Advanced Techniques in Biology & Medicine
Open Access
ISSN: 2379-1764
ISSN: 2379-1764
Research Article - (2023)Volume 11, Issue 1
Introduction: Low vision rehabilitation services are one of the least covered subjects in ophthalmic literatures. But, 2.2 billion people have Visual Impairment (VI) or blindness worldwide. Among these, 1 billion people have VI that could have been prevented or addressed.
Objective: To determine the barriers of low vision rehabilitation services in Ethiopia.
Methodology: A cross sectional descriptive survey conducted over practicing ophthalmic personnel in Ethiopia from June 1-July 30, 2020. The data was entered to Epi data manager version 4.4.1.0 and exported to SPSS version 23 for analyses. Descriptive statistics like means, proportions and frequency tables was applied for different analysis. Chi-square test was used to test association between independent variable and dependent variables.
Results: A total of 150 (72.8%) out of 206 responded to the questionnaire and completed it. 115 (76.7%) were males. Mean and standard deviation of age was 30.62 ± 3.89 years. Among study participant’s 54 (36.0%) were Ophthalmologists and subspecialists, 6 (4.0%) Cataract-Surgeon, 49 (32.7%) Ophthalmology-Residents and 27 (18%) Optometrists. The major barriers in providing low visions care includes: non-availability and expensiveness of low vision devices 136 (90.67%), lack of training 117 (78%), lack of awareness 49 (32.7%) and lack of interest/motivation 38 (25.3%). The perception that lack of interest/motivation is a major barrier is significantly higher (OR 3.148 (1.459, 6.795)) among knowledgeable than not knowledgeable about low vision services and among those trained in Ethiopia (OR 5.062(1.345, 19.050)) than abroad. Lack of training was perceived to be a major constraint in a greater proportion of respondents who were from institution giving low vision rehabilitation (OR 4.0125 (1.471, 10.945)) than who didn’t.
Conclusion and recommendation: Non-availability of low-vision devices and expensiveness of low vision device within the country is the most common constraint for the provision of low vision rehabilitation. It is better if Ethiopian Ministry of Health give concern for ways to provide low vision devices at all government eye care services.
Low vision rehabilitation service; Barriers; Ophthalmic personnel
Visual impairment is classified as distance and near; by international classification of diseases 11(2018). Distance vision impairment is further divided into four as mild VI with Visual Acuity (VA) of <6/12 on the better eye, moderate VI (<6/18), severe (<6/60) and blindness (<3/60). The Near Visual Impairment (NVI) is defined as near VA worse than N6 or M.08 with existing correction [1].
9 out of 10 of the world's blind live in a developing country, especially Asia and Africa [2]. The causes for preventable or treatable VI include: Uncorrected Refractive Error (URE) (123.7 million), cataract (65.2 million), glaucoma (6.9 million), corneal opacities (4.2 million), diabetic retinopathy (DR) (3 million) and trachoma (2 million). The treatable NVI is commonly caused by unaddressed presbyopia (826 million) [3]. In developing country prevalence of distance VI is four times higher than developed regions. Unaddressed NVI are >80% in Africa but lower than 10% in developed regions [4].
The national prevalence of blindness and low vision are 1.6% and 3.7% respectively with considerable regional variations in Ethiopia [5]. In another institution based study in St. Paul hospital done by Cherinet, et al. in 2019, the prevalence of low vision and blindness is 10.3% and 7.3% respectively [6].
Vision rehabilitation may begin starting from birth and continues throughout life time. The goal of low vision rehabilitation should be to maximize the visual function of individual. In doing this, the individual becomes independent and the quality of life is improved because there is enhanced visual function [7]. Low vision rehabilitation requires usually multidisciplinary team. This team include: Medical, optometric, allied health (occupational therapist/physical therapist), social, educational/rehabilitative, mobility and psychological services [8].
Low vision can dramatically pose the social, psychological and economic problems on the individual patient, the community and the country at large. Low vision and blindness from cataract, DR, glaucoma and URE affect 1.58-2.31 million people in the UK. Direct health care cost is £3.0 billion, with impatient and day care cost being £735 million and outpatient comprising £771 million. Indirect costs estimated to be £5.65 (5.12-6.22) billion [9,10].
