Pediatrics & Therapeutics
Open Access
ISSN: 2161-0665
ISSN: 2161-0665
Research Article - (2022)Volume 12, Issue 2
Background: The nutritional status of under-five children is an important marker of child health in a nation. Malnutrition accounts for significant morbidity and mortality among under-fives, globally. Low income countries like Nigeria are the worst hit. A few researches on family function revealed that key components of family function allow a conducive environment for the development of mental and psychological well-being of under-five children. Despite the vastness of literature available on malnutrition, information is scarce on the role family function plays on nutritional status of under-fives. This was the reason for undertaking this study.
Aim/Objective: To determine the nutritional status of under-five children and its relationship with family function with a view to making recommendations to improve their nutritional status. To achieve this aim, this study determined the prevalence of malnutrition, family dysfunction, the pattern of family function and the relationship between family function and nutritional status of under-five children.
Materials and methods: This was a hospital based cross-sectional analytical study, carried out in the under-five clinic of Federal Medical Centre, Bida. Sample size was determined using the formula and found to be 230. Systematic random sampling was used for the selection of subjects. Anthropometric measurements were taken and matched to their corresponding Z-scores using the World Health Organization reference values to determine weight for age, weight for height, height for age, and weight/height Z-scores. Interviewer administered questionnaires were also used to retrieve data from their mothers to determine their family function.
Results: In this study of 230 under-five children, the prevalence of underweight undernutrition was 27.4%; wasting and stunting undernutrition were 27.8% and 23.5% respectively while overweight/obesity overnutrition was 4.8% (specifically overweight was 2.2% and obesity was 2.6%). When considered as cut-offs for public health significance, the prevalence of under nutrition fell under high prevalence while overweight/obesity fell under low prevalence. The prevalence of family dysfunction in this study was 2.18% moderate dysfunction was 43.91% while highly functional was 53.91%. The mean family function score was 7.5 ± 2.1. On the perception of family function by mothers, satisfaction was highest with the resolve component (62%) and lowest with adaptation (48.7%).
The result also showed that high family function was associated with lower rates of underweight (12.6%) and stunting (10.9%) malnutrition but was associated with higher rates of wasting (16.1%) and overweight/obesity (4.4%). Also, moderate family dysfunction was associated with lower rates of wasting (10.9%) and overweight (0.4%) malnutrition as well as higher rates of underweight and stunting. Family dysfunction was only associated with wasting (0.9%). However, these associations were not statistically significant.
Conclusion: Although these associations were not statistically significant, the result suggested the need for primary care physicians to determine family function when caring for malnourished under-five children.
Family Dysfunction; Malnutrition; Nutrition
The nutritional status of under-five children has become a topical issue of great concern to the nations of the world and is an important health index [1]. Malnutrition is accountable for significant morbidity and mortality among under-fives especially in Low Income Countries (LICs) and Medium Income Countries (MICs) such as Nigeria. It accounts for 2.5 million cases of severe acute malnutrition among under-fives in Nigeria, 420,000 annual deaths of under-fives in Nigeria alone and over 11 million cases of stunting [2-5]. The under-fives (ages 0 to 59 months) are a very vulnerable population whose nutritional status are determined by the form of care they receive [6]. Literature subsists of the various determinants of under-five nutrition but they are scarce on the effect their family function may have on their nutritional status [7]. The various forms of malnutrition (underweight, wasting, stunting and overweight) seen among under-five children can only be detected by conscientiously assessing the nutritional status of this vulnerable group [8-10].
The family is the basic unit of the society where the vulnerable under-five population receive nurture, nutrition and care as they take their place in the world [11]. Family dysfunction is any condition that interferes with healthy family functioning, although families may have some periods of time where functioning is impaired by stressful occurrences, healthy families tend to return to normal functioning after the crisis passes. In dysfunctional families, however, problems tend to be chronic and children fail to consistently get their needs met while in the long run, negative patterns of parental behaviour tend to be dominant in their children's lives [12]. Under-five malnutrition is one of the key health indicators of a nation and up till now the documented diseases that have been studied in association with family dysfunction were none of the recognized health indicators by the Sustainable Development Goals (SDG), this underscored the relevance of this study [13].
The World Health Organization (WHO) emphasized that malnutrition among under-fives was of major public health importance and still is so, because millions of under-five children suffer from different forms of malnutrition resulting in significant morbidity and mortality among them [14]. In 2012, the WHO reported the burden of malnutrition among under-five African children to be 59 million of which stunting accounted for over one third of this population with 19.7 million stunted under-fives, wasting of 14.5 million, underweight of 36 million while, 9 million were overweight [15]. Sub-Saharan Africa is home to 90% of the world’s malnourished under-five children of which Nigeria is one of the countries with the largest population in the region [16]. The presumed factors responsible for this high figure in Sub-Saharan Africa are; lack of access to nutritious food which increases their risk to infectious diseases, lack of access to life-saving treatments, lack of access to safe drinking water, sanitation and hygiene necessary for diarrhoea disease prevention. Poor implementation of WHO recommendations such as the use of Insecticides Treated Nets (ITNs), exclusive breastfeeding and immunization strategies are among the environmental factors contributing to the frightening data [17]. The WHO in 1995 drew up cut-off values for public health significance in malnutrition which categorized the prevalence of the different forms of malnutrition from very low prevalence to low, medium, high and very high prevalence. These cut-offs were different for the different forms of malnutrition. They draw attention to the magnitude of the problem of malnutrition and are useful to guide policies and interventions towards addressing malnutrition among under-fives [18,19].
