Angiology: Open Access
Open Access
ISSN: 2329-9495
ISSN: 2329-9495
Research Article - (2024)Volume 12, Issue 7
This study evaluated the safety and effectiveness of a modified stent retrieval technique controlling the micro catheter’s unsheathing level to resolve distal vessel occlusions from migrated emboli. From January 2016 to February 2022, this technique was used on 24 of 445 patients with acute large vessel occlusion strokes in the anterior circulation, with secondary embolus migration into M2, M3, A2, or A3 branches. The procedure used radiopaque stent retrieval systems like Trevo XP 4 ×20 mm and Solitaire Platinum 4 × 20 mm, adjusting coverage through partial re-sheathing of the microcatheter. After recanalizing the primary occlusion, secondary occlusion occurred in 12/6/4/2 patients in the M2/M3/A2/A3 branches, respectively (time from puncture to primary recanalization: 45.5 ± 17 min). Modified TICI scores were 2a and 2b in 8 and 16 patients, respectively. The one-pass rate for secondary occlusions was 70.8%, and 23 of 24 patients achieved a final recanalization rate of at least TICI 2c at the migrated occlusion (mean duration: 23.2 ± 14 min) without significant complications. At 3 months, 16 patients achieved favorable outcomes (mRS, 0–2). This technique was simple, safe, and effective in resolving distal occlusions from migrated emboli.
Mechanical thrombolysis; Stents; Endovascular treatment; Ischemic stroke; Thrombectomy
Mechanical thrombectomy is a well-established treatment protocol for acute Large Vessel Occlusion (LVO) stroke, with favorable clinical outcomes reported [1-3]. Despite its effectiveness, secondary occlusion rates, such as thrombus fragmentation, tortuous vessel course, anterograde flow through a collateral channel, and failure to use a balloon guiding device during the procedure have been reported in 7%–11% of cases [4,5].
Unfortunately, the emergence of new Distal Vessel Occlusions (DVO) can significantly affect the final TICI score and functional disability. For example, a distal MCA-M3 occlusion causing aphasia or an anterior cerebral artery occlusion causing monoplegia can have a devastating impact on patient’s functional independence [6-9].
Neurointerventionalists find it challenging to access and achieve successful recanalization in DVOs, given the small caliber, fragility, and tortuous anatomy of these vessels, all of which can pose safety risks [5,10]. The tortuous arterial anatomy and small vessel caliber can complicate the use of stent retrievers and medium to large bore aspiration catheters, as navigating these distal vessels can be problematic, raising concerns about arterial trauma. To overcome these obstacles, the use of second-generation devices with a smaller profile or technical adjustments of the primary stent to reduce contact area are warranted to minimize the risk and achieve successful recanalization [11-16].
This study aimed to evaluate the safety and effectiveness of a modified Stent Retrieval (STR) technique for the removal of migrated emboli in the M2, M3, A2, and A3 segments during mechanical thrombectomy for acute LVO. This article follows the STROBE (Strengthening the Reporting of Observational studies) in epidemiology reporting guidelines.
Patients
This retrospective study was approved by the local institutional review board, and all participants provided informed consent. All procedures in studies involving human participants were performed in accordance with the ethical standards of the institutional and/or national research committee and the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
From January 2016 to February 2023, we enrolled 24 of 445 (5.4%) consecutive patients who experienced secondary embolic migration to the distal branch (M2, M3, A2, A3) after the primary intervention for acute LVO stroke in the anterior circulation at our institution. Emboli to New Territory (ENT) was defined according to the standard angiographic anatomy [17]. The eligibility criteria for the modified STR technique for DVOs were as follows: After achieving complete recanalization of the primary LVO with a modified TICI (mTICI) score of 2a or 2b, the neurointerventionalist evaluated whether ENT affected the main blood supply to an eloquent area. Additionally, they evaluated if the device was accessible without vascular tortuosity or tension, and if retrograde filling into the ENT would prevent further ischemic progression.
Exclusion criteria
Evidence of intracranial hemorrhage or low density on the initial CT scan in the secondary migrated territory. All patients presented with symptoms of acute stroke and underwent a nonenhanced CT and multiphase CT after neurological evaluation. The following data were collected and reviewed for all patients: age, sex, risk factors, baseline mRS score, NIHSS score, ASPECTS, use of tPA, time from symptom onset to arrival at the hospital, time from symptom onset to femoral puncture, time from femoral puncture to successful recanalization, location of primary LVO, migrated DVO, total procedural time (divided into primary LVO and secondary DVO), primary thrombectomy devices, secondary stent retriever, modified stent retriever attempts, final mTICI score and other relevant information [18].
