Journal of Alcoholism & Drug Dependence
Open Access
ISSN: 2329-6488
ISSN: 2329-6488
Case Report - (2022)Volume 10, Issue 5
Obsessive Compulsive Disorder (OCD) is a chronic disabling psychiatric illness with a lifetime prevalence of 1-3 percent. Comorbidity with Substance Use Disorder may complicate the clinical picture to lead to more severe OCD symptoms. In this report, we present a case of a young woman who started using alcohol as self-medication for her OCD and rapidly achieved Alcohol Dependence. She presented with alcohol withdrawal seizure which was erroneously diagnosed as Seizure disorder leading to challenges in overall management.
Refractory OCD; OCD with Substance use; Comorbidities with OCD
Obsessive Compulsive Disorder is a fourth most common psychiatric illness and a leading cause of disability in functioning and quality of life [1]. Despite the introduction of various evidence based treatment guidelines for treatment of OCD majority of adults with OCD do not achieve remission. Up to 49% treated patients continued to experience clinically significant symptoms in a 10 year follow study of treatment outcomes in OCD [2].
Drug resistant OCD has been defined as less than 25% reduction in Yale-Brown Obsessive Compulsive Scale (YBOCS) to at least 2 sequential Selective serotonin reuptake inhibitors (SSRIs) and Clomipramine given for trial duration of 12 weeks [3]. A variety of augmentation treatment options have been tried and promulgated for use in such patients. However, the level of evidence for use of such treatment options is low and is based on limited research evidence.
Furthermore, the course of illness is likely to be complicated by co-morbid psychiatric disorders. It has been reported that up to a quarter of patients who seek treatment for OCD suffer from Substance Use Disorder (SUD) and majority have Alcohol Use Disorders. Patients with SUD comorbid with OCD present with more severe OCD symptoms, poorer insight regarding OCD, poorer quality of life and greater impairment in overall psychosocial functioning than participants without SUD [4]. Self-medication hypothesis of substance use in OCD states that although ineffective some patients may use alcohol as a way of coping with the anxiety associated with their symptoms [5].
Very few studies have studied the clinical correlates of SUDs in a clinical sample of OCD thereby hampering the improvement in available treatment options. Nonetheless, these patients are at increased risk of suicidality thereby deserving special attention [6]. Most guidelines are silent regarding treatment options in patients with comorbid OCD and SUD.
Here, we present the case of a young woman who started using alcohol as self-medication for her OCD and rapidly developed Alcohol Dependence Syndrome. Data regarding prevalence of Alcohol Dependence Syndrome in Indian women is very scarce. Rates of alcohol use in Indian women have been variously reported to be low (less than 5%) but even lower depending upon the region of country studied, social, cultural and religious factors [7-9]. This indirectly indicates that Alcohol Dependence in Indian women is rare making this case unique thereby posing a diagnostic and treatment challenge.
39 year-old female, home maker was first brought to psychiatry Out Patient Department (OPD) in 2017. She had a 4-year history of repeated obsessions of household things being dirty cleaning and washing them during major part of her daily routine. For past one year she had decline in social interaction with irritability towards family members. Her general physical and systemic examination was normal.
Relevant laboratory investigations were normal. Mental Status Exam (MSE) revealed anxious affect with disturbed sleep and appetite. Her YBOCS score was 28/40 suggestive of severe illness. She was diagnosed as a case of Obsessive and Compulsive Disorder and started on Fluoxetine, built up to 80 mg per day in divided doses over 12 weeks. She was also given psychoeducation and exposure and response prevention, but had suboptimal response to treatment. In view of poor response, she was switched to Clomipramine 225 mg but she continued to experience significant distress and dysfunction due to her symptoms over next four months. She was lost to follow up thereafter. After a gap of 03 years, she was brought to emergency department with history of 02 episodes of seizures. She had features of autonomic hyperactivity in the form of tachycardia, tremors, profuse sweating. She was evaluated by neurologist initially and her Electroencephalogram (EEG) and Magnetic Resonance Imaging (MRI) brain were normal. She was diagnosed as a case of seizure disorder and started on antiepileptic drugs. She was referred for psychiatric evaluation in view of past history of OCD. Patient disclosed history of surreptitiously consuming increasing amounts of alcohol over the last 05 years. She apparently felt a temporary reduction in her anxiety with alcohol and had better sleep. She had gradually increased the amounts consumed daily due to perceived reduced effects with previously consumed amounts. Her intake further increased after she felt that medications were not helping her and she perceived that there was no cure to her illness. She had temporarily felt tremors and excessive sweating when she did not consume alcohol and improvement in these symptoms after consuming alcohol. She was unable to abstain from alcohol due to strong urge even though it caused marked impairment in her social relations with family members.