In Nigeria, the prevalence of underweight undernutrition among under-fives was 29% in 2013, while in 2018 there was a reduction to 23% [20,21]. Under-weight malnutrition reflected the effect of both short term and long term malnutrition, hence in some write-ups it was taken as the prevalence of malnutrition [22]. The prevalence cut-offs for underweight given by the WHO categorized that any prevalence less than 10% was low prevalence, 10% to 19% was medium prevalence, 20% to 29% was high prevalence while, 30% was very high prevalence. When this classification was applied to the reports of the national surveys, both 29% and 23% fell under the high prevalence rate category in the prevalence cutoffs for public health significance [23,24]. In North Central Nigeria where this study was carried out, the prevalence of underweight malnutrition was 18.5%, which fell under medium prevalence going by the “cut-off for public health significance” [25,26]. This seeming reduction was as a result of the North Central not being among the worst affected regions like the North East that is bedevilled by the “Boko Haram” insurgency and the North West by banditry with resultant internal displacement of populations, insecurity, hindrances to farming activities and close down of health facilities.
Stunting undernutrition was sustained at 37% prevalence between 2013 and 2018 in Nigeria [27,28]. The WHO prevalence cut-offs for stunting revealed that less than 20% was low prevalence, 20% to 29% was medium prevalence, 30% to 39% was high prevalence while, 40% and above was very high prevalence. Applying this tool to the national survey report for stunting of 37%, it fell under ‘high prevalence’ in the cut-off for public health significance [29]. The Northern Nigeria situation described above having persisted for more than five years was culpable as well in the stunting scenario. Stunting is the result of long-term nutritional deprivation arising from lack of access to nutritious food and recurrent infections which tend to put children at greater risk for illness and death [30,31]. Civil unrest contributes to food insecurity, lack of essential amenities and inability to treat childhood diseases.
Wasting was 18% in 2013 but witnessed a remarkable reduction over a five year period to 7% in 2018 while in North Central Nigeria the prevalence was 11.7% [32,33]. The prevalence cut-offs for public health significance for wasting showed that less than 5% prevalence was low prevalence, 5 to 9% was medium prevalence, 10% to 14% was high prevalence, while 15% prevalence and above was very high prevalence of wasting malnutrition [34,35]. Going by this, a wasting prevalence of 11.7 was considered ‘high prevalence of wasting’. This trend that was seen over the last decade emphasized that truly, wasting was indicative of acute nutritional episodes. It determined the nutritional status in the period just before the survey which was subject to change depending on prevailing environmental, behavioural or biological factors: this is the only plausible explanation for this spurious difference in data.
Overweight/obesity globally has a prevalence rate of 5.6% it was 4% in Nigeria as of 2013 and 2% was reported in the 2018 survey while in North Central Nigeria the prevalence of overweight was 1.3% [36,37]. When using overweight/obesity as an indicator, the public health significance cut-off for overweight showed that less than 2.5% prevalence was very low, 2.5 to less than 5% prevalence was low prevalence, 5% to 9% was medium prevalence, 10% to 14% prevalence was high prevalence rate while 15% and above was very high prevalence rate of overweight/obesity [38]. Going by this classification, the overweight prevalence of 1.3% documented for North Central Nigeria was in keeping with “very low” prevalence rate. The Nigerian prevalence of 4% fell under ‘low’ prevalence rate, while the global prevalence of 5.6% fell under ‘medium’ prevalence rate while the 2% reported in the 2018 NDHS was very low prevalence. The seeming gradual rise before 2013 was because there has been no effort to stem the rate of overweight in more than 15 years [39]. Meanwhile, the reduction reported for 2018 can be said to be due more to a fall in socioeconomic activities of the population from the internal unrest earlier described which has resulted in food insecurity.
From the aforementioned, the prevalence of various forms of malnutrition among under-five children, despite the seeming drop in some of them, is actually due to a rise in population, thus malnutrition have remained high and would continue to increase except drastic actions were taken to forestall the negative trend with strategies and policies that will address the double burden brought on by the spectrum of overweight/obesity [40].
Knowing that the under-five child does not exist in isolation, and that there is an interaction of various components (that is, the context, home environment, bio psychosocial and socio-cultural components), which interplay to determine their nutritional status, the role of the family is therefore underscored. The child is a member of a family, a community, a society with unique health beliefs, and cultural and religious practices, which all interplay to contribute to their nutritional status [41-43]. Family members have different tasks or roles which they individually must carry out for a smooth family function thereby creating an enabling environment for healthy growth of the under-five child. It was against this backdrop that the author sought to know whether a relationship existed between the nutritional status of under-fives and their family functionality.