Patients having vision loss was found to have 4.6 times higher risk of suffering from psychological distress compared to patients with normal vision. It was found in 49.8% of patients who had loss of vision at least in one eye while 18.3% of the controls had it. Patients with vision loss in both eyes and worse VA in the better eye are more likely to have psychological distress than patients with vision loss in one eye only and good VA in the better eye respectively [11].
Even if there are studies done about vision rehabilitation services across the world, there is no such study done in Ethiopia yet amid continuous increment in VI and blindness in Sub-Saharan Africa and Ethiopia [12]. Despite the efforts of some globally recognized individuals and institutions, coverage of low-vision rehabilitation service and the patient flow where the service is available have remained low even in developed regions [13].The aim of this study is to explore the barriers of visual rehabilitation services among the ophthalmic personnel in all centers in Ethiopia.
The study was conducted from June 1 to July 30, 2020 at all governmental and non-governmental ophthalmic centers in Ethiopia. Ethiopia is one of the rapidly developing countries in sub-Saharan Africa. It is located in tropical climatic condition. It is the 2nd most populous (114.9 million) nation after Nigeria (206 million) in Africa. A cross sectional descriptive survey was conducted over practicing ophthalmic personnel in all ophthalmic centers in Ethiopia who were accessible.
Data was taken from practicing ophthalmologists, cataract surgeons, Ophthalmology residents, optometrists and ophthalmic nurses accessing by email. Initially the professionals included were identified. Those who had no internet access and complete address were excluded. Then the web-based online survey format was sent for all professionals fulfilling the inclusion criteria through email. All data were seen and filled on the semi-standard questionnaire by the volunteer professionals working at all centers. A reminder mail was sent and phone called after 4, 5 and 6 weeks for those who didn’t respond to the first mail. The data recorded by all volunteered professionals include: Socio-demographic data, place of work, involvement in low vision practice, awareness about low vision rehabilitation, awareness and involvement in vision 2020 activities, WHO criteria for diagnosis of low vision patients, availability of Low Voltage Directive (LVDs) at their center and their opinion about inclusion of low vision care in the training program. Data collection terminated when the calculated sample size was reached (152). All the responses were collected into the Gmail drive and accessible to the investigators at any point of time. The email was supplied from sinbonageleta@gmail.com from Jimma University Medical Center.
Operational definitions and definition of terms
• Ophthalmic personnel: The professionals working either as ophthalmologists (general, sub-specialty), Ophthalmology residents, Optometrists (BSc, MSc) or Ophthalmic nurses (Diploma, BSc).
• Low vision patient: One who has impairment of visual functioning even after treatment and/or standard refractive correction and has a visual acuity of less than 6/18 to LP or a visual field of <10 from the point of fixation but uses or potentially able to use the vision for the planning and/or execution of tasks.
• Low-vision devices: Appliances, aids or methods/techniques (optical and non-optical) which help low-vision patients to maximize visual potential or for maximal use of the residual vision.
• Low vision rehabilitation service: A care given for patients with low vision by the use of low vision devices, training the effective use of the residual vision and advice about the environment and orientation/mobility skills to enhance and promote the patient’s social, vocational and educational activities.
Validating methods
• Knowledgeable: proper answer for at least 3 of the following 5 parameters [14].
• You consider a person as having low vision based on: WHO criteria
• As to you the criteria for low vision includes: Visual acuity OR visual field
• You consider a person is having low vision by VA if <6/18
• You consider a person is having low vision by visual field if <10 degree
• What is low vision rehabilitation? >3/=3 options
• Awareness: The personnel are aware if responded correctly for 5 or more of the following 8 parameters [15].
• Have you heard about low vision? yes
• Do you know about the availability of low vision devices? yes
• Are you aware of WHO definition of low vision of low vision? Yes
• Do you know any organization providing low vision rehabilitation? Yes
• Are you aware of vision 2020? Yes
• Low vision has not been identified as priority in vision 2020. no
• Are you involved in vision 2020? Yes
• Are you aware of concessions for low vision patients? Yes
Data processing and statistical analysis: Data was entered using epidata version 4.4.1.0 and exported to SPSS version 23.0 to perform statistical tests. Descriptive statistics like means, proportions and frequency tables were applied for the analysis of relevant socio-demographic characteristic. The categorical variables were analyzed by using the Chi-square test to test association with the dependent variables.
