Clinical Pediatrics: Open Access
Open Access
ISSN: 2572-0775
ISSN: 2572-0775
Case Report - (2024)Volume 9, Issue 6
Objective: The purpose of this study was to analyze a case of recurrent atypical odontoma after surgical resection, in order to provide some references for the etiology analysis and treatment of this disease.
Methods: The detailed clinical data and history of related clinical symptoms of this patient were retrieved at first visit. Intraoral examination showed permanent dentition, no left maxillary first premolar (tooth 24). However, there were several anomalous tooth-like tissues in the affected area. Imaging studies showed several small, highly dense image aggregates above tooth 24. The erupting and un-erupting teeth-like tissues were removed in accordance with the surgical method of extraction of supernumerary teeth under local anesthesia. The patient was returned to our clinic one month later, and periapical radiography examination showed irregular and unorganized radiopaque mass surrounded by a clear thin radiographic halo above the crown of tooth 24. The imaging data indicated that this was a typical manifestation of odontoma. After full communication with the child's parents, the second surgical resection was performed to remove the cyst wall and the hard tissue inside the capsule.
Results: When the patient returned 3 months after the second operation, the intraoral examination showed tooth 24 had erupted normally, and periapical radiography examination showed no abnormal root development.
Conclusion: The case gives us three inspirations: Atypical odontoma is easy to cause misdiagnosis and lead to incomplete resection and postoperative recurrence; Intraoperative stimulation can promote the rapid growth of odontoma. Young permanent teeth can erupt normally after removing mechanical blockages without special treatment.
Atypical odontoma; Recurrence; Case report
Odontoma is a relatively common benign odontogenic tumor derived from odontogenic epithelium and odontogenic ectodermal mesenchymal tissue. It is formed by the abnormal development and hyperplasia of one or more dental embryonic tissues [1]. The tumor growth is slow and self-limiting. When the size is small, there are no symptoms in the early stage, most of which are accidentally found during the pre-orthodontic X-ray examination. If the tumor is large, it will appear as local painless hard mass. The general morphology of odontomas was basically the same whether they were curving tomography or Computed Tomography (CT) examination: The tumor body was located in the jaw, and the tumors were mostly round or quasi-circular, with less irregularity. The most characteristic imaging findings are a clear thin radiation band at the edge of the tumor enveloping a large number of immature teeth or undentated calcified masses with uniform or uneven density [2,3]. Because odontoma has typical imaging features, it is not easy to be confused with other odontogenic tumors in clinical practice, and accurate diagnosis can be made in most cases. However, it is worth considering whether the correct diagnosis and treatment can still be made for the atypical odontoma without definite fibrous tissue envelope and with abnormal multi-dentate tissue exposed in the mouth.
In this article, we summarized and analyzed a case of atypical odontoma that recurred after extraction due to misdiagnosis as "supernumerary tooth ". Through the discussion of this case, we can expand the diagnostic thinking of this kind of disease, and then provide certain reference for the definite diagnosis and thorough resection of odontoma.
A 12-year-old female patient in apparent well health presented to our pediatric department for absence of eruption of left maxillary first premolar(tooth 24)as reason of consultation. All procedures of this study were carried out in accordance with relevant guidelines and approved by Lianyungang Affiliated Hospital of Xuzhou Medical University/Lianyungang First People's Hospital (Grant number: LW-2024050701-01). Informed consent forms were assigned by the patient's parents before she were enrolled in the research. And the written informed consent for publication of identifying images or other personal or clinical details was obtained from the patient's parents.
The intraoral examination revealed permanent dentition, no left maxillary first premolar. However, there are several anomalous tooth-like tissues in the affected area. CBCT radiography findings showed several small, highly dense image aggregates above the un-erupted left maxillary first premolar (Figure 1). According to the clinical visual observation and imaging data, the preliminary diagnosis was supernumerary teeth. Under local anesthesia, we performed extraction according to the standard of supernumerary teeth. Before sutures, we did a periapical radiography control and the postoperative imaging examination indicated that the irregular teeth had been completely removed (Figure 2).