The study was a hospital based descriptive (cross sectional analytical) study which took place at the Under-five Clinic of Federal Medical Centre, Bida. Children from ages 6 to 59 months who met the inclusion criteria and their parents gave consent were recruited for the study. Sample size determination was calculated using malnutrition prevalence of 18.5% reported in the 2013 NDHS and Leslie Kish’s formula for single population proportion was used. This gave the sample size as 230. Systematic random sampling technique was used for subject’s selection. Excluded were children with chronic diseases that could influence their nutritional status e.g. children with HIV/AIDS (Human Immunodeficiency Virus infection and Acquired Immune Deficiency Syndrome), tuberculosis, established malignancies, children with congenital anomalies e.g. congenital heart disease, inborn errors of metabolism and children too ill to withstand the stress of measurements. The questionnaire was interviewer administered and consisted of four sections. Section A was socio-demographic data of child such as sex, age, tribe, religion, birth order, household size as well as prevalence and risk factors for malnutrition. Section B was child’s anthropometric measurements such as weight (kg), height/length (cm), for the determination of nutritional status. Section C was parent’s/care giver’s socio- demographic characteristics, prevalence and risk factors for family dysfunction. Section D was family function assessment using the Smilkstein family APGAR tool. Anthropometric measurements were compared with the WHO child growth reference values of 2006 to note the Z-scores and determine the nutritional status. Nutritional status were defined by: percentage of underweight i.e. WAZ (weight-for-age below -2 Standard Deviation (SD) of the WHO Child Growth Standards median) ; percentage of stunting i.e. HAZ (height-for-age below -2 SD of the WHO Child Growth Standards median); percentage of wasting i.e. WHZ (weight-for-height below -2SD of the WHO Child Growth Standards median); percentage of overweight i.e. BMI for age (weight-for-height 2 above +2SD of the WHO Child Growth Standards) among children under five years of age.
The data collected were then entered into the Statistical package for social sciences version 23 (IBM SPSS version 23, United States). Summary statistics (descriptive statistics for means, standard deviations) were generated and the prevalence of malnutrition and family dysfunction were determined. Cross tabulations of appropriate variables were done to test for associations between dependent and independent variables at 5% level of significance. Approval for the study was obtained from the Hospital research and ethics committee.
An average of 1,974 under-five children was seen at the under- five clinic of Federal Medical Centre, Bida from August 2017 to October 2017, of which 230 were recruited for this study. The ages of under-five children ranged from 6 months to 59 months. The majority of under-five children were from the 6-11 months’ group which represented 93 (40.4%) of the study population. The mean age was 20.3 ±15.2 months. There were 123(53.5%) males and 107 (46.5%) female under-five study participants. The male to female ratio was 1.2:1 (Table 1).
| Variables | Frequency | Percentage (%) |
|---|---|---|
| Age group (in months) | ||
| 6-11a | 93 | 40.4 |
| Dec-17 | 48 | 20.9 |
| 18-23 | 21 | 9.1 |
| 24-29 | 15 | 6.5 |
| 30-35 | 7 | 3 |
| 36-41 | 16 | 7 |
| 42-47 | 11 | 4.8 |
| 48-53 | 5 | 2.2 |
| 54-59 | 14 | 6.1 |
| Sex | ||
| Male | 123 | 53.5 |
| Female | 107 | 46.5 |
| Residence | ||
| Rural | 30 | 13 |
| Semiurbanb | 200 | 87 |
| Religion | ||
| Christianity | 51 | 22.2 |
| Islam | 179 | 77.8 |
| Ethnicity | ||
| Nupe | 163 | 70.9 |
| Hausa | 12 | 5.2 |
| Yoruba | 22 | 9.6 |
| Igbo | 19 | 8.3 |
| Othersc | 14 | 6 |
| Mother’s age (yrs) | ||
| ≤ 20 | 13 | 5.7 |
| 21-40 | 209 | 90.9 |
| >40 | 8 | 3.4 |
| Father’s age (yrs) | ||
| Primary | 12 | 5.2 |
| Secondary | 52 | 22.6 |
| Tertiary | 145 | 63.1 |
| Othersd | 21 | 9.1 |
| Mother’s occupation | ||
| Unemployed | 70 | 30.4 |
| Self-employede | 108 | 47 |
| Civil servant | 52 | 22.6 |
| Father’s occupation | ||
| Unemployed | 6 | 2.6 |
| Self- employede | 107 | 46.5 |
| Civil servants | 117 | 50.9 |
Note: a: Ages 0-5 months were excluded; b: Bida town is semi urban (or suburban); c: Others included Gwari, Igala, Kwale, Kagara, Tiv, Bini, Kamuku; d: Others included Islamic education, certificated skill acquisition, non-literate; e: Self-employed: Self-owned businesses: Business centres; skilled; Work force: artisans-mechanic, tailors, hairdressers, soap makers, etc; Farmers: Fish farmers, poultry farmers, cattle rearers, crop farmers. Other forms of unskilled labour: Food vendors, freelance labourers, petty trading. n=230.
Table 1: Socio-demographic characteristics of study population (children and parents).