A total of 152 out of 206 practitioners agreed to respond making a response rate of 72.8%. Two participants didn’t complete the questionnaire well and therefore not included in the analysis. 115 (76.7%) of the participants were males. The mean age of the respondents was 30.62 years. Residents on training comprised of 32.7% while 36.0% were ophthalmologists and subspecialists and 18% optometrists.
Among respondents, 88% were working at teaching government hospitals while the remaining 12% were working in private centers and NGOs. Regarding their level of experience, 112 (74.7%) respondents had less than five years of experience. Total of 94.7% of the participants noted that their primary site of activity to be on patient’s eye examination with or without training eye care personnel, low vision rehabilitation and community eye health and 19 (12.7%) of them practice on low vision rehabilitation (Table 1).
| Independent variables | Category | Number(N) | Percent (%) |
|---|---|---|---|
| Age | (Mean ± SD) | 30.62 ± 3.89 | - |
| (Minimum,Maximum) | (23,45) | - | |
| ≤ 30 Years | 97 | 64.7 | |
| >30 Years | 53 | 35.3 | |
| Sex | Female | 35 | 23.3 |
| Male | 115 | 76.7 | |
| Qualifications | Seniors1 | 54 | 36 |
| Ophthalmology residents | 49 | 32.7 | |
| Others2 | 47 | 31.3 | |
| Experience | ≤ 5 Years | 112 | 74.7 |
| >5 Years | 38 | 25.3 | |
| Organization where practicing | Governmental | 132 | 88 |
| Non-governmental | 18 | 12 | |
| Over all knowledge status about low vision(Score of ≥ 3 out of 5 score | Knowledgeable | 104 | 69.3 |
| Not knowledgeable | 46 | 30.7 | |
| Over all awareness | Aware | 134 | 89.3 |
| Status low vision(score of ≥ 5 out of 8) | Not aware | 16 | 10.7 |
| Place of training | Ethiopia | 140 | 93.3 |
| Foreign | 10 | 6.7 | |
| Primary area of activity | Patient’s eye examination (Yes) | 142 | 94.7 |
| Training eye care personnel (Yes) | 72 | 48 | |
| Community eye health/prevention of blindness (Yes) | 52 | 34.7 | |
| Low vision rehabilitation services (Yes) | 19 | 12.7 | |
| Others | 5 | 3.3 |
Note:
1Ophthalmologists 49 and 5 Ophthalmology sub-specialists,
2Others (20 BSc in Optometry, 7 MSc in Optometry, 6 cataract surgeons, 3 opticians, 11 Ophthalmic-Nurses)
Table 1: Socio-demographic data of respondents.
All of the respondents (100%) had heard about low vision service. 135 (90%) respondents knew about the existence of low-vision devices. Regarding the level of involvement in low vision practice, only 19 (12.7%) of them were involved in varying levels/scopes of low-vision practice.
Regarding their level of involvement in Vision 2020 activities, ninety four (62.7%) participants had been involved in vision 2020 activities. Majority of the respondents (98.7%) were aware of WHO definition of low vision. Generally 89.3% of the participants have good awareness.
99 (66%) of the respondents defined low vision rehabilitation as training to use low vision devices, mobility training and adaptive training for job, while 14.7% replied training to use low vision devices, 6.7% responded as training to use low vision devices, 6% replied as training to use low vision devices and adaptive training and 2% responded adaptive training and mobility training as a definition of low vision rehabilitation services.
91 (60.7%) of the practitioners considered a person is having low vision when the VA in the better eye is less than 6/18, 22% when the VA is less than 6/60, 16% if the VA is less than 3/60 and 1.3% when the VA is less than 1/60. In terms of VF, eighty (53.3%) of the participants considered a person is having low vision when the VF from the point of fixation is less than 10, 21.3% when the VF is less than 20, 10% when the VF is less than 30. Twenty three (15.3%) respondents were not sure. From all participants 69.3% of them are knowledgeable about low vision (Table 1).
From all participants, 87.4% mentioned retinal problems, post cataract extraction, glaucoma and right eye as a cause of low vision (Figure 1).