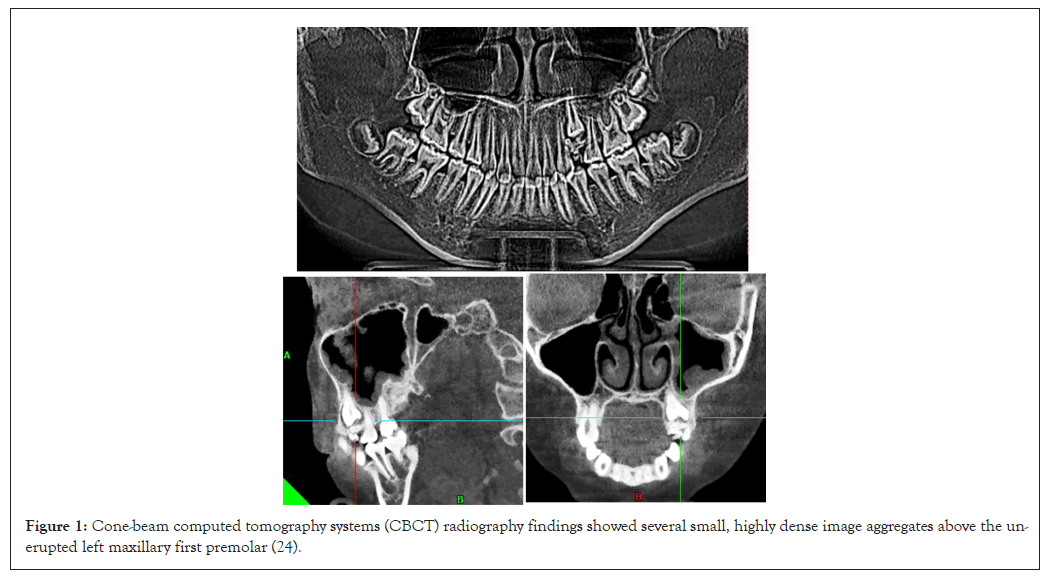
Figure 1: Cone-beam computed tomography systems (CBCT) radiography findings showed several small, highly dense image aggregates above the un-erupted left maxillary first premolar (24).
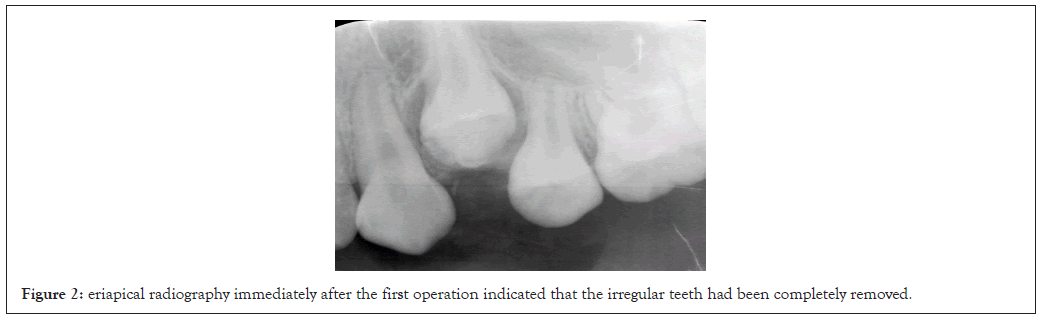
Figure 2: eriapical radiography immediately after the first operation indicated that the irregular teeth had been completely removed.
