Autism-Open Access
Open Access
ISSN: 2165-7890
ISSN: 2165-7890
Research Article - (2024)Volume 14, Issue 4
Background: Unlike other neurological disorders, there are no such supporting examinations that can definitively diagnose Autism Spectrum Disorder (ASD). The ASD presents a wide range of symptoms with variations that can indicate the severity of the condition, making its identification more complex and leading to potential misdiagnosis, missed diagnosis or delayed diagnosis.
Materials and methods: This study aims to ensure the precise diagnosis of ASD, distinguish it from other conditions, so it could provide comprehensive management to achieve optimal outcomes. This study is part of a larger research on ASD and its relationship with serotonin and brain-derived neurotrophic factors. Recruitment and diagnostic screening were conducted from May to June 2023 at the Neurobehavior Pediatric Center (NBPC), Bandung, based on the arrival of patients who registered directly at NBPC and through online registration. All patients were assessed with identical procedures, with a Childhood Autism Rating Scale (CARS) and through careful observation directly, followed by re-evaluation using video. The data will be presented in descriptive form.
Results: Of the 150 registered patients, 49 children were diagnosed other than autism. Dyslexia became the most common diagnosis after re-evaluation, present in 30.6% of the subjects. This was followed by intellectual disability (26.5%) and Expressive Language Disorders (ELD)+Risk of Dyslexia (RD) (22.4%). Additionally, there were other diagnoses such as ELD, ERLD, giftedness, Seckel syndrome, Cerebral Palsy (CP) and borderline Intelligence Quotient (IQ).
Conclusion: It requires extensive and repeated observational studies conducted over sufficient time, as well as a thorough understanding of neurodevelopmental disorders, executive function and theory of mind. Additionally, using multiple assessment tools is essential.
Autism spectrum disorder; Diagnosis; Re-evaluation; Previously diagnosed; Neurobehaviour
Autism Spectrum Disorder (ASD) is a neurodevelopmental disorder characterized by deficits in social communication and the presence of restricted interests and repetitive behaviors [1]. The Diagnostic and Statistical Manual of Mental Disorders-5th edition (DSM-5) updated the diagnostic criteria for ASD from the previous 4th edition (DSM-4), in 2013. In DSM-5, the concept of a spectrum ASD diagnosis was created, combining the DSM-4s separate Pervasive Developmental Disorder (PDD) diagnoses such as autistic disorder, Asperger’s disorder, childhood disintegrative disorder and Pervasive Developmental Disorder Not Otherwise Specified (PDDNOS), into one. Rett syndrome is no longer included under ASD in DSM-5 as it is considered a discrete neurological disorder [2].
Unlike other neurological disorders, such as epilepsy syndrome or autoimmune anti-n-methyl-d-aspartate receptor encephalitis, which have laboratory support and other diagnostic tools to establish a definitive diagnosis, there are no such supporting examinations that can definitively diagnose ASD. The ASD presents a wide range of symptoms with variations that can indicate the severity of the condition, making its identification more complex and leading to potential misdiagnosis, missed diagnosis or delayed diagnosis. The symptoms of ASD can overlap with, be overshadowed by or mimic other similar conditions. Increased general awareness of ASD has led to more attention to the condition. Diagnosing ASD requires careful observation of the symptoms and behaviors of a child suspected of having ASD due largely to wide variations in symptom types and severity and their alterations with age [3,4].
The clinical heterogeneity of ASD is at least partially due to high comorbidity with other mental disorders. The comorbidity with other psychiatric conditions might be over-represented among patients with mild ASD compared to those with severe forms, with lifetime estimates overlapping disorders in this subgroup ranging from 70% to about 80%. For example, gifted children are frequently diagnosed with ASD due to similar behaviors, such as low social skills and restricted interests in specific topics. Clinicians and pediatricians who are not trained to assess the unique emotional difficulties of gifted children often make diagnostic errors. Many intellectual students are diagnosed as having autism and many children with autism are not diagnosed as exceptional. Misdiagnosis in the assessment of autism has consequences for behavior and clinical therapy, rendering them ineffective. Parents, clinicians and teachers should be familiar with concepts such as twice-exceptional, dyslexia and Attention Deficit Hyperactivity Disorder (ADHD) [5-7]. Through this study, we aim to underline the importance of an accurate diagnosis of ASD and misdiagnosis of ASD but not diagnosed as ASD, so that appropriate comprehensive management can be provided to achieve optimal results.