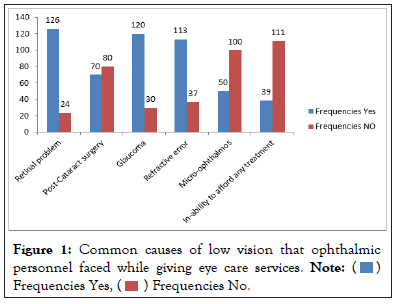
Figure 1: Common causes of low vision that ophthalmic personnel faced while giving eye care services. 

Responses related to the perceived barriers to the provision of low-vision service for the ophthalmic personnel are illustrated in Table 2. Non-availability of low-vision devices and expensiveness of low vision device within the country (n=136; 90.67%) and lack of training in low-vision practice (n=117; 78%) were the main barriers (Table 2).
| Variables for barrier | Number (N) | Percent (%) |
|---|---|---|
| Non-availability and expensiveness of low vision device | 136 | 90.67 |
| Lack of training | 117 | 78 |
| Lack of awareness | 49 | 32.7 |
| Lack of interest/motivation | 38 | 25.3 |
| More work load and lack of man power | 34 | 22.67 |
| Less profitability and time consumption of low vision care | 28 | 18.67 |
| Difficulty in satisfying patients and non-effectiveness of low vision care | 18 | 12 |
Table 2: Major barriers faced in providing low vision care of the ophthalmic personnel.
On the way of improving low vision practices, majority of the respondents were in support of creating public awareness and creating awareness among practitioners representing 85.3% and 84% of the respondents respectively (Table 3).
| Practices | Frequency | Percent |
|---|---|---|
| Improving the availability of low vision devices | 134 | 89.3 |
| Creating public awareness | 128 | 85.3 |
| Creating awareness among practitioners | 126 | 84 |
| Availability of Low vision devices at low cost: | 124 | 82.7 |
| More training programs | 121 | 80.7 |
| Including Low vision as a part of curriculum | 116 | 77.3 |
Table 3: Improving low vision practices.
Table 4 shows the significant factors associated with each constraint/barrier in providing low vision services. The perception that lack of interest/motivation as a major barrier in providing low vision rehabilitation is significantly higher (OR 3.148(1.459, 6.795)) among those who were knowledgeable than not and among those trained in Ethiopia (OR 5.062(1.345, 19.050)) than abroad.
| Independent variable associated with the barrier | Category Of independent variable | Major barrier Ophthalmology personnel face | Odd ratio (95%CI) | P-Value | |
|---|---|---|---|---|---|
| Lack of awareness | |||||
| Knowledge status | Yes | No | |||
| Knowledgeable | 77 | 27 | 2.614(1.265-5.402) | 0.009 | |
| Not knowledgeable | 24 | 22 | |||
| Lack of training | |||||
| Low vision rehabilitation services | Yes | No | |||
| Yes | 9 | 10 | 2.614 (1.471, 10.945) | 0.007 | |
| No | 24 | 107 | |||
| Lack of interest/motivation | |||||
| Age | Yes | No | |||
| ≤ 30 | 67 | 30 | 2.519(1.059, 5.991) | 0.037 | |
| >30 | 45 | 8 | |||
| Sex | Female | 19 | 16 | 3.560(1.582, 8.012) | 0.002 |
| Male | 93 | 22 | |||
| Organization where working | Governmental | 103 | 29 | 3.552 (1.291, 9.768) | 0.014 |
| None governmental | 9 | 9 | |||
| Over all knowledge status about low vision(Score of ≥ 3 out of 5 score | knowledgeable | 85 | 19 | 3.148(1.459, 6.795) | 0.003 |
| Not knowledgeable | 27 | 19 | |||
| Place where the training is obtained/being obtained | Ethiopia | 108 | 32 | 5.062(1.345, 19.050) | 0.016 |
| Foreign | 4 | 6 | |||
| More work load and lack of man power | |||||
| Sex of participants | Yes | No | |||
| Female | 18 | 17 | 5.444(2.352, 12.603) | <0.001 | |
| Male | 98 | 17 | |||
| Non-availability and expensiveness of low vision device | |||||
| Experience(years) for participants | Yes | No | |||
| ≤ 5Years | 7 | 105 | 3.387 (1.103, 10.398) | 0.033 | |
| >5Years | 7 | 31 | |||
| Difficulty in satisfying patients and non-effectiveness of low vision care | |||||
| Organization where working | Yes | No | |||
| Governmental | 111 | 21 | 3.364 (1.170, 9.672) | 0.024 | |
| None governmental | 11 | 7 | |||
| Less profitability and time consumption of low vision care | |||||
| Organization where working | Yes | No | |||
| Governmental | 120 | 12 | 5.0 (1.590, 15.722) | 0.006 | |
| None governmental | 12 | 6 | |||
Table 4: Significant factors associated with barriers of ophthalmic personnel in providing low vision care.