The patient was returned to our clinic one month later, and periapical radiography examination showed mixed radio-opaque and radiolucent lesion above the crown of 24 surrounded by a thin radiolucent band (Figure 3). The imaging data indicated that this was a typical manifestation of odontoma. After full communication with the child's parents, we started the eviction surgery surgical resection of the odontoma. We tried to undertake a minimally invasive surgical removal under local anesthesia. After bone eviction, we were able to remove the odontoma and found that the tumor was made up of seven small tooth-like structures. Same thing before the sutures, we did an X-ray control and the postoperative periapical radiography indicated that no mixed radio-opaque and radiolucent lesion above the crown region of tooth 24 (Figure 4). The patient was returned to the clinic one month later, and imaging showed no abnormal odontoma-like tissue above the crown region of tooth 24 (Figure 5). The patient was revisited three months after the second operation, and intraoral examination showed that the tooth 24 had erupted normally, while the imaging data indicated there was no obvious abnormality in tooth root development (Figure 6).
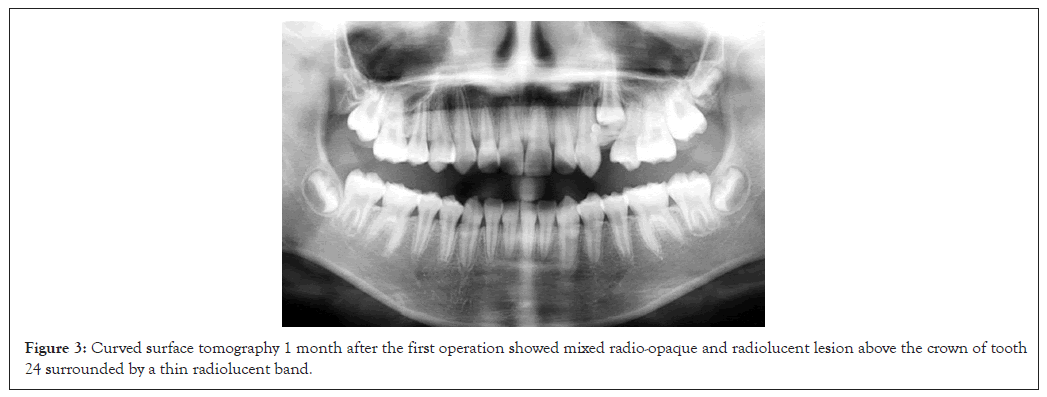
Figure 3: Curved surface tomography 1 month after the first operation showed mixed radio-opaque and radiolucent lesion above the crown of tooth 24 surrounded by a thin radiolucent band.
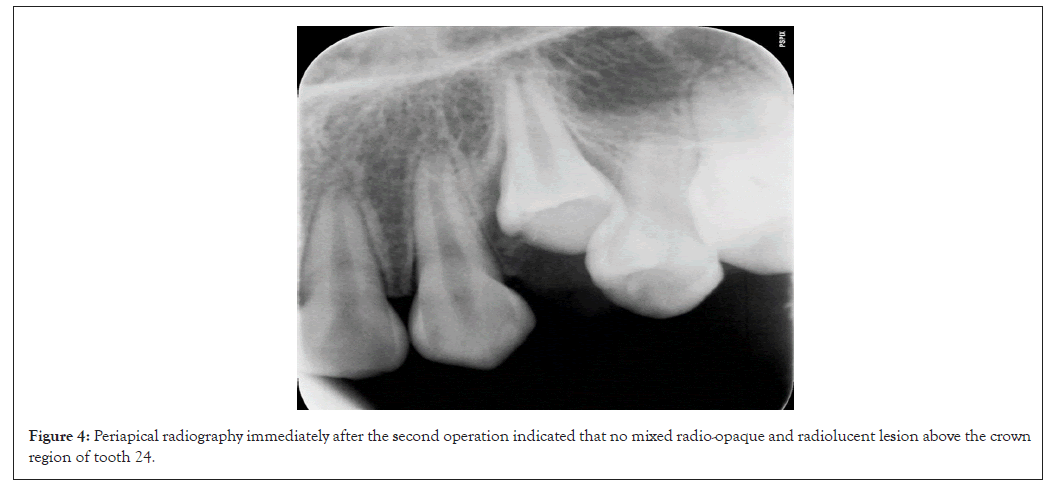
Figure 4: Periapical radiography immediately after the second operation indicated that no mixed radio-opaque and radiolucent lesion above the crown region of tooth 24.