This study is part of a larger research on ASD and its relationship with serotonin and brain-derived neurotrophic factors. Recruitment and diagnostic screening were conducted from May to June 2023 at the Neurobehavior Pediatric Center (NBPC), Bandung. Patient recruitment was based on the arrival of patients who registered directly at NBPC and through online registration. The criteria of the patients are 3-10 years old when the evaluation begins in NBPC and have been diagnosed with ASD previously. The guardians always sign a written informed consent during the first visit and allow the application of their children’s data for research purposes. All patients were assessed with identical procedures by the clinical staff, composed of one trainee in neuropediatric and Pediatric Neurology (PN) consultant with 25 years of experience in neurobehavioral pediatrics. The screening was conducted through careful observation directly, followed by re-evaluation using video. Clinical judgment by experienced clinicians is considered to be the gold standard for autism diagnosis. Standardized tools for the diagnosis of ASD using Childhood Autism Rating Scale (CARS). It is a widely used assessment tool to evaluate the severity of autism symptoms in children. The CARS score is based on a 15-item scale that assesses social interaction, communication and repetitive behaviors. The CARS provides a comprehensive evaluation of the child’s overall autism symptoms and helps for the diagnosis and monitoring of the condition [8,9]. The data will be presented in descriptive form.
Of the 150 registered patients, 49 children were diagnosed other than autism, of these 29 registered online and 20 came directly to NBP center. The average age of the 49 subjects who were diagnosed other than autism is 6.1 years, with the majority (53.1%) aged between 6 and 10 years old, and the remaining (46.9%) aged between 3 and 5 years old. The gender distribution indicates a greater proportion of males (67.3%) than females (32.7%).
When reviewing the re-diagnosis results, there is significant variation in diagnoses. Dyslexia became the most common diagnosis after re-evaluation, present in 30.6% of the subjects. This was followed by intellectual disability (26.5%) and Generalized Brain Edema (GBE)+Risk of Dyslexia (RD) (22.4%). Additionally, there were other diagnoses such as Generalized Brain Edema (GBE), GBER, exceptional ability, Seckel syndrome, Cerebral Palsy (CP) and borderline IQ (Table 1).
| Variable | n=49 |
|---|---|
| Dyslexia | 15 (30.6) |
| Intellectual disability | 13 (26.5) |
| Expressive language disorders+Risk to dyslexia | 11 (22.4) |
| Expressive language disorders | 4 (8.2) |
| Expressive language disorders+Responsive | 1 (2.0) |
| Gifted | 1 (2.0) |
| Seckel syndrome | 1 (2.0) |
| Cerebral palsy | 2 (4.1) |
| Borderline Intelligence Quotient (IQ) | 1 (2.0) |
Table 1: Diagnosis of 49 children previously suspected of having Autism Spectrum Disorder (ASD).
Table 2, presents the distribution of re-diagnosis results in children with ASD based on age and gender. The prevalence of dyslexia tends to be higher in children aged 6-10 years (46.2%) compared to other age group. Overall, the number of females diagnosed with dyslexia (37.5%) is slightly higher than the number of males (27.3%). There is no difference in the distribution of intellectual disability between the two age groups and the proportion between males and females. The prevalence of expressive language disorders+risk of dyslexia is higher in children aged 3-5 years (34.8%) compared to children aged 6-10 years (11.5%), the number of males is higher than females. Figure 1, presents the results in a bar chart, allowing us to see the distribution more clearly. In our records, patients previously diagnosed with autism were not only identified by medical professionals such as pediatricians or general practitioners, but also by parents who relied on internet information, books, journals, discussions with other parents, teachers, psychologists or therapists.