The likelihood of belief that Low Vision Rehabilitation Service (LVRS) is less profitable and consumes time is significantly higher (OR 5.0 (1.590, 15.722)) among the ophthalmic personnel practicing at governmental organization than those practicing at non-governmental organization.
The likelihood of responding that lack of awareness as the main constraint/ barrier was greater for those who were knowledgeable about low vision rehabilitation (OR 2.614(1.265-5.402)) than not knowledgeable. Lack of training was perceived to be a major constraint for the provision of low vision rehabilitation in a greater proportion of respondents who were from institution giving low vision rehabilitation (OR 4.0125 (1.471, 10.945)) than who didn’t provide LVRS.
From the univariate analysis, factors such as age (>30 years, p=0.037), sex (male, p=0.002) and type of organization (government hospital, P=0.024) were significant for the constraint that lack of interest/ motivation is the major constraint for the provision of low vision rehabilitation service.
A good response rate was achieved in this national survey (72.8%) compared to 65% which was achieved in global survey on low vision service provision from 2011 [16].
This study demonstrated that Non-availability of low-vision devices and expensiveness of low vision device within the country (n=136; 90.67%) as a greatest constraint for application of low vision rehabilitation services. Similarly non-availability of low-vision devices was cited by the greatest proportion of respondents (88%) as a barrier in a study done in Nigeria [17]. Non-availability of low-vision devices was also found to be a significant factor among Indian ophthalmologists (72.2%) which is far less than this study. This shows that non-availability of low vision devices and expensiveness of low vision devices is significant problems in Africa than other regions because there is no local production of low vision devices or few if there at all. On another way, only 5.9% (2/34) of participants identified cost as a reason for not obtaining License Verification System (LVS) in Spafford, et al. study done in 2013 at Canada [18]. The possible reason for the difference could be due to the difference in the setup of the research areas because it was done in America where the instruments are readily available and the community living there had better socio-economic status than our setup. The perceived non-availability of low-vision devices in Ethiopia may be a strong indicator to the fact that they are not presently aware that low-vision devices from the Vision 2020 Low-Vision Resource Center of the Hong Kong Society for the Blind are being imported into the country and that most of the simple devices can be produced locally using indigenously available materials and appropriate technology. The prescribing culture of those ophthalmic personnel giving low vision rehabilitation services and the consuming culture of the patients with low vision (end users) could play a role in changing the perception of the non-availability of low-vision devices as a barrier to the provision of low-vision rehabilitation services.
Lack of training in low-vision practice (n=117; 78%) and lack of awareness (n=49, 32.7%) were noted to be the barriers to the provision of low vision rehabilitation services by the respondents. This has proximity with a study conducted among ophthalmologists in India demonstrating comparable figure (82.3%) responding a lack of training as the major constraints to provide low-vision rehabilitation service but 74.7% of the respondents(more than twice in this study) responded a lack of awareness as one of the major constraints to provide low-vision rehabilitation service [17]. Lack of training was also reported by 73.5% of respondents (which was also near to this study) from a survey in Nigeria in 2007 by Okoye, et al. but lack of awareness of the professional was two times higher from the study at Nigeria (60.2%) [13]. Lack of public awareness (60.2%) was one of the major barriers in Nigeria which was slightly lower than this study which was responded by 83.3% of the professionals as one of the common barriers for the applications of low vision rehabilitation in Ethiopia. The majority of the study participants were aware of vision rehabilitation services (54%) in a study done by Overbury in 2011 at Montreal, Canada which was only slightly higher than in this study [19].
