors of recovery rate in severely malnourished children admitted to the hospital (Table 7).
| Variable | Category | Treatment Outcome | CHR( 95% CI ) | P- Value | |
|---|---|---|---|---|---|
| Recovery Frequency (%) | Not Recovery Frequency (%) | ||||
| Age Category | 6-11 months | 68 (18.5%) | 31(8.4%) | 1 | |
| 12-23 months | 114 (31.1%) | 28 (7.6%) | 1.358 (1.003-1.839) | 0.048 | |
| 24-59 months | 108 (29.5%) | 18 (4.9%) | 1.333 (0.982-1.810) | 0.065 | |
| Sex | Male | 163 (44.6%) | 36(9.8%) | 1 | |
| Female | 126 (34.4%) | 41 (11.2%) | 1.207 (0.955-1.525) | 0.116 | |
| Residence | Urban | 125 (34.2%) | 33 (9%) | 1 | |
| Rural | 164 (44.8%) | 44 (12%) | 0.923 (0.730-1.165) | 0.499 | |
| BF on admission | Yes | 90 (24.6%) | 29 (7.9%) | 1 | |
| No | 199 (54.4%) | 48 (13.1%) | 1.015 (0.790-1.304) | 0.907 | |
| Appetite at admission | Good | 72 (21.3%) | 8 (2.2%) | 1 | |
| Poor | 217 (64.2%) | 14 (12.3%) | 0.801 (0.613-1.047) | 0.104 | |
| Vomiting | Yes | 38 (10.4%) | 23 (6.2%) | 0.706 (0.499-0.997) | 0.048 |
| No | 251 (68.6%) | 54(14.8%) | 1 | ||
| Diarrhea | Yes | 38 (10.4%) | 23(6.3%) | 0.904 (0.711-1.149) | 0.41 |
| No | 251 (68.6%) | 54 (14.7%) | 1 | ||
| Tuberculosis(TB) | Yes | 35 (9.6%) | 29 (7.9%) | 0.478 (0.335-0.681) | 0 |
| No | 254 (69.4%) | 48 (13.1%) | 1 | ||
| Anemia | Yes | 32 (8.7%) | 26 (7.1%) | 0.451(0.310-0.655) | 0 |
| No | 257(70.2%) | 51(13.9%) | 1 | ||
| Malaria | Yes | 18(5%) | 3 (0.8%) | 1.060 (0.657-1.711) | 0.81 |
| No | 271(74%) | 74 (20.2%) | 1 | ||
| IV Fluid | Yes | 92 (25.2%) | 40 (10.9%) | 1 | |
| No | 197(53.8%) | 3437(10.1%) | 1.469 (1.144-1.886) | 0.003 | |
| Vitamin A | Yes | 275(75.1%) | -9.30% | 1 | |
| No | 38(10.4%) | 19(5.2%) | 0.682(0.470-0.990) | 0.044 | |
| Measles Vaccine | Yes | 183(50%) | 36(9.8%) | 1 | |
| No | 78(21.3%) | 32(8.7%) | 0.888(0.681-1.158) | 0.382 | |
| No Applicable | 28(7.7%) | 9(2.5%) | 0.947(0.632-1.420) | 0.792 | |
| Folic Acid | Yes | 237(64.8%) | 51(13.9%) | 1 | |
| No | 52(14.2%) | 26(7.1%) | 0.731(0.540-0.991) | 0.043 | |
| Deworming | Yes | 192(52.5%) | 41(11.2%) | 1 | |
| No | 97(26.5%) | 36(9.8%) | 0.788(0.617-1.01) | 0.057 | |
| Immunization status | Fully immunized | 89(24.3%) | 10(2.7%) | 1.119(0.731-1.714) | 0.604 |
| Partially immunized | 171(46.8%) | 58(15.8%) | 0.967(0.648-1.443) | 0.869 | |
| Not Immunized | 29(7.9%) | 9(2.5%) | 1 | ||
Table 7: Bivariate cox regression analysis of SAM children with 6-59 months at Fik primary hospital, Somali region, Ethiopia: From January 2016 up to December 2019.
Multivariate cox regression was carried out for variables verified as significance at P-value <0.25, consequently after adjusting the variables age between 24-59 months, Tuberculosis (TB), anemia and Intra Venous fluid (IV) administration were found to be independent predictor for recovery rate. Accordingly severely malnourished children those age from 24 months to 59 months had 2.8 times higher probability of recovery from SAM compared to 6-11 months old children (AHR=2.796 95% CI: 1.132-5.592). Similarly SAM children who were admitted without tuberculosis infection were 58% increased of recovery compared to those who had tuberculosis as comorbidity (AHR: 0.422 95% CI: 0.202-0.878). Likewise children who received IV fluids during rehabilitation were 50% more likely to recover compared to those who had not received IV fluid (AHR: 0.508; 95%CI; 0.322-0.802). SAM children who were not presented with anemia are 73% better to recover compared to those who had anemia with (AHR: 0.269; 95% CI: 0.116-0.621) (Table 8) [19,20].