She persisted to have distressing OCD. Her treatment was then optimized with addition of Aripiprazole 15 mg with which she reported gradual reduction in her symptoms. She had achieved abstinence from alcohol during this period and her interpersonal relations had improved. In her subsequent follow ups, she was in remission and was abstinent from alcohol (Figure 1) .
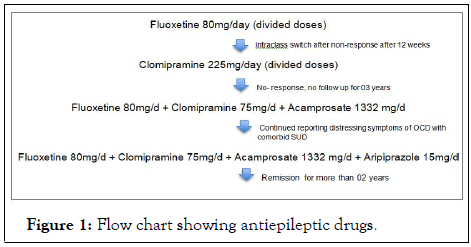
Figure 1: Flow chart showing antiepileptic drugs.
Patient was reassured and was given a dual diagnosis of OCD with Alcohol Dependence Syndrome. Antiepileptic drugs were gradually tapered off and stopped. Fluoxetine 80 mg/day was reinstituted and added on Tab Clomipramine 75 mg/day. Concurrently, she was given Acamprosate as an anticraving agent. She was also psychotherapy and cognitive behavior therapy. Self-medication of alcohol in OCD may complicate the clinical picture and add to treatment resistance. Additionally, this may impact social relationships of the individual. The index case presented various challenges for the treating team (Table 1).
| Challenges in index case |
|---|
| Alcohol considered a taboo in social and cultural background for a female |
| High expressed emotions, criticism and hostility of family members |
| Social isolation by family members |
| Non adherence to OCD treatment due to alcohol use |
| Alcohol withdrawal seizures erroneously diagnosed as seizure disorder |
Table 1: The index case presented various challenges.
She had poor response to initial SSRI treatment which could have been due to complex interaction between alcohol and psychotropics. She was managed with concurrent targeting of her OCD and Alcohol Dependence Syndrome. She was treated aggressively for her OCD with combination of Fluoxetine with Clomipramine in maximum therapeutic doses for OCD. She was given Cognitive Behavioral Therapy (CBT) and Family Therapy to address high expressed emotions and include family members in the treatment. Drug non-response was tackled by augmentation with Second Generation Antipsychotic (Aripiprazole) with which she achieved remission. She was psychoeducated about relapsing nature of her both the illness and how one might affect the outcome of other.
This case specifies the self-medication hypothesis of substance use in OCD. It further highlights the need for clinicians to be aware of this possibility and actively seek and assess for features of substance use disorders in such patients who conventionally may not be consuming alcohol. It has been proposed in the past that addressing OCD will help in treatment of SUD. However, concurrently addressing OCD and SUD is likely to have maximal benefit for the patient. Thus, it can be concluded that SUD can complicate the clinical picture of OCD with implications on treatment and outcome. Active addressal of both psychiatric co-morbidities simultaneously is recommended for better outcome.
Citation: Singh J, Dangi A, Chauhan VS, Yadav AS (2022) Refractory OCD Complicated by Alcohol Withdrawal Seizures: A Case Report. J Alcohol Drug Depend. 10:368.
Received: 22-Aug-2022, Manuscript No. JALDD-22-17127 ; Editor assigned: 24-Aug-2022, Pre QC No. JALDD-22-17127 (PQ); Reviewed: 07-Sep-2022, QC No. JALDD-22-17127 ; Revised: 13-Sep-2022, Manuscript No. JALDD-22-17127 (R); Published: 22-Sep-2022 , DOI: 10.35248/2329-6488.22.10.368
Copyright: © 2022 Singh J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.