Journal of Hematology & Thromboembolic Diseases
Open Access
ISSN: 2329-8790
ISSN: 2329-8790
Research - (2022)Volume 10, Issue 7
Red blood cell transfusion in oncohematological patients is considered an essential part of treatment, but its role in palliative care that aims to improve symptoms and quality of life is not well established. The aim of this study was to evaluate the evolution of symptoms after red blood cell transfusion in palliative care patients. Thirteen patients were followed at an outpatient blood transfusion clinic at the University of Campinas. Data was collected on the Palliative Performance Scale (PPS) as well as the characteristics of the patients, the oncohematological diagnosis, the stage of the disease, and clinical symptoms that justified transfusion. To analyze the evolution of symptoms and functional capacity, the Edmonton Symptom Assessment Scale (ESAS) and the Katz Index Functional Assessment Scale for basic activities of daily living were applied serially on the day of transfusion, as well as two and seven days after the procedure. We also observed the occurrence of transfusion reactions. We were able to identify improvements in symptoms such as fatigue, depression, drowsiness, as well as overall well-being in most patients up to seven days after transfusion. However, patients with seven days or more of transfusion maintained improvement only in fatigue. Similarly, other studies report an improvement in symptoms such as weakness, fatigue, and overall well-being after transfusion, this improvement also being transient and lasting less than 14 days.
Blood transfusion; Anemia; Palliative care; Fatigue; Tiredness
Anemia, defined as hemoglobin below 12 g/dl according to criteria of the World Health Organization, is a prevalent finding in cancer patients. In palliative care units, its frequency is approximately 70%, being the most common hematologic manifestation in these patients [1,2]. In the oncological context, anemia has a multifactorial etiology whose main mechanism is the decrease in erythroid production in the bone marrow. The causes of this hypoproliferative anemia in cancer patients are diverse. In cases of anemia caused by inflammation or chronic disease, there is an increase in inflammatory cytokines, especially Interleukin-6 (IL-6), which interferes with iron homeostasis with greater hepcidin production and decreased erythropoietin synthesis. Furthermore, direct infiltration of the bone marrow by the neoplasm can occur with decreased production of normal hematopoietic cells, such as erythroid precursors, which is frequently observed in hematological neoplasms and tumors of solid metastatic organs, such as breast, prostate, and renal carcinoma [3]. Other mechanisms occur due to iron deficiency, such as chronic bleeding, which occurs mainly in tumors of the gynecological and gastrointestinal tract, nutritional anemia due to anorexia and decreased food intake, and finally as a consequence of cancer treatment itself, due to myelotoxicity of chemotherapy and radiotherapy [3]. The clinical manifestations of anemia include symptoms such as dyspnea, fatigue, drowsiness, and malaise, severely reducing the quality of life of these patients and limiting their daily activities [1]. With the progressive aging of the population, we have observed an increase in the prevalence of cancer and chronic diseases. Despite advances in medicine, we still deal with therapeutic limitations and with patients without the means to get proper treatment. In this context, palliative care is based on prevention and relief of suffering in patients who face life-threatening diseases, focusing on the treatment of symptoms and the improvement of life quality [4,5].
Furthermore, it rejects the introduction or maintenance of therapies considered futile, that is, those that are unable to modify the natural course of the disease and do not aim to promote the patient's well-being [5]. Thus, the value of blood transfusion as a supportive treatment in hematological and oncological diseases is well established and is seen as an essential part of treatment. However, its role in relieving symptoms in oncohematological patients in palliative care units still needs to be consolidated [2]. For patients with advanced cancer, a conservative transfusion strategy is generally used, restricting transfusion to those who are symptomatic and with hemoglobin levels generally less than or equal to 8 g/dl2. However, there are few studies that evaluate the real benefit of transfusion in relieving symptoms such as tiredness and dyspnea, as well as in the general improvement of wellbeing in patients under palliative care. These symptoms may be related to anemia, but are multifactorial in cancer patients, making it difficult to assess the impact of red blood cell transfusion on symptom relief and its true benefit [2]. However, the deleterious effects associated with blood transfusion are well established. Transfusion reactions can range from mild to serious events. Possible immediate transfusion reactions are: Transfusion-Associated Circulatory Overload (TACO), acute lung injury, transfusionassociated sepsis, and hemolytic reaction due to ABO incompatibility [6,7].