| Variables | Category | Treatment outcome | CHR (95% CI) | AHR (95% CI) | |
|---|---|---|---|---|---|
| Recovered frequency (%) | Not recovered frequency (%) | ||||
| Age | 24-59 months | 108 (29.5%) | 18 (4.9%) | 1.34 (0.99-1.82) | 2.57 (1.19-5.55) |
| 6-11 months | 68 (18.5%) | 31 (8.4%) | 1 | 1 | |
| Sex | Male | 163 (44.6%) | 36 (9.8%) | 1 | 1 |
| Female | 126 (34.4%) | 41 (11.2%) | 1.207 (0.955-1.525) | 1.35 (0.97,1.45) | |
| Residence | Urban | 125 (34.2%) | 33 (9%) | 1 | 1 |
| Rural | 164 (44.8%) | 44 (12%) | 0.923 (0.730-1.165) | 0.97 (0.81, 1.42) | |
| BF on admission | Yes | 90 (24.6%) | 29 (7.9%) | 1 | 1 |
| No | 199 (54.4%) | 48 (13.1%) | 1.015 (0.790-1.304) | 1.35 (0.92, 1.54) | |
| Appetite at admission | Good | 72 (21.3%) | 8 (2.2%) | 1 | 1 |
| Poor | 217 (64.2%) | 14 (12.3%) | 0.801 (0.613-1.047) | 0.76 (0.43, 1.15) | |
| Vomiting | Yes | 38 (10.4%) | 23 (6.2%) | 0.706 (0.499-0.997) | 0.65 (0.31,1.09) |
| No | 251 (68.6%) | 54 (14.8%) | 1 | 1 | |
| Diarrhea | Yes | 38 (10.4%) | 23 (6.3%) | 0.904 (0.711-1.149) | 0.87 (0.72, 1.06) |
| No | 251 (68.6%) | 54 (14.7%) | 1 | 1 | |
| Tuberculosis(TB) | Yes | 35 (9.6%) | 29 (7.9%) | 0.478 (0.335-0.681) | 0.52 (0.28,1.03) |
| No | 254 (69.4%) | 48 (13.1%) | 1 | 1 | |
| Anemia | Yes | 32 (8.7%) | 26 (7.1%) | 2.288 (1.575-3.324) | 0.27 (0.12-0.62) |
| No | 257 (70.2%) | 51 (13.9%) | 1 | 1 | |
| IV Fluid | Yes | 92 (25.2%) | 40 (10.9%) | 1.463 (1.140-1.879) | 0.51 (0.32-0.80) |
| No | 197 (53.8%) | 37 (10.1%) | 1 | 1 | |
| Folic acid | Yes | 237 (64.8%) | 51 (13.9%) | 1 | 1 |
| No | 52 (14.2%) | 26 (7.1%) | 0.731 (0.540-0.991) | 0.84 (0.61, 1.15) | |
| Vitamin A | Yes | 275 (75.1%) | -9.30% | 1 | |
| No | 38 (10.4%) | 19(5.2%) | 0.682 (0.470-0.990) | 0.47 (0.27-1.14) | |
| Malaria | Yes | 18 (5%) | 3 (0.8%) | 1.060 (0.657-1.711) | 1.14 (0.62-1.89) |
| No | 271 (74%) | 74 (20.2%) | 1 | 1 | |
| Deworming | Yes | 192 (52.5%) | 41 (11.2%) | 1 | 1 |
| No | 97 (26.5%) | 36 (9.8%) | 0.788 (0.617-1.01) | 0.89 (0.73, 1.24) | |
| Measles Vaccine | Yes | 183 (50%) | 36 (9.8%) | 1 | 1 |
| No | 78 (21.3%) | 32 (8.7%) | 0.888 (0.681-1.158) | 0,92 (0.71, 131) | |
| No applicable | 28 (7.7%) | 9 (2.5%) | 0.947 (0.632-1.420) | 0.98 (0.68, 1.55) | |
| Immunization status | Fully immunized | 89 (24.3%) | 10 (2.7%) | 1.119 (0.731-1.714) | 1.38 (0.81, 1.56) |
| Partially immunized | 171 (46.8%) | 58 (15.8%) | 0.967 (0.648-1.443) | 0.76 (0.57, 1.32) | |
| Not Immunized | 29 (7.9%) | 9 (2.5%) | 1 | 1 | |
Table 8: Multivariate cox regression analysis of SAM children with 6-59 months at Fik primary hospital, Somali region, Ethiopia: From January 2016 up to December 2019.
The finding of this study revealed that overall recovery rate of the complicated SAM was 79% were the rests 21% end up with non-recovery (combination of defaulter, dead and medical transfer). The length of stay in the stabilization center was 10.3 days SD (± 5.567). This study this is in line with acceptable minimum standard and Ethiopian protocol for management of SAM which recommends children should stay in the stabilization center less than 28 days. In this study average weight gain of 10.4 g/kg/day has been recorded. This result is above the minimum weight gain of international sphere standard which is 8 g/kg/day.