Up to 181 (78.7%) study participants’ families were monogamous in setting, while 49 (21.3%) were polygamous. Also 138 (60%) families were of the nuclear family type, while 92 (40%) were of the extended family type. The mean number of children per family was 3 ± 2. 184 (80%) study participants families have four or fewer number of children while 46 (20%) have more than 4 children. Similarly, households were small with a mean household size of 4 ± 5. Small households of four or less were represented by 93 (40.4%) and larger household of more than five persons per household represented 137 (59.6%) (Table 2).
| Variables | Frequency | Percentage (%) |
|---|---|---|
| Family setting | ||
| Monogamous | 181 | 78.7 |
| Polygamous | 49 | 21.3 |
| Family type | ||
| Nuclear | 138 | 60 |
| Extended | 92 | 40 |
| Marital status | ||
| Married | 229 | 99.6 |
| Separated | 1 | 0.4 |
| No of children | ||
| ≤4 children | 184 | 80 |
| >4 children | 46 | 20 |
| Household size | ||
| ≤4 persons | 93 | 40.4 |
| >4 persons | 137 | 59.6 |
Table 2: Socio-demographic characteristics (family structure) (n=230).
The prevalence of underweight was 63/230 which equaled 0.2739 and on expressing in percentage gave approximately 27%. The others were stunting with a prevalence of 23.5%, wasting prevalence was 27.8% and overweight prevalence was 2.2%. It should be noted that overweight as determined by BMIZ was used in line with the WHO recommendation as a more reliable measure of overweight in children. BMIZ gave 2.2% prevalence. On sub-classification, the prevalence of severe underweight malnutrition calculated from P=n/N was 24/230 which was equal to 0.1043, expressing this in percentage gave 10.4%. Applying this to determine the prevalence of the severe forms of other malnutrition revealed that, the prevalence of severe stunting in the study population was 5.7%, severe wasting was 6.5%, while the severe form of overweight (i.e. obesity) was 2.6% (Table 3).
| Variables | Standard deviation | Frequency sub-class | Percentage (%) sub-class |
Total | Percentage (%) malnutrition |
|---|---|---|---|---|---|
| WAZ | |||||
| Severely Underweight | -3SD | 24 | 10.4 | ||
| Underweight | -2SD | 39 | 17 | 63 | 27.4 |
| Normal weight | -1to+1SD | 159 | 69.1 | ||
| Overweight | +2SD | 6 | 2.6 | ||
| Obese | +3SD | 2 | 0.9 | ||
| HAZ | |||||
| Severely stunted | -3SD | 13 | 5.7 | ||
| Stunted | -2SD | 41 | 17.8 | 54 | 23.5 |
| Normal length/height | -1to+2SD | 172 | 74.8 | ||
| Abnormal height/Endocrine disorder | +3SD | 4 | 1.7 | ||
| WHZ | |||||
| Severely wasted | -3SD | 15 | 6.5 | ||
| Wasting | -2SD | 49 | 21.3 | 64 | 27.8 |
| Normal | -1 to +1SD | 165 | 71.8 | ||
| Overweight | +2SD | 1 | 0.4 | ||
| BMI for age Z score | |||||
| Severely wasted | -3SD | 197 | 85.7 | ||
| Wasting | -2SD | 4 | 1.7 | ||
| Normal BMI | -1to+1SD | 18 | 7.8 | 11 | 4.8 |
| Overweight | +2SD | 5 | 2.2 | ||
| Obese | +3SD | 6 | 2.6 |
Table 3: Prevalence of malnutrition and sub-classification (n=230).
Five components were measured to determine the prevalence and pattern of family function, these included: Adaptation (which was the component with lowest positive responses) with 48.7%, partnership was 51.7%, growth was 52.6%, affection was 53.7% and resolve (the component with highest positive responses) was 62.2% (Table 4).
| Variables | Frequency | Percentage (%) |
|---|---|---|
| Adaptation | ||
| Hardly ever | 3 | 1.3 |
| Some of the time | 115 | 50 |
| Almost always | 112 | 48.7 |
| Partnership | ||
| Hardly ever | 10 | 4.4 |
| Some of the time | 101 | 43.9 |
| Almost always | 119 | 51.7 |
| Growth | ||
| Hardly ever | 12 | 5.2 |
| Some of the time | 97 | 42.2 |
| Almost always | 121 | 52.6 |
| Affection | ||
| Hardly ever | 13 | 5.7 |
| Some of the time | 93 | 40.4 |
| Almost always | 124 | 53.9 |
| Resolve | ||
| Hardly ever | 6 | 2.6 |
| Some of the time | 81 | 35.2 |
| Almost always | 143 | 62.2 |
Note: *These five components were measured to determine the pattern of family function and the mean score of family function was 7.5 ± 2.1
Table 4: Pattern of family function (n=230).
The prevalence of family dysfunction was 2.18%, moderate family dysfunction was 43.91%, while 53.91% were highly functional families (Figure 1). The mean score of family function was 7.5 ± 2.1.
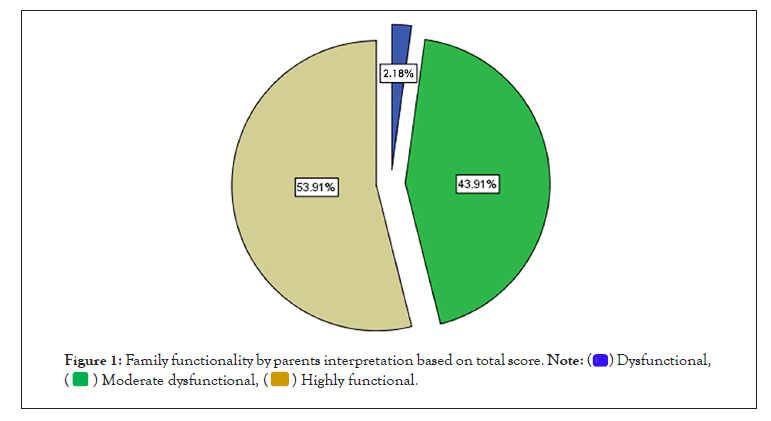
Figure 1: Family functionality by parents interpretation based on total score.