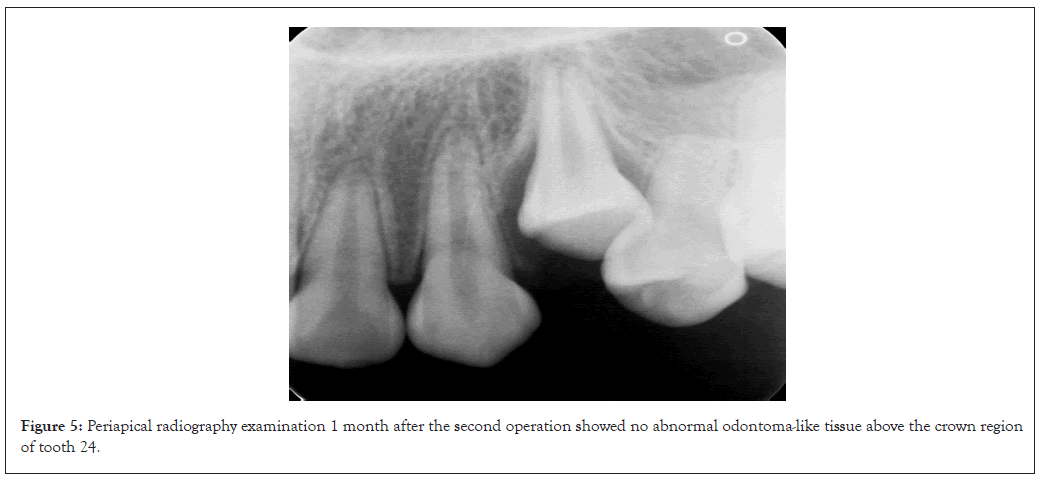
Figure 5: Periapical radiography examination 1 month after the second operation showed no abnormal odontoma-like tissue above the crown region of tooth 24.
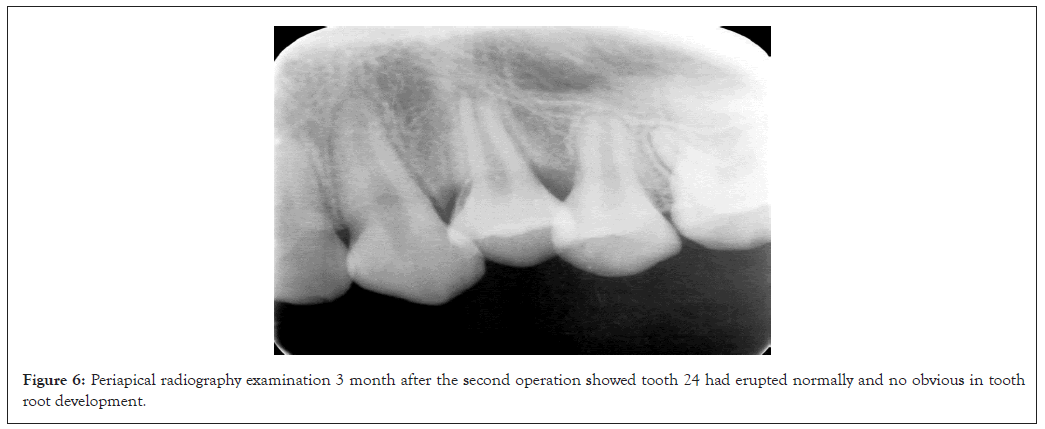
Figure 6: Periapical radiography examination 3 month after the second operation showed tooth 24 had erupted normally and no obvious in tooth root development.