Modified STR technique
All mechanical thrombectomies were performed through femoral puncture while the patients were under conscious sedation. For the anterior circulation, a balloon guiding catheter (8 or 9 Fr BGC Cello/Medtronic, Irvine, California, USA or 9 Fr Optimo/ Medtronic, Irvine, California, USA) or a non-balloon guiding catheter (Neuromax 6F or Fubuki 7F) was placed as distally as possible in the cervical ICA of the occluded side, using a 5-F long angio-catheter for navigation. The primary LVO site was initially accessed using the Trevo XP Provue 4 × 20 mm (Stryker Neurovascular, Fremont, CA, USA), Solitaire Platinum 4 × 20 mm (Medtronic, Dublin, Ireland), or Penumbra Reperfusion Catheter 5Max Ace 068. A microcatheter [Prowler Select plus (Cordis, Dublin, OH, USA] or Markman 27 or Phenom 21 (Medtronic)] was navigated to the point of occlusion, and the length of thrombus and distal vascular nature was examined using super-selective angiography. In the event of ENT occurring in the DVO after successful recanalization of the primary LVO, either the Trevo XP Provue 4 × 20 mm (Stryker) or Solitaire Platinum 4 × 20 mm (Medtronic) retriever stent was applied. The deployed range was easily identified by the radiopaque wire or marker, respectively.
The modified STR technique was used for clot removal and included adjusting the covered range of the stent by partially resheathing the delivery catheter after fully unsheathing it. The microcatheter and microwire maneuvered over the embolic lesion (Figure 1a), and the radiopaque stent retriever was carefully deployed inside the thrombus by unsheathing the microcatheter (Figure 1b). At this point, the waisted portion of the stent can be indicated by compression of the clot. After allowing 2 min for the clot to engage with the stent, the microcatheter was gently pushed forward to partially re-sheath the stent, reducing the physical friction between the parent artery and the stent (Figure 1c). Resistance during the re-sheathing process indicated that the clot was in contact with the microcatheter. The partially re-sheathed stent was slowly retrieved into the guide catheter by pulling back, with careful monitoring of the motion of the parent artery under an inflated balloon guiding the catheter or proximal aspiration catheter (Figure 1d).
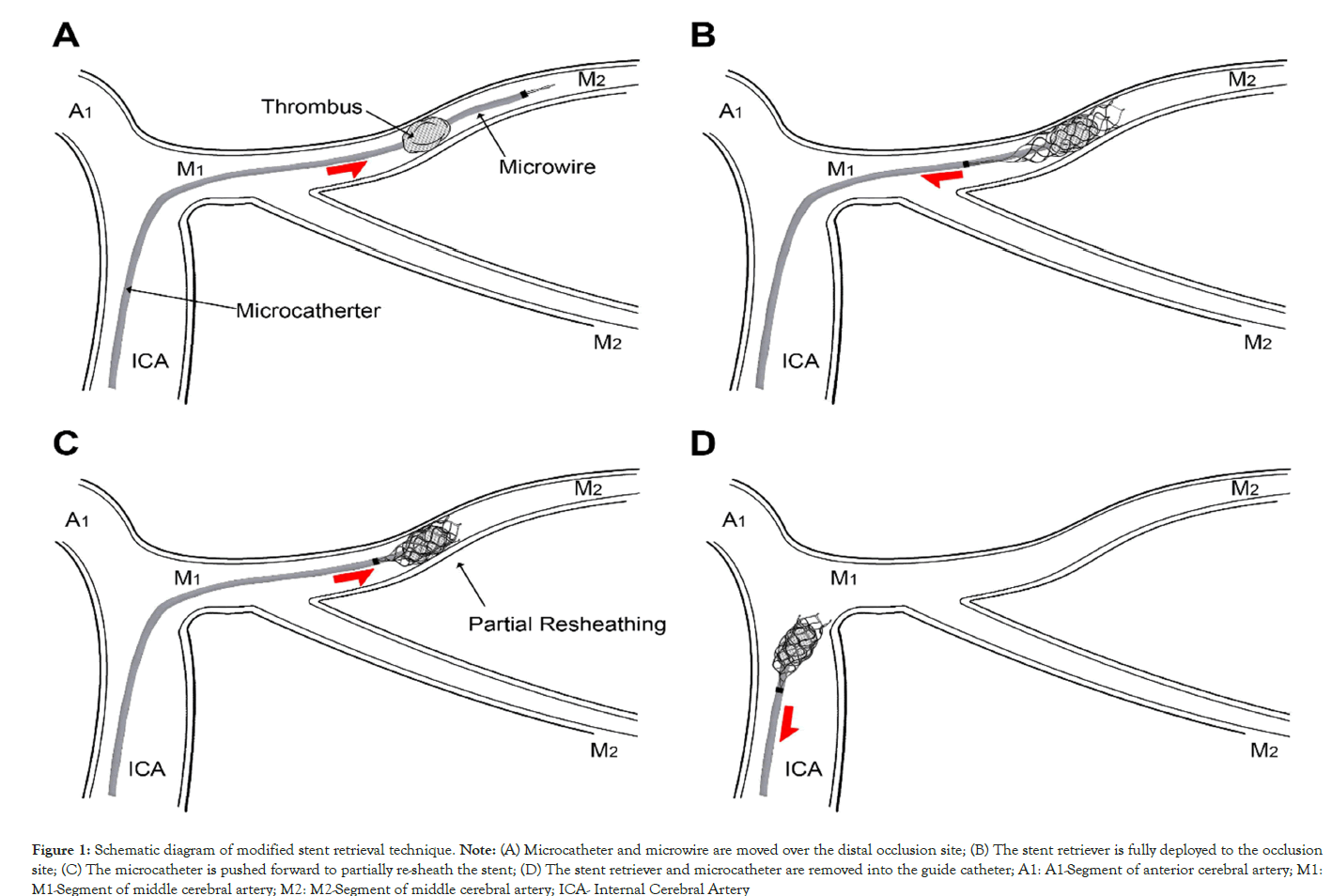
Figure 1: Schematic diagram of modified stent retrieval technique.
Note: (A) Microcatheter and microwire are moved over the distal occlusion site; (B) The stent retriever is fully deployed to the occlusion site; (C) The microcatheter is pushed forward to partially re-sheath the stent; (D) The stent retriever and microcatheter are removed into the guide catheter; A1: A1-Segment of anterior cerebral artery; M1: M1-Segment of middle cerebral artery; M2: M2-Segment of middle cerebral artery; ICA- Internal Cerebral Artery