Low vision services are rarely given even at tertiary hospitals in Ethiopia as it is understandable from the report that only 19 (12.7%) of the participants were involved in varying levels/scopes of low-vision practice. The result of a Global Survey of Low Vision Service Provision in 2011 was also similar with this finding indicating that most of the African region had either no services, very low/poor coverage or no information could be obtained. The provision of low vision services is related to the availability of trained human resources. The human resource base must be increased by training in low vision services to meet the need for these services. Professionals involved in low vision service include ophthalmologists, optometrists, ophthalmic nurses and rehabilitation workers among others. Therefore, it is very important to find ways to include low vision services as part of different ophthalmic curricula. Effort has to be made at different level of medical education to sensitize increase interest of the medical community to low vision services and to train them to make the appropriate diagnosis and referrals.
More work load with general ophthalmic practice and lack of man power was also mentioned by the Ethiopian ophthalmic personnel representing 34(22.66%) of the respondents as another main constraint. Busy in providing general ophthalmology services (44.3%) was reported by Indian ophthalmologists [17]. This figure is twice the figure reported in this study. The possible reason for the difference could be the time of the research which was done 15 years back when there was little number of ophthalmologists and other ophthalmic personnel. The participants of this research were ophthalmologists who were obviously busy with general ophthalmic activities than low vision rehabilitation. Busy in providing general ophthalmology services (56.6) was even higher in the study done in Nigeria among the ophthalmologists in 2007 by Okoye, et al. [13]. The reason for variability could be same as explained above. Again the participants of this study include only ophthalmologists and residents who were most likely busy at general ophthalmic activities. The average ophthalmic personnel invariably spend a tremendous amount of his workday attending to all manners and forms of general ophthalmic cases. The vital complementary roles of the optometrists and other allied eye-care staff should be considered in addressing this perceived barrier. These categories of worker are more likely to devote more time to low-vision care if properly trained.
Lack of interest/ motivation was reported by 25.3% of the respondents. This finding was reported to be slightly higher (42.2%) in a study done by Okoye, et al. in 2007 among ophthalmologists in Nigeria. Lack of motivation was reported by 54.4% of the participants in a study done in India by Khan, et al. in 2005. This variation might have come from high burden of low vision with low/no low vision rehabilitation service in Ethiopia resulting in higher level of interest and motivation among ophthalmic personnel.
Non-availability of low-vision devices and expensiveness of low vision device within the country, lack of training in low-vision practice, lack of awareness, more work load and lack of man power were noted to be the main barriers among eye care practitioners. Majority of the respondents were in support of creating public awareness and creating awareness among practitioners. The perception that lack of interest/motivation as a major barrier in providing low vision rehabilitation is significantly higher among those who were knowledgeable than not knowledgeable about low vision services and among those trained in Ethiopia than abroad.
Ophthalmologists and other eye care staffs need to get appropriate training in low vision by different ophthalmic societies like ophthalmic society of Ethiopia or Non-Governmental Organizations (NGOs) working with them. The concept of low-vision care should be given more attention in the curricula of the ophthalmology residency program and even the undergraduate medical education and in curriculum of other eye care personnel by Ethiopia ministry of education being with Ethiopia ministry of health. Low vision care education/awareness campaigns should be formulated properly targeting the public and eye-care providers. Availability and accessibility of low-vision devices to ophthalmic personnel and the public should be improved by health care administrators found at different levels. Local production/manufacture of low vision device from easily available ingredients should be encouraged.
Next to God I would like to acknowledge Jimma University Ophthalmology department, my collegue and study participants.
The research is not funded.
The authors declare no conflict of interest.
The corresponding author has planned, supervised, analyzed and written the manuscript. The co-authors also participated on the planning and analysis of the manuscript.
All data generated or analyzed during this study are included in this published article (and its supplementary information files).
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Dendea SG, Ababor JK, Daba KT, Molla JM (2023) Reported Perceived Barriers to Low Vision Rehabilitation Services among Ophthalmic Personnel in Ethiopia. Adv Tech Biol Med. 11:400.
Received: 14-Feb-2023, Manuscript No. ATBM-23-21809; Editor assigned: 17-Feb-2023, Pre QC No. ATBM-23-21809 (PQ); Reviewed: 03-Mar-2023, QC No. ATBM-23-21809; Revised: 10-Mar-2023, Manuscript No. ATBM-23-21809 (R); Published: 20-Mar-2023 , DOI: 10.35248/2379-1764.23.11.400
Copyright: © 2023 Dendea SG, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Sources of funding : No