Because odontoma has typical radiographic features, mainly presenting as irregular, unorganized radiopaque mass, usually surrounded by a clear thin radiographic halo, it is easy to make a definite diagnosis in the clinic [4,5]. However, once the dent-like tissue within the odontoma erupts out of the mouth, although this is very rare, it is difficult to establish a correct clinical diagnosis [6]. This article reports a rare case of atypical odontoma with the above characteristics. At the patient's first visit to our clinic, intraoral examination and imaging findings revealed multiple teeth with abnormal morphology located above the crown of the un-erupted tooth 24. However, one month after the removal of the excess teeth, a rapidly growing mass appeared in the alveolar bone, with typical odontoma characteristics. Eruption of impacted teeth will not occur until the second operation, after the obstruction has been removed according to odontoma surgical standards. For this rare case, we will analyze from several aspects, including how to make a correct diagnosis, the cause of rapid tumor growth, and the standard treatment of impacted teeth, in order to provide some references for the diagnosis and treatment of this rare odontoma with teeth eruption.
How to make a correct diagnosis of odontoma with teeth eruption?
The odontoma was mostly enclosed in the alveolar bone, most of the affected parts of the gingiva and alveolar bone showed no obvious abnormality or only slight eminence during clinical oral examination. However, because odontomas show distinct features on imaging, a correct diagnosis can usually be made by routine X-ray or CT examination [7,8]. Not everything is normal, there will always be accidents. If the odontoma is atypical and does not show typical odontoma features in oral and imaging examinations, how we can make a correct diagnosis is the focus of this paper [9]. For the cases reported in this paper, we took it for granted that they were supernumerary teeth due to the presence of multiple malformed teeth and no obvious odontoma structure on oral and radiographic examination. We reflect on mistakes made in early diagnosis.
First, there are cognitive deficits. Our understanding of odontomas rests on images of the typical odontoma form, the fibrous capsule wall surrounding the dentate tissue. Once the odontoma appears in an atypical form, we cannot make a correct diagnosis. Therefore, this is also the original intention of our case report. We hope that the reflection on this case can expand the clinician's cognition of atypical odontoma, so as to make better diagnosis and treatment for patients.
Second, careless observation deprives us of the opportunity to correct the erroneous diagnosis. When we re-examined the earlier Cone-beam computed tomography systems (CBCT) images, we found that on the crown of the un-erupted tooth, apart from several teeth with abnormal morphology that were removed, we could also see some other occluded image coverage. In addition, the post-operative periapical radiography examination after the first extraction of the redundant tooth also showed mixed radio-opaque and radiolucent lesion above the crown of un-erupted tooth. Although preoperative and postoperative imaging does not show the typical characteristics of odontoma, if we look closely, we will find that there is still unremoved tissue after the removal of the redundant tooth. Had we been aware of this at the time and consulted a more experienced professional, a second operation might have been avoided.
Why does the odontoma grow rapidly one month after the first operation?
In this misdiagnosed case, we stumbled upon a meaningful phenomenon. One month after the removal of the exposed odontoid tissue, the odontoma developed rapidly and presented a typical odontoma-like appearance on imaging. On this issue, we conducted a literature review and reached the following conclusions.
First of all, we need to analyze the etiology of odontoma. Odontomas are developmental abnormalities caused by the interaction of epithelial cells and mesenchymal tissue, which appear as regular or irregular masses of hard tissue surrounded by a fibrous tissue envelope [10,11]. The specific causes of odontoma still unclear, and there are several theories, including primary dentition trauma, infection, family history, genetic mutations, and overactivity of odontoblast cells [12]. For the cases reported in this paper, we speculated that it may be the trauma during the first extraction of redundant teeth, or the postoperative infection stimulated the odontoma capsule wall, which aggravated the abnormal epithelial and mesenchymal response and stimulated the rapid growth of odontoma lesions.
In addition, at the second surgical resection, we found that even after the odontoma had been removed, there were many smaller fibrous capsule walls hidden around the alveolar bone wall. This is similar to the recurrence of myxocysts caused by incomplete cleaning of vesicles after excision [13]. These potential fibrous capsule walls are also important factors for the recurrence of odontoma. Another point that cannot be ignored, the external stimulation during the first operation and the postoperative infection accelerated its growth rate, making it grow into a larger odontoma in just one month.