This finding of 79% of recovery rate is above the minimum sphere standard and national SAM guideline protocol of 75%, it’s in line with study conducted in Debremarkos and Finote Salam hospitals and Wolaita zone hospitals. Lower than the findings of Jimma university specialized hospital of, Woldia hospital and Southern Ethiopia.
The finding of the study is above other studies conducted in Lacor Uganda which indicates recovery rate of 66.9%, the one in Diredawa Dilchora referral hospital 69.9% and Bahirdar Flege Hiwot referral hospital 58.4%. This difference could be due to differences of quality of care given to the patient, hospitals caseload, presence of updated SAM management guidelines in some facilities and staff knowledge and adherence of severe acute management protocol.
In the current study SAM children without Tuberculosis (TB) and anemia had significantly better recovery than their counterparts. Similarly children between the ages of 24-59 months had better recovery rate than those with age between 6-11 months and additionally Intravenous fluid (IV) intake had significant association with recovery rate.
The current study revealed that children with age of 24-59 months had 2.6 times more likely to recover compared to those children between 6-11 months (AHR 2.57 (95% CI: 1.19-5.54). this findings agrees with other study conducted at Ghana Tamale teaching hospital. but different from the study conducted Debremarkos and Finote selam hospitals which indicates children age from 24 to 35 months had 34% lower probability of recovery from SAM compared to 6–11 months old children. The difference of the findings may be due to difference of age groups who have been sampled or differences of feeding practice across the area.
In this study children who are without tuberculosis are 58% increased of recovery compared to those who had TB as comorbidity (AHR: 0.422 95% CI: 0.202-0.878), this finding is in line with other study conducted in Sekota whegamer zone, Southern Ethiopia and another study conducted in Northwest Ethiopia which indicate that children without TB comorbidity are 1.6 times better to recover compared to their counterparts. This may be as normally tuberculosis is immune suppressive the child may develop appetite loss and unable to feed the recommended daily diet or therapeutic milk which in turn can delay the recovery.
Anemia has showed statistically significant association with recovery rate, accordingly children who were not presented with anemia are 73% better to recover compared to those who had anemia with (AHR: 0.269; 95% CI: 0.116-0.621). The findings of this study are in line with the study conducted in Northwest Ethiopia, Woldiya hospital Sekota hospital Weghamer zone and Bahirdar Flege Hiwot referral hospital. Finally this study revealed that children who received IV fluids during rehabilitation are 50% more likely to recover compared to those who had not received (AHR: 0.508; 95% CI; 0.322-0.802).
the findings of this study agreed with other study conducted in Mekele city Ethiopia and Southern Ethiopia but this finding is contradict to other study conducted in Addis Ababa SPMMC and Lacor Northern Uganda which reveals I.V fluid infusion were associated with an increased risk of mortality this contradiction may be due to fluid overload or lack regular monitoring during infusion as a result of that it may contribute mortality.
The overall recovery and other outcome indicators were in the range of the minimum international standard. Mean weight gain and mean length of hospitalization were in the acceptable range of international standards.
In the current study SAM children without Tuberculosis (TB) and anemia had significantly better recovery than their counterparts. Similarly children between the ages of 24-59 months had better recovery rate than those with age between 6-11 months and finally IV intake had significant association with recovery rate.
Based on the above findings the following recommendations are forwarded to the hospital, Zonal health office and regional health bureau; Treatments of medical complications like tuberculosis and anemia needs to be focused.
Maternal care, optimal breast feeding and personal hygiene and sanitation sessions should be given to caretaker mothers and their visitors. All results of the investigations should be clearly documented in the patient card to prevent future incompleteness of the records.
Strong monitoring and evaluation of the program, ensuring sustained resource follow and timely provision of routine medications will have crucial roles in improving recovery rate and establishing an appropriate SAM management system in the hospital.
This study was conducted after obtaining ethical clearance from Institutional Health Research Ethics Review Committee (JJUIHRERC college of medicine and health sciences,) of Jigjiga university. In addition to this permission were obtained from Fik hospital administration (CEO) before conducting the study. As the study was conducted through a review of records, no consent was obtained from the mothers or caregivers of the study subjects. No personal identifiers to maintain confidentiality of the information and privacy during data collection.
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Ibrahim AM, Kalif FA, Muse AI, Osman MO, Ahmed AT, Wedajo GT, et al. (2023) Recovery Rate and Associated Factors of Children Aged 6-59 Months Admitted with Severe Acute Malnutrition at Inpatient Unit of Fik Primary Hospital, Somali Region Ethiopia. Gynecol Obstet. 13:603.
Received: 10-Mar-2023, Manuscript No. GOCR-23-22117; Editor assigned: 13-Mar-2023, Pre QC No. GOCR-23-22117 (PQ); Reviewed: 27-Mar-2023, QC No. GOCR-23-22117; Revised: 17-May-2023, Manuscript No. GOCR-23-22117 (R); Published: 24-May-2023 , DOI: 10.35248/2161-0932.23.13.603
Copyright: © 2023 Ibrahim AM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.