In the palliative care population, the risk of TACO should be considered. TACO is characterized by the appearance of cardiogenic pulmonary edema caused by the infusion of a blood component. Prospective and retrospective hemovigilance analyzes report incidence of TACO in 1% to 6% of transfused patients, with an estimated mortality of up to 10% [8,9]. The risk factors are advanced age, low weight, hypoalbuminemia and impaired renal function, such characteristics that are frequently observed in oncohematological patients in palliative care [8,9].
Thus, the use of blood transfusion in advanced disease may be associated with reduced survival rates, with mortality rates ranging from 13% to 33% in patients with up to 15 days after red blood cell transfusion [1]. However, this most likely reflects the advanced stage of the disease, rather than establishes a causeand- effect relationship. The scientific literature on the risks and benefits of blood transfusion in the palliative care population is limited, leaving unanswered a number of questions regarding transfusion practices in palliative patients [10].
In this context, the decision to recommend transfusion in these patients is a complex ethical decision. On the one hand, we must establish therapies that alleviate symptoms and provide comfort, valuing the patient's well-being. On the other hand, we must avoid treatments that bring harm or prove futile or disproportionate to the stage of the disease. We must also consider that blood transfusion is a high-cost therapy and that the pressure to maintain adequate stocks of blood components has been growing [1,6,7,10].
As an aggravating factor, the criteria used to indicate blood transfusion in these patients, the effect of transfusion on symptoms and quality of life, and the frequency of adverse events in this population are not well established [10].
In addition, the benefits observed in clinical patients who receiveda transfusion cannot simply be extrapolated to oncohematological patients in palliative care, due to the disease burden, cachexia, functional status, and side effects of already performed treatments. Thus, we still do not have definitive evidence of the effect (benefit or harm) of this treatment in palliative care [7,10,11]. The aim of this study was to evaluate the evolution of symptoms after red blood cell transfusion in palliative care patients.
This is an observational study that included 13 patients in palliative care diagnosed with oncohematological diseases who were admitted to the University of Campinas Blood Transfusion Service between February and April 2021. Patients with hematological malignancies in palliative care who had an indication for packed red blood cell transfusion as assessed by the hematologist were included. All patients signed an informed consent form (FICF) and the inclusion of the patient in the study did not interfere with the institution's treatment proposal. The present study was approved by the UNICAMP Ethics and Research Committee (CAE 30497220.8.0000.5404).
Data such as age, sex, Body Mass Index (BMI) were collected, as well as information on diagnosis, stage of the disease, number of units transfused, and pretransfusion hemoglobin level. In addition, the physical condition of the patients was assessed before the red blood cell transfusion using the Palliative Performance Scale (PPS). This tool has been validated in a population of palliative care in Canada and provides a percentage score that determines the estimated survival rate for the next three months. It consists of six subjective parameters resulting from the evaluation of the patient's walking, activity capacity, evidence of illness, self-care, food intake, and level of consciousness [12].
To assess the possible effects of packed red blood cell transfusions on the evolution of symptoms and the capacity for daily activities, the Edmonton Symptom Assessment Scale (ESAS) and the Katz index functional assessment scale of basic activities of daily living were applied three times: Before transfusion (D0), two days after transfusion (D2) and seven days after transfusion (D7). For patients who were unable to return for re-evaluation 2 or 7 days after transfusion, the information was collected by telephone contact.
The Edmonton Symptom Assessment Scale (ESAS) was developed in the palliative care unit of Edmonton General Hospital in Canada for use in the daily assessment of symptoms of patients in palliative care. This tool addresses nine physical and psychological symptoms such as pain, fatigue, nausea, drowsiness, appetite, and shortness of breath, in addition to depression, anxiety, and wellbeing [13]. The Katz index is one of the oldest tools to assess activities of daily living, being described in 1963 [13]. It is a questionnaire that addresses six functions and daily activities such as feeding, continence, transference (locomotion), toileting, dressing, and bathing. All patients were under observation for 30 minutes after transfusion to monitor possible adverse effects.