Complications and outcomes
Procedure-related complications were recorded during the intraangiography and post-procedural CT examinations. Stenosis of the targeted vessel and a double contour layer after retrieval were defined as arterial vasospasm and dissection. Vessel perforation was determined if a contrast leak occurred due to incorrect navigation of the microcatheter and microwire. Postprocedural CT scans were used to identify SAH and Intracerebral Hemorrhage (ICH), which was classified as Hemorrhagic Infarction type 1, 2 (HI 1,2) and Parenchymal Hematoma type 1, 2 (PH 1,2) according to the European Co-operative Acute Stroke Study-II (ECASS II) classification system [19]. Symptomatic ICH was defined as worsening of ≥ 4 points on the NIHSS scale clinical examination, accompanied by hemorrhage on CT after treatment.
The primary LVO and secondary DVO before and after treatment were defined according to the mTICI classification. Successful revascularization was defined as an mTICI score of 2c or 3 and was determined by two blinded physicians based on the procedural process. Patients were routinely scheduled for MRI within 24–48 hours after the procedure. Regional ischemic findings associated with the ENT were evaluated post-recanalization of the DVO and classified into the following three categories: complete, partial, and none. Clinical outcomes were obtained from medical records using the NIHSS and mRS at discharge and 90 days after treatment. A good functional outcome was defined as a mRS score of ≤ 2 at three months.
During the study period, 24 out of 445 patients (5.4%) with acute large intracranial artery occlusions in the anterior circulation, treated with mechanical thrombectomy, developed ENT. All cases of DVOs were managed using the modified STR technique. The demographics, device profiles, and procedural outcomes of patients are summarized in Table 1. The mean age of the patients was 68.3 ± 9.1 years, with 62.5% being women. The median baseline NIHSS score was 12.3 ± 4.4, and 10 patients (41.7%) had received IV tPA within a 4.5-hour time window. The initial median ASPECTS was 8.5 ± 1.0, and the collateral state on multiphase CTA showed good collateral flow in 8 patients, moderate in 9 patients, and poor in 7 patients. Primary LVO was observed in 9 patients at the ICA and in 15 patients at the M1 segment, whereas secondary DVO was noted in 12, 6, 4, and 2 patients at the M2, M3, A2, and A3 segments, respectively. Initially, Solitaire 4 × 20 mm was used for LVO treatment in 9 patients, whereas Trevo 4 × 20 mm was used in 15 patients, with these devices consistently applied for secondary lesions without changing the thrombectomy device.