| Variable (Diagnosis, n(%)) | Age | Gender | ||
|---|---|---|---|---|
| 3-5 years (n=23) | 6-10 years (n=26) | Boy (n=33) | Girl | |
| Dyslexia | 3 (13.0) | 12 (46.2) | 9 (27.3) | 6 (37.5) |
| Intellectual disability | 6 (26.1) | 7 (26.9) | 9 (27.3) | 4 (25.0) |
| Expressive language disorders+Risk for dyslexia | 8 (34.8) | 3 (11.5) | 8 (24.2) | 3 (18.8) |
| Expressive language disorders | 3 (13.0) | 1 (3.8) | 4 (12.1) | 0 (0.0) |
| Expressive and receptive language disorders | 1 (4.3) | 0 (0.0) | 1 (3.0) | 0 (0.0) |
| Gifted | 0 (0.0) | 1 (3.8) | 0 (0.0) | 1 (6.3) |
| Seckel syndrome | 0 (0.0) | 1 (3.8) | 1 (3.0) | 0 (0.0) |
| Cerebral palsy | 1 (4.3) | 1 (3.8) | 1 (3.0) | 1 (6.3) |
| Borderline Intelligence Quotient (IQ) | 1 (4.3) | 0 (0.0) | 0 (0.0) | 1 (6.3) |
Table 2: Distribution of re-diagnosis results in children with Autism Spectrum Disorder (ASD) based on age and gender.
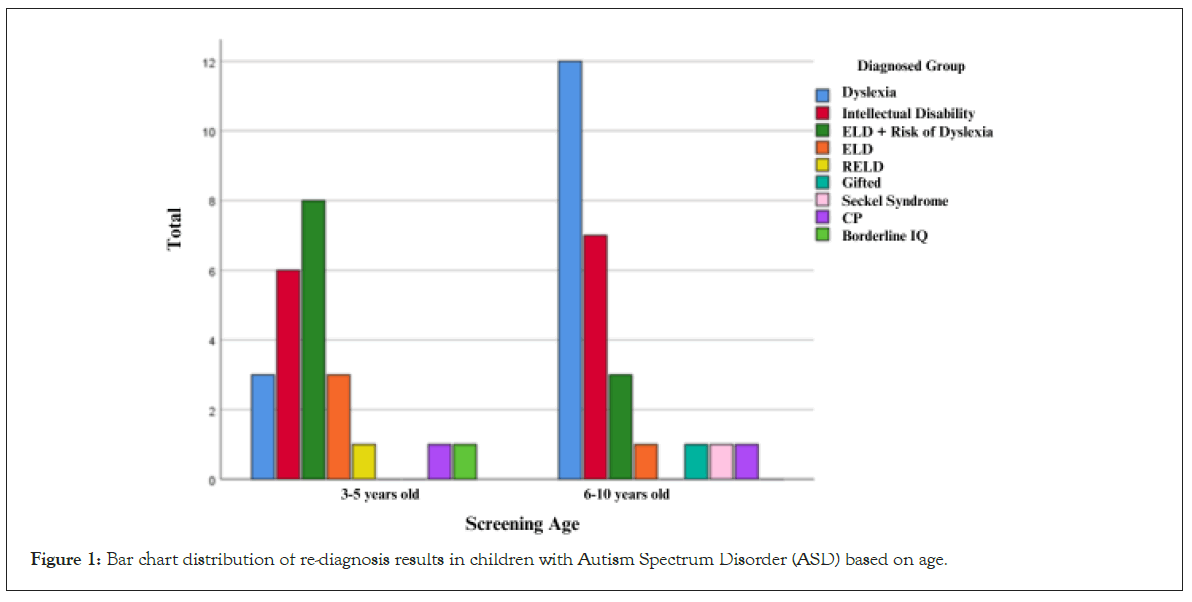
Figure 1: Bar chart distribution of re-diagnosis results in children with Autism Spectrum Disorder (ASD) based on age.
This study aims to ensure the precise diagnosis of ASD, distinguish it from other conditions and provide comprehensive management to achieve optimal outcomes. Based on DSM-5, provides specific criteria for diagnosing ASD, with the outline of the following:
• Persistent deficits in social communication and social interaction across multiple contexts.