All this reminds us that when performing odontoma removal, thorough detoxification should be carried out to remove all exposed fibrocystic walls, and gentle movements should be performed to reduce adverse intraoperative and postoperative irritation, so as to reduce the possibility of odontoma recurrence.
What do we need to do about unerupted tooth due to odontoma?
Odontoma is more common in young patients, and the reason for visiting the doctor is that the permanent teeth do not erupt normally [14,15]. Therefore, for these patients, the normal eruption of permanent teeth is their focus. We know that the most common clinical tooth eruption disorder is mechanical impaction except for the unexplained primary eruption disorder, and odontoma is an important cause. For tooth eruption disorders caused by mechanical impact, most of the clinical treatments are to remove the mechanical obstacles, teeth can normally erupt without special treatment [16]. In the case reported here, the patient came to the clinic because tooth 24 failed to erupt normally. Since clear obstacles can be seen above the crown of the un-erupted tooth, we first take the way to observe the eruption of the tooth after removing the obstacles. However, due to the wrong diagnosis at the first visit, we only removed the abnormal tooth above the un-erupted crown, and failed to completely remove the obstacle on the crown side, resulting in the impacted tooth still unable to erupt.
After fully analyzing the cause and communicating with the patient and her parents, we carried out the second operation very carefully. During the second operation procedure, we considered in detail the factors that might affect the eruption of permanent teeth. In addition to the condition of not damaging the normal development of permanent tooth embryo, the surrounding fiber capsule wall is removed as far as possible. At the same time, a more gentle approach is taken during the operation to prevent recurrence caused by mechanical trauma to the hidden cyst wall and postoperative infection. The results of the second surgery were satisfactory. The un-erupted teeth had erupted normally, and the crown and root development were not abnormal. This case is further described that young permanent teeth affected by odontoma can grow back normally without further treatment as long as the coronary odontoma is removed [17]. Of course, further orthodontic treatment may be required in the future if the dentition is to be made neat and aesthetically pleasing.
In this paper, the possible causes of recurrent odontoma after operation were analyzed, and the following conclusions were drawn. Not all odontomas are standard fibrous capsular walls surrounding hard tooth tissue. Some odontomas may appear as the eruption of deformed teeth. During the operation, remove all the capsule walls as far as possible without damaging the unerupted teeth, and ensure that the action is gentle. Young impacted teeth have strong eruptive power and can erupt spontaneously after removing crown resistance.
The data presented in this study are available on reasonable request from the corresponding author.
Han Qin, Yong-qing Gong: designed the research study. Han Qin: performed the research. Han Qin, Yong-qing Gong: analyzed the data. Han Qin: wrote the manuscript. Both authors read and approved the final manuscript.
All procedures of this study were carried out in accordance with relevant guidelines and approved by Lianyungang Affiliated Hospital of Xuzhou Medical University/Lianyungang First People's Hospital (Grant number: LW-2024050701-01). Informed consent forms were assigned by the patient's parents before she were enrolled in the research.
This research was funded by the 521 Scientific Research Project of Lianyungang City (Grant number: LYG 06521202362); Xuzhou Medical University Affiliated Hospital Development Fund Support Project (Grant number: XYFM202457).
The authors are grateful to the patient and her family members for their kind cooperation and participation.
The authors declare no conflict of interest.
The written informed consent for publication of identifying images or other personal or clinical details was obtained from the patient's parents.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Qin H, Gong Y (2024). Reflections on Postoperative Recurrence of Atypical Odontoma: A Case Report. Clin Pediatr. 09:281.
Received: 21-Oct-2024, Manuscript No. CPOA-24-34997; Editor assigned: 24-Oct-2024, Pre QC No. CPOA-24-34997 (PQ); Reviewed: 07-Nov-2024, QC No. CPOA-24-34997; Revised: 14-Nov-2024, Manuscript No. CPOA-24-34997 (R); Published: 21-Nov-2024 , DOI: 10.35248/2572-0775.24.09.281
Copyright: © 2024 Qin H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.