Thirteen patients were recruited during the study period. The mean age was 62 years, ranged from 45 to 84 years; 7 patients were women and 6 were men. The pretransfusion hemoglobin level ranged from 5.8 g/dl to 8 g/dl with a median of 6.8 g/dl and the anemia-related symptoms reported by the patients were fatigue and tiredness (Table 1).
| Patient | Age | Sex | BMI | Diagnoses | PPS | Pre -transfusion hemoglobin value (g/dl) |
|---|---|---|---|---|---|---|
| 1 | 83 | F | 20 | Secondary AML/ MDS | 60 | 7.3 |
| 2 | 78 | F | 21 | Chronic lymphocytic leukemia | 80 | 7.2 |
| 3 | 61 | F | 19 | Myelodysplastic syndrome + cholangiocarcinoma | 80 | 7.1 |
| 4 | 73 | M | 23 | Myelodysplastic syndrome | 90 | 8.0 |
| 5 | 53 | M | 23 | Multiple myeloma | 80 | 6.0 |
| 6 | 50 | F | 21 | Secondary AML/Primary myelofibrosis | 70 | 5.9 |
| 7 | 62 | M | 25 | Primary myelofibrosis | 90 | 6.9 |
| 8 | 59 | F | 16 | AML | 90 | 6.4 |
| 9 | 84 | M | 18 | Primary myelofibrosis | 50 | 6.8 |
| 10 | 81 | F | 12 | Multiple myeloma | 60 | 6.6 |
| 11 | 54 | F | 18 | Chronic myeloid leukemia in blast crisis | 70 | 5.8 |
| 12 | 83 | M | 25 | Secondary AML/MDS | 60 | 6.4 |
| 13 | 45 | M | 25 | Secondary AML/MDS | 70 | 7.0 |
Table 1: Demographics and clinical characteristics.
All components of the transfused blood were leukocyte reduced and irradiated. None of the patients had an adverse reaction during or 24 hours after transfusion. As a result, the evaluation of symptoms using the ESAS scale recorded before transfusion and reported 2 days after transfusion showed improvements in fatigue, depression, well-being and sleepiness in most patients (69.2%, 53.8%, 53.8%, 46.2%, respectively), as shown in Figure 1 below.
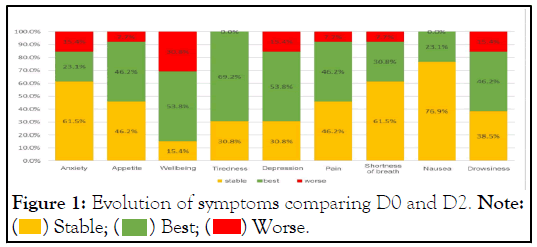
Figure 1: Evolution of symptoms comparing D0 and D2. Note:  Stable;
Stable;  Best;
Best;  Worse.
Worse.
In addition, pain and appetite also improved in a significant portion of the patients (46.2%), but the same number of patients kept these symptoms stable within 2 days. For symptoms of nausea, anxiety, and shortness of breath, most patients remained stable (76.9%, 61.5% and 61.5%, respectively) when comparing D0 (before transfusion) and D2.
Similarly, when evaluating the evolution of these symptoms in D2 and D7, we observed that most patients remained stable in terms of anxiety, appetite, and depression, and pain, shortness of breath, nausea, and drowsiness. On the other hand, we observed that there was a deterioration of the sensation of wellbeing in most patients (53.8%) when comparing the evolution from D2 to D7. Regarding fatigue, 38.5% of the patients reported improvement in this period and 38.5% reported worsening, and the remaining 23% remained stable with the symptom during this period (Figure 2).
Figure 2: Evolution of symptoms comparing D2 and D7. Note:  Stable;
Stable;  Best;
Best;  Worse.
Worse.
There was no improvement in functional levels after RBC transfusion using the Katz index functional assessment scale of basic activities of daily living (Figure 3).
Figure 3: Evolution of symptoms comparing D0 and D7.Note:  Stable;
Stable;  Best;
Best;  Worse.
Worse.