• Restricted, repetitive patterns of behavior, interests or activities, as manifested at least two of the following stereotyped or repetitive motor movements, insistence on sameness, inflexible adherence to routines or ritualized patterns of verbal or nonverbal behavior, a highly restricted or fixated interest that abnormal in the intensity of focus, hyper or hyporeactivity to sensory input or unusual interest in sensory aspects of the environment.
• Symptoms must be present in the early development period.
• Symptoms cause clinically significant impairment in social, occupational or other important areas of current functioning.
• These disturbances are not better explained by intellectual disability or global developmental delay. Intellectual disability and ASD frequently co-occur; to make comorbid diagnoses of ASD and intellectual disability, although nowadays we have another classification low function and high function autism.
In our study, dyslexia are predominant in the re-diagnosis of patients previously diagnosed with ASD, due to there are many behaviors caused by dysfunctional executive function in dyslexia. Although there is no ubiquitous agreed definition of executive function, it can be described broadly as a set of higher-order cognitive control processes that enable purposeful behavior, required to achieve a known goal [10-13].
Dyslexia is often associated with rigidity, which may contribute to difficulties in learning and processing information and sometimes missed diagnosis or misdiagnosis. In particular, dyslexics frequently struggle with short-term memory and visual processing, they may experience dysfunction in the cerebellum, impacting their task management and ability to adapt to changing situations, which can lead to rigidity in behavior and challenges in spelling and fluency [11-13]. Their lack of ability in a language area, their rigidity and their association with ADHD sometimes lead to persistent deficits in social communication and social interaction such as ASD. Although repetitive behavior is not a primary characteristic of dyslexia, some individuals with dyslexia may exhibit repetitive behaviors as part of their overall cognitive and behavioral profile, this includes repetitive movements such as hand or finger movements or repetitive speech patterns, sometimes to cope with their frustration to anxiety related to language [14,15].
The second result is Intellectual Disability (ID). The definition of intellectual disability has evolved over the past century, with consensus in the scientific and practice communities around a framework that includes significantly lower-than-average cognitive functioning (intellectual capacity) and challenges in everyday activities in the home, school, community and employment environment (adaptive behavior). The link between intellectual capacity and adaptive behavior is complex [16]. The American Association on Intellectual and Developmental Disabilities (AAIDD) provided a widely recognized definition, intellectual disability is characterized by significant intellectual functioning and the conceptual, social and practical skills that make up adaptive behavior during the developmental period [17].
The association between autism, IQ and adaptive functioning has been probed in recent epidemiological and prospective cohort studies. Children with ASD drawn from the general population have lower adaptive skills relative to their IQ scores; moreover, lower adaptive scores are associated with a magnitude of early social impairment. Some symptoms of ID and ASD are similar, particularly in difficulties with communication, social interaction and repetitive behaviors, making it challenging to diagnose and distinguish between the two conditions accurately. Significant limitations in intellectual functioning and adaptive behaviors limit the ability to perform daily tasks that cause prominent communication and behavioral challenges [18,19]. Individual differences in early cognitive abilities are the putative tools with which to navigate novel life information, adapt flexibly in changing environments and judge well [20]. The implications are that individuals with intellectual disability who suffer from deficits in social skills are likely to have difficulty interpreting social signals in their interactions, moreover, they may experience problems regulating their emotions when interacting with their peers.
Language plays an important role in mediating cognitive tasks, establishing social roles and achieving social goals, highlighting the importance of interaction in the development of language itself as a critical component of social interaction. Individuals with expressive language disorders may struggle to communicate effectively, leading to social isolation and difficulties in forming and maintaining relationships [21,22].