This contingency table revealed that 14.8% of children with underweight malnutrition assessed by WAZ were from moderately dysfunctional families. This was more than 12.6% of children with underweight malnutrition who were from highly functional families. However, this difference was not statistically significant with an x2 of 6.179 and p-value of 0.186. Similarly, HAZ assessment showed that more stunted children (12.6%) were from moderately dysfunctional families compared to 10.9% stunted children from highly functional families. This observation too was not statistically significant with an x2 of 5.810 and p-value of 0.214.
WHZ in assessment of wasting was the only indicator of under nutrition that showed there were more children with wasting malnutrition (16.1%) from highly functional families compared to 10.9% who were from moderately dysfunctional families. Also, while there were no under-five children with underweight or stunting malnutrition from dysfunctional families, 0.9% of under- fives with wasting malnutrition were from dysfunctional families.
The BMIZ assessing overweight in this study showed that more overweight under-fives were from highly functional families with 4.3% compared to 0.4% from moderately dysfunctional families (Table 5).
| Nutritional status | Dysfunction | Moderate dysfunction | Highly functional | Total | X2 | P- value |
|---|---|---|---|---|---|---|
| WAZ | ||||||
| Normal | 5 (2.2%) | 65 (28.2%) | 89 (38.7%) | 159 (69.1%) | ||
| Underweight (underweight+severe underweight) | 0 | 34 (14.8%) | 29 (12.6%) | 63 (27.4%) | ||
| Overweight | 0 | 2 (0.9%) | 6 (2.6%) | 8 (3.5%) | 6.179 | 0.186 |
| HAZ | ||||||
| Normal | 5 (2.2%) | 69 (30.1%) | 98 (43%) | 172 (75.3%) | ||
| Stunting (stunting+severe stunting) | 0 | 29 (12.6%) | 25 (10.9%) | 54 (23%) | ||
| Endoc | 0 | 3 (1.3%) | 1 (0.4%) | 4 (1.7%) | 5.81 | 0.214 |
| WHZ | ||||||
| Normal | 3 (1.3%) | 76 (33.1%) | 86 (37.4%) | 165 (71.8%) | ||
| Wasting (wasting+severe wasting) | 2 (0.8%) | 25 (10.9%) | 37 (16.1%) | 64 (27.8%) | ||
| Overweight | 0 | 0 | 1 (0.4%) | 1 (0.4%) | 2.012 | 0.734 |
| BMIZ | ||||||
| Normal | 0 | 11 (4.8%) | 7 (3%) | 18 (7.8%) | ||
| Wasting | 5 (2.2%) | 89 (38.7%) | 107 (46.5%) | 201 (87.4%) | ||
| Over/Obes | 0 | 1 (0.4%) | 10 (4.4%) | 11 (4.8%) | 8.541 | 0.074 |
Table 5: Pattern of family function (n=230).
The result from this study revealed that malnutrition was a major problem confronting under-five children in the study area. One of the easily overlooked environmental factors was family functionality which this study showed influenced the nutritional status of under-five children. Of the 230 subjects recruited for this study, 53.5% were males and 46.5% were females, this distribution is similar to the findings in Jos North LGA, North Central Nigeria where the proportion of recruitment was 60% males to 40% females [1] also at Kusada, North Western Nigeria, it 37.5% males to 62.5% females while [2] the South West observed 48.3% males to 51.7% females in the distribution of under-fives recruited [3,4]. In addition Anambra, South Eastern Nigeria had a male to female distribution of 50.3% males to 49.7% females [5]. These differences had no effect on the findings of their studies but rather showed a good representation of both sexes in their study population. In this study the mean age of under-five children was 20 ± 14 months. The age range of 6 to 11 months had the highest representation with 40.4% and was closely followed by age group 12 to 17 months with 20.9%, while 18 to 23 months was 9.1%. This showed a steady reduction in the number of recruited subjects with increasing age. This portrayed that the predominant age group recruited was 6 months to 23 months, they accounted for 70.4% of recruited under-fives. This predominance of the younger age group was observed too in the work by Saki [6]. Who had 31.4% from the age range 12 months to 23 months while another work had the highest representation from age range 6 months to 12 months with 67% [7]. This is because majority of this age group were the ones still attending the under-five clinics for immunization schedules as against the older under-fives (24-59 months) who were at pre-school, and the age group (6-23 months) were very much dependent, vulnerable and prone to ill health on account of their immature immunity. This was particularly true for this study.