Asthenia and fatigue are frequent complaints in cancer patients. However, its etiology may be related to anemia, which is commonly observed in this group of patients, but also occurs as a result of tumor burden and toxicity of chemotherapy treatment1 [10-15]. Thus, it will always be difficult to determine how much anemia contributes to the occurrence of these symptoms. Other studies have already shown similar results with improvement in weakness, dyspnea, and well-being after transfusion of packed red blood cells in patients under palliative care. This effect appears to be transient, lasting less than 14 days [1,2,7].
In addition, patients whose main indication for transfusion was fatigue and asthenia, such as the patients in the present study, seem to be those with the greatest benefit [1,2,7]. On the other hand, other factors can influence physicians in the decision to prescribe blood transfusion, such as pressure from family members or other health professionals, in addition to the hemoglobin level alone, regardless of the presence of anemia symptoms [15]. The benefit of red blood cell transfusion is less evident in this context.
Previous studies suggest that the estimated rate of patient survival and the degree to which patient's body functions are preserved seem to be associated with the degree of improvement [1]. In this sense, patients with better functionality and with higher PPS are expected to have a greater improvement in symptoms after transfusion. However, these studies were conducted in a small number of patients and without casecontrol, which does not allow us to make this correlation. Nonetheless, it should be noted that the patients analyzed here had a PPS greater than 50%, which is consistent with this hypothesis.
It is important to consider that the group of patients analyzed was small, with different oncohematological diagnoses and at different stages of the disease, which certainly influences the intensity of tiredness and well-being. Therefore, it is not possible to define in the present study whether the evolution of symptoms was mainly influenced by the diagnosis and stage of the disease or the effect of blood transfusion.
As discussed in similar studies, it is still not possible to define predictive factors of response in improving symptoms after red blood cell transfusion in cancer palliative care patients [1]. The principal limitation of this study is that on the same day blood transfusion was performed; patients underwent routine outpatient return to the institution, evaluated in a medical and nursing consultation. Therefore, other interventions such as adjustment of medications and adequacy of analgesia, in addition to other nonpharmacological treatments, may have contributed to the improvement of symptoms. The improvement in pain and appetite seen in the first two days after transfusion may be related in part to this. In addition to that, it is not possible to exclude a placebo effect associated with transfusion, i.e, based on the patient’s belief in the benefits of blood transfusion and its fortifying effect [2,6].
Other studies reported similar results with no change in functionality after blood transfusion of packed red blood cells [16]. Regarding adverse effects related to transfusion, despite the fact that patients had risk factors for the occurrence of TACO; no immediate transfusion reaction was observed. Certainly, the adequacy of the transfusion volume and infusion speed with the patient's weight, in addition to constant clinical evaluation during transfusion, contributed to reducing this risk. Additionally, all transfused blood components were leukocytefree. Finally, it is important to consider that transfusion implies the need for patients to visit a health service and spend hours in care, which in itself can cause discomfort and decrease quality of life [15-17].
RBC transfusion can improve the subjective perception of symptoms of fatigue, sleepiness, and well-being related to a drop in hemoglobin. However, the only symptom that maintained a perception of improvement after 7 days was fatigue. Furthermore, we observed that although most patients reported improvements in well-being 2 days after transfusion, this did not sustain after 7 days, which makes us conclude that this perception of improvement is transient. Therefore, we consider that the decision to prescribe packed red blood cell blood transfusion in palliative care oncohematological patients should be made on a case-by-case basis, taking into account the presence and degree of symptoms related to anemia, the physical condition of these patients, the expected survival time, and the perception of improvement of symptoms reported by the patient. More studies are needed to better define the role of blood transfusion in this context and to assess possible predictors of response to improve symptoms.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Magnus MM, Lacativa JCL, Assumpção JA (2022) Red Blood Cell Transfusion in Palliative Care Patients with Oncohematological Disease. J Hematol Thrombo Dis.10.505.
Received: 17-Oct-2022, Manuscript No. JHTD-22-19679; Editor assigned: 21-Oct-2022, Pre QC No. JHTD-22-19679 (PQ); Reviewed: 04-Nov-2022, QC No. JHTD-22-19679 ; Revised: 11-Nov-2022, Manuscript No. JHTD-22-19679 (R); Published: 18-Nov-2022 , DOI: 10.35248/2329-8790.22.10.505
Copyright: © 2022 Magnus MM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.