Executive functions are a set of cognitive skills (moderately correlated components in confirmatory factor analysis) essential for updating ongoing information in working memory while monitoring task execution (updating); inhibiting unnecessary or irrelevant information (inhibition); efficiently shifting between mental sets (shifting). Crucially, later abilities rely on previously acquired skills and may significantly affect complex behaviors, such as those required for efficient communicative exchanges [23,24]. In our study, participants aged 3 to 10 years were at a stage where expressive language plays a vital role in socialization, particularly in speaking. This aligns with 2020 research on preschool children, which found that children with developmental language disorders often struggle to maintain sustained attention on verbal and nonverbal tasks in phonological working memory. This ability is necessary for the updating component of executive functions, as well as for tasks assessing inhibitory control and cognitive flexibility.
Individuals who are gifted typically have high cognitive ability, much has been written about the social-emotional vulnerability of high IQ individuals, with some scholars holding that highly gifted students experience social skill difficulties that are misdiagnosed as other disorders such as ASD. Gifted children sometimes being overlooked due to their giftedness, actually, in a comprehensive review, gifted children are more at-risk for adjustment problems than their non-intellectual peers and intellectualness increases a child’s vulnerability to adjustment difficulties. They are at greater risk for emotional and social problems, particularly during adolescence and adulthood. The hypothesis is that the intellectual are more sensitive to interpersonal conflicts and experience greater degrees of alienation and stress than do their peers as a result of their cognitive capacities [25,26].
The literature review, based on a cross-sectional approach, provides a more coherent overview of clinical observations and empirical study results. It summarizes that verbal skills, extended vocabulary, heterogeneous Wechsler Intelligence Scale for Children scores, attention problems, atypical sensory modulation, emotion regulation impairments, high prevalence of left-handedness, greater involvement of right-handedness and disharmonious developmental trajectories are similarities between children with ASD and those who are intellectual or have high intellectual potential. While full-scale IQ and social adaptive skills are generally better in intellectual children, the severity of autistic symptomatology is often less pronounced and does not persist for a lifetime. Due to these similar symptoms, some intellectual children are misdiagnosed, leading to significant consequences [26,27]. In our study, only one intellectual child was diagnosed with ASD, which may be attributed to our recruitment method, as we waited for participants to arrive at the NBPC.
We also identified other diagnoses, such as cerebral palsy and Seckel syndrome, which are mostly associated with intellectual disability related to syndromic conditions and cerebral palsy. Given the heterogeneity of its causes, the global frequency of intellectual disability in syndromic children varies greatly. The literature provides a concise analysis of gene ontology and suggests using transcriptional profiling to prioritize candidate genes. Research indicates that the prevalence of intellectual disability among individuals with cerebral palsy in the United States is less than 20%. In Indonesia, accurate data on the prevalence of intellectual disability are not available [28,29].
Diagnosing ASD is not simply a matter of referring to the DSM-5 or relying solely on the CARS assessment. It requires extensive and repeated observational studies conducted over sufficient time, as well as a thorough understanding of neurodevelopmental disorders, executive function and theory of mind. Additionally, using multiple assessment tools are essential. Many patients are diagnosed with ASD not only by specialized neuropediatricians but also by parents who gather information from the internet, readings, and discussions with other parents, teachers, therapists or pediatricians.
The first limitation is the number of participants, as we only recruited those who registered at NBP centers and had limited time for recruitment. The second limitation is that we solely used the CARS tool, alongside expert opinion, to determine whether patients had ASD. It would have been beneficial to use additional tools, such as ADOS, for a more comprehensive assessment.
This study was funded by Padjadjaran Univeristy and Hasan Sadikin General Hospital of Bandung, West Java, Indonesia.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Solek P, Nurfitri E, Prasetya T, Rizqiamuti AF, Sahril I, Burhan A, et al. (2024). Re-diagnosis of Previously Diagnosed Autism Spectrum Disorders in Neurobehaviour Pediatric Center, Bandung. Autism-Open Access. 14:412
Received: 02-Sep-2024, Manuscript No. AUO-24-32998; Editor assigned: 04-Sep-2024, Pre QC No. AUO-24-32998 (PQ); Reviewed: 18-Sep-2024, QC No. AUO-24-32998; Revised: 25-Sep-2024, Manuscript No. AUO-24-32998 (R); Published: 03-Oct-2024 , DOI: 10.35248/2165-7890.24.14.412
Copyright: © 2024 Solek P, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.