Studies across Nigeria exposed that family structure played a direct role in family function [8-10]. Findings contributing to family structure in this study and hence family function were that 99.6% of mothers were married, 78.7% were of monogamous family and 60% were nuclear in family. Both ‘fathers’ and ‘mothers’ ages were predominantly from the range of 21 to 40 years with 72.6% for fathers and 90.9% for mothers respectively. This implied that the parents of these children are in their active and productive age group; this has socioeconomic implications for the families. Their study demonstrated that having active and productive parents translated to the ability to meet their family’s needs [11]. The study expounded that having a good family structure such as was seen in this study translated to a good environment and well-structured families inferred a good family function which were suitable for growth and wellbeing of under-five children [12]. Although this study was carried out in a Muslim dominated environment that allowed the practice of polygamy, in this study it was observed that there was a predominantly monogamous nuclear family interaction. This finding was similar to those who also had predominantly monogamous nuclear family interaction in their study however; they did not state the predominant religion [13]. The study also had a predominantly monogamous setting of marriages (92.7%) but there was an almost even distribution in religion with 34% of Christians, 32% of Muslims and 34% of African traditional worshippers [14].
Prevalence of malnutrition and family function
In this study, underweight malnutrition was 27.4% and by public health significance classification fell under “high prevalence” [15]. It was higher than the prevalence reported for Nigeria of 23% [16]. The severely underweight undernutrition in this study of 10.4% was also higher than the severely underweight undernutrition reported for Nigeria of 8% [17]. The proportion of children who were underweight in Nigeria according to the national survey, were also reportedly more in rural areas (29%) than in the urban areas (16%) [18]. It is similar to the findings of this study where the proportion of children with underweight undernutrition that were resident in sub-urban Bida town was 82.5% while those from rural villages were 17.5%. The low prevalence of 17.5% from the rural villages however, was not necessarily because they had better nutrition; rather it was because they were very few that accessed health care at the under-five clinic of the FMC, Bida. This implied that there is still much work to be done to achieve universal coverage and equity in health care delivery to disadvantaged rural communities. Underweight finding in this study was also higher than the report of another study, where the prevalence of underweight malnutrition was 9.1% [19]. Although reasons of being a hospital based study with children coming from average to rich caregivers/mothers was reported as accountable for their findings at Saki [20] the same could not be said for this study which though was also a hospital based study with high rates of educated (72.6%) and empowered mothers (69.6%), had a higher prevalence of underweight malnutrition.
Wasting prevalence in this study was 27.8% while 6.5% suffered from severe wasting. Going by public health significance classification, this fell under “very high prevalence” that required urgent attention to address it [21,22]. It was also higher than the NDHS 2018 prevalence for Nigeria of 7% of which 2% were severely wasted. Eight percent of children in the rural areas and 5% in the urban areas suffered from wasting undernutrition according to the Nigerian survey [23] which when compared to this study revealed 17.2% from rural areas and 82.8% from urban areas. As earlier stated, this was because only a very few villagers (13%) patronized government hospital for under-five clinic services. Secondly, rural areas households consume what is seasonally available from their farmlands and forests unlike in the urban areas where household income is the main determinant of what is eaten [24]. So even though urban families seem to earn better than rural dwellers, there are so many things competing for the earnings like rents, taxes and bills which the rural family is spared from. The Saki study had a low wasting prevalence of 2.5%, Akwuano study also had a low prevalence of 12.7% while Borgu had 8.8% but the Akwuano study excluded ages 6 to 23 months [25].
Stunting in this study had a prevalence of 23.5% which fell under “high prevalence” in the public health significance classification while severe stunting was 5.7%. This prevalence was less than the reported prevalence of 37% (very high in public health significance classification) in Nigeria in the 2018 demographic survey of which severely stunted under-fives were 19%. The survey also reported an increase with age that peaked at 47% among children aged 24 to 35 months in Nigeria [26] but it was not so with the current study. In the current study, stunting showed peak prevalence in the 6-23 months’ age group with 68.5%.
The level of undernutrition seen so far in this study is a red herring into the true situation in Nigeria in recent years. Considering the proximity of the study location to some troubled zones in the country (Plateau, Kaduna, Benue and Zamfara States) which were neighboring states to Niger State with which it has both geopolitical and economic ties. Some communities in these states have not known peace in recent years on account of crises. In addition, the higher prevalence recorded in this study, can also be due to environmental and behavioral factors such as deleterious cultural practices in childcare, the rising inflation (despite the high level of education and employment among the mothers in this study the cash in hand can only do a little) because of economic down turn or rising inflation, religious disharmony all of which were prevalent in recent times [27,28].
The prevalence of overweight and obesity in this study was 4.8% (which specifically were 2.2% for overweight and 2.6% for obesity) with a public health significance classification of “low prevalence”. This was preferably measured with the BMIZ when children two years and above are the study population or WHZ when children two years and below are the study population [29]. However, the BMIZ is in addition said to correlate strongly with body fats compared to the WHZ hence it was used in this study for children aged six months to five years [30]. The prevalence of overweight/ obesity seen in this study was higher than the prevalence reported for Nigeria in the 2018 survey with 2% and 4% in the 2013 survey which was calculated with WHZ: Thus the national survey reported a 50% reduction in overweight and obesity in Nigeria between 2013 and 2018 [31,32]. A comparative look at the distribution using WHZ and BMIZ in this study revealed that there was 0.4% prevalence with WHZ and 4.8% prevalence with BMIZ. The age distribution showed WHZ detected overweight only in the age group 6-11 months while BMIZ detected overweight/obesity in the age group 42-59 months and this was statistically significant. This established the earlier reports on the age group related sensitivity of these two indicators.
The prevalence of family dysfunction in this study was 2.18%, moderately dysfunctional family was 43.91% and highly functional families were 53.91%. The perceived family functioning in the subject population was measured using the family APGAR scale. This prevalence of family dysfunction (2.18%) was much lower than what was obtained in a similar study at Saki, Oyo State with 19.9%. In this study, there was statistically significant association between family structure and family function as more married families tend to be highly functional compared to separated families, with 53.9% compared to 0%. Also, more monogamous families tend to be more functional compared to polygamous families with 48.3% compared to 5.7%. While nuclear families tend to be more functional compared to extended families with 35.7% compared to 18.3%, but these were not statistically significant.
These findings were similar to the study at Saki which revealed a relationship between family function and family structure. They found that more monogamous families were highly functional compared to polygamous families, and more nuclear families were highly functional compared to extended families. Also in that study, married families tend to be more highly functional compared to separate families [33]. The reason for this trend was because a good family structure was indispensable to good family function and good nutrition. They explained further that both parents will tend to combine resources and be actively involved in child rearing while small sized and nuclear type families meant less demand on the family’s resources [34]. The reasons given holds true for this study. The current study showed too that families with gainfully employed fathers and mothers had higher family functioning with 54.5% and 51.9% respectively compared with unemployed but the differences were not statistically significant. Similarly, mothers with above secondary level of education had better family functioning with 62.9% compared to those with below secondary education (30.2%) and this was statistically significant.
Pattern of family function
Family function has been defined as the process of communicating, relating and or maintaining relationship and making decisions to solve problems among family members or within the family [35]. The role of the family in the physical and psychological development of children cannot be overemphasized and the family’s role was further underscored in different disease conditions and health situations [36,37]. The pattern of family function that was seen in this study showed that the prevalence of family dysfunction was 2.18%, moderately dysfunctional was 43.91% and highly functional was 53.91%. The mean family function score was 7.5 ± 2.1. The family components that were employed to determine the pattern of family function in the study population revealed that 48.7% of the respondents’ families had satisfactory adaptation, 51.7% were satisfied with partnership in their families, 52.6% were satisfied with their families’ disposition to growth, another 53.9% opined that affection within their families was optimal while 62.2% were satisfied with the resolve component. The strongest component therefore, determining family function in this study was “The Resolve” with 62.2% while the weakest was “Adaptation” with 48.7%. Adaptation assesses how families use intra and extra familial resources for problem solving within the family. It is expected that in the event of stress in the family like sickness portends often time, family members would turn to one another for the extra resources to cope. These mothers are expressing their dissatisfaction with the non-availability of ‘intrafamilial’ and ‘extrafamilial’ resources to cope with challenges such as malnutrition however; they expressed satisfaction with the time family members share together, which is a measure of commitment of family members to the family. From Herzer, et al. write-ups, “intra or extra familial” refers to emotional (warmth) and psychological environment within the family which can be disrupted by stress and distress [21,38] further explained that familial resources help families to cope in the face of challenges such as poverty thus we are back to socioeconomic status. Despite the high score on resolve, the low poverty level was largely responsible for the low score in adaptation reported by mothers in this study. In the assessment they observed there was increased need for continual adaptation and reorganization of family roles with increased demand of illness such as is seen with chronic diseases like malnutrition [39]. Similar findings were reported in a systematic review of family functioning of children and adolescents with chronic pain. They found that families of children with medical conditions had higher stress and lower socio-emotional functioning than families with healthy children, also, they found that better family functioning was associated with less disability while, higher disability scores were associated with more family dysfunction [40]. Although [41] looked at the impact of family function on malnutrition, they did not elucidate on the pattern of family function to determine the component of strongest perception or weakest perception. They reported a prevalence of family dysfunction of 19.6% and highly functional family of 80.4% but did not give a breakdown on the proportion that was moderately dysfunctional. With the proportion of moderately dysfunctional families hidden somewhere in their report of (19.6% and 80.4%), it made comparison with this study rather difficult.
Relationship between family function and nutritional status
In the determination of relationship between nutritional status and family functionality, this study tested for association using the chi square test and found that compared to dysfunctional families, functional families were associated with lower rates of undernutrition: underweight with 38.7%, stunting with 42.6% and wasting with 37.4%. In addition, there are relatively few studies to which this study (as it relates to family functionality) can be compared but on further analysis of these lower rates there were insightful findings.
Firstly, there was an association between underweight (WAZ) undernutrition and family function. There were more children with underweight undernutrition from moderately dysfunctional families with 14.8% than from highly functional families with 12.6% but this association was not statistically significant. Also, more children with normal weight for age (WAZ) were associated with higher family functions just like in the study [41,42] and co-workers in their write-up underscored the role a good family function in terms of a good family structure played in good nutrition.
Secondly, stunting (HAZ) showed that more stunted children were from moderately dysfunctional homes with 12.6% than children from highly functional home with 10.9% but this difference was not statistically significant. Stunting in this study was also associated with large households (53.7%) compared to 46.3% from smaller households. A greater proportion of under-fives with normal height for age were from highly functional families (42.6%) compared to 2.2% from dysfunctional families.
Thirdly, wasting (WHZ) prevalence was higher than other forms of undernutrition with 27.8%, with relation to family function it expectedly followed the trend of underweight and stunting undernutrition. The aggregates of children with wasting were highest in highly functional families with 16.1% when compared to 10.9% in moderately dysfunctional families and 0.9% in dysfunctional families. It was highest in the age group 23 months and below with 81.3% followed by 10.9% in the 24 to 41 months’ group, the least however was the age group 42 to 59 months with 7.8%.
Lastly, overweight and obesity tool BMIZ has superior sensitivity in the determination of overweight and obesity. It revealed higher rates of overweight/obesity in highly functional families (4.4%) compared to moderately dysfunctional families of 0.4% and dysfunctional families of 0%. This is naturally the expected trend because a functional setting is expected to be a right environment for adequate nutritional intake which can even be in excess. This train of thought is in line with the findings in Port-Harcourt [43]. They reported a higher prevalence of overweight and obesity among the children of the higher socioeconomic classes whose additional lifestyles of inactivity in the form of use of vehicles for transportation instead of walking, long hours of television viewing and increased urbanization of diets were considered contributory. The study in Ethiopia reported a higher prevalence of overweight and obesity than this study’s’ with a prevalence of 13.8%, specifically 9.6% for overweight and 4.2% for obesity. In similarity with this study, the age groups majorly affected were the 36-47 months old followed by 48-60 months old. They also observed a close association between overweight/obesity and high dietary diversity with consumption of sweet foods. This was also similar to the observations at Port Harcourt.
Based on the findings of this study, the null hypothesis was accepted as no statistically significant associations was seen between the nutritional status of under-five children and their family function and any relationship was a weak one at the most. The prevalence of underweight malnutrition was 27.4%, of which severely underweight was 10.4%; wasting under-nutrition was 27.8% of which severe wasting was 6.5%, while stunting malnutrition was 23.5% of which severe stunting was 5.7% and overweight overnutrition was 4.8% of which the obese was 2.6%. The prevalence of family dysfunction was 2.18%, family with moderate dysfunction was 43.91% and family with highly functional was 53.91%. The strongest component that determined family function in this study was the Resolve with 62.2% while the weakest was Adaptation with 48.7%. The others were Partnership (51.7%), Growth (52.6%), and Affection (53.7%). There is a need to increase awareness and use of the family function tool as much as the family structure and family environment tools in order to better determine and improve the psychological health of under-fives. There is a need for increased awareness and sensitization of physicians who attend to all ages to be conversant with the use of nutritional status assessment tools and family function assessment tools. This will go a long way to help in early detection and address early the various forms of malnutrition. Efforts should be made to prevent childhood obesity by using multipronged approach at population level through targeted education, sustainable interventions related to healthy nutritional practices at school and at home by ensuring highly functional homes and promotion of increased physical activities. There is a need to address the issue of household food security by increasing purchasing power of families in order to combat the price hike in food stuff and decisive actions taken to address insurgence and their far reaching consequences.
Being a cross sectional study, it is relevant to the time the study was conducted and does not describe a causal relationship. Being a hospital based study, the iceberg phenomenon becomes applicable.
Relationship between weaning practices and family function among under-fives in the study population is worth studying. In addition, determinants of malnutrition in the study population as well as studies on each form of malnutrition independently and how each related with the family factors implicated in the literature search. A further replication of this study in the community to reveal the prevalence of malnutrition and pattern of family function in the community as a community based study rather than a hospital based study is another area for consideration.
We express our appreciation to the children and parents at the Under-five clinic for their cooperation.
We declare no relationship financial or otherwise that may inappropriately influence this work.
[Crossref] [Google Scholar] [pubmed]
[Crossref] [Google Scholar] [pubmed]
[Crossref] [Google Scholar] [pubmed]
[Crossref] [Google Scholar] [pubmed]
[Crossref] [Google Scholar] [pubmed]
[Crossref] [Google Scholar] [pubmed]
[Crossref] [Google Scholar] [pubmed]
[Crossref] [Google Scholar] [pubmed]
[Crossref] [Google Scholar] [pubmed]
[Crossref] [Google Scholar] [pubmed]
[Crossref] [Google Scholar] [pubmed]
[Crossref]
[Crossref] [Google Scholar] [pubmed]
[Crossref] [Google Scholar] [pubmed]
[Crossref] [Google Scholar] [pubmed]
Citation: Oladele GO, Oladele CO, Ahmed G, Gara PN, Dirisu EM, Amao EA, et al. (2022) Relationship between the Nutritional Status of Under-Five Children and Family Function as Seen in the Under-Five Clinic of Federal Medical Centre Bida, North Central Nigeria. Pediatr Ther. 12:436.
Received: 20-Dec-2021, Manuscript No. PTCR-22-15523; Editor assigned: 31-Dec-2021, Pre QC No. PTCR-22-15523 (PQ); Reviewed: 11-Jan-2022, QC No. PTCR-22-15523; Revised: 18-Jan-2022, Manuscript No. PTCR-22-15523 (R); Published: 25-Jan-2022
Copyright: © 2022 Oladele GO, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.