| Case No | Gender /Age |
Baseline NIHSS | Initial ASPECTS |
Collateral CTA | Primary LVO | Secondary DVO | Initial Device |
Secondary STR |
Primary LVO/Final VO (mTICI) |
Modified STR (times) | Complications | Local infarction | mRS at 3months |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F/68 | 14 | 9 | Moderate | ICA | A2 | Solitaire | Solitaire | 2b/3 | 1 | PH type1 | None | 2 |
| 2 | F/74 | 16 | 8 | Moderate | M1 | M2 | Solitaire | Solitaire | 2b/3 | 1 | Spasm | None | 3 |
| 3 | F/79 | 18 | 7 | Poor | ICA | A3 | ACE 68/Trevo | Trevo | 2a/3 | 2 | - | Partial | 4 |
| 4 | F/74 | 8 | 9 | Good | M1 | M3 | Trevo | Trevo | 2b/3 | 1 | - | Partial | 2 |
| 5 | F/67 | 10 | 8 | Moderate | ICA | M2 | ACE 68 | Trevo | 2a/2c | 1 | - | None | 1 |
| Trevo | |||||||||||||
| 6 | M/63 | 10 | 9 | Moderate | ICA | M3 | Solitaire | Solitaire | 2b/3 | 1 | - | Complete | 2 |
| 7 | F/71 | 15 | 7 | Poor | M1 | A2 | ACE 68/Trevo | Trevo | 2b/3 | 1 | PH type1 | Complete | 4 |
| 8 | M/84 | 17 | 8 | Poor | ICA | M3 | ACE 68/Trevo | Trevo | 2b/3 | 2 | SAH | Complete | 4 |
| 9 | F/55 | 7 | 10 | Good | M1 | M2 | Trevo | Trevo | 2a/3 | 1 | - | None | 1 |
| 10 | M/54 | 9 | 9 | Moderate | M1 | M2 | Trevo | Trevo | 2b/3 | 2 | - | None | 2 |
| 11 | M/63 | 10 | 9 | Moderate | ICA | M3 | Solitaire | Solitaire | 2b/3 | 1 | - | Complete | 2 |
| 12 | F/81 | 16 | 7 | Poor | M1 | A2 | Trevo | Trevo | 2a/3 | 1 | - | Complete | 3 |
| 13 | M/85 | 19 | 8 | Poor | ICA | M2 | ACE 68/Trevo | Trevo | 2a/2a | 3 | Dissection, SAH | Complete | 5 |
| 14 | M/59 | 8 | 9 | Good | M1 | A3 | Solitaire | Solitaire | 2b/3 | 1 | Spasm | None | 2 |
| 15 | F/65 | 6 | 10 | Good | M1 | M2 | Trevo | Trevo | 2b/3 | 1 | - | None | 0 |
| 16 | F/54 | 7 | 9 | Moderate | M1 | M2 | Trevo | Trevo | 2a/3 | 1 | - | None | 2 |
| 17 | F/68 | 14 | 9 | Good | M1 | A2 | Solitaire | Solitaire | 2b/3 | 1 | - | None | 1 |
| 18 | M/67 | 12 | 8 | Moderate | M1 | M2 | Solitaire | Solitaire | 2b/2c | 1 | - | None | 2 |
| 19 | F/71 | 18 | 7 | Poor | ICA | M3 | ACE 68/Solitaire | Solitaire | 2b/3 | 2 | Spasm, PH type1 | Complete | 4 |
| 20 | F/64 | 6 | 10 | Good | M1 | M2 | Trevo | Trevo | 2a/3 | 1 | - | None | 0 |
| 21 | F/72 | 16 | 9 | Moderate | M1 | M2 | Trevo | Trevo | 2b/3 | 2 | - | Partial | 2 |
| 22 | M/56 | 14 | 9 | Good | M1 | M2 | Solitaire | Solitaire | 2b/2c | 1 | - | None | 1 |
| 23 | F/77 | 18 | 7 | Poor | ICA | M2 | ACE 68/Trevo | Trevo | 2a/3 | 3 | Spasm, PH type1 | Complete | 3 |
| 24 | M/67 | 8 | 10 | Good | M1 | M3 | Trevo | Trevo | 2b/3 | 1 | - | None | 0 |
Note: NIHSS-National Institute of Health Stroke Scale; ASPECTS-Alberta Stroke Program Early CT Score; CTA-Computed Tomography Angiography; LVO-Large Vessel Occlusion; DVO-Distal Vessel Occlusion; VO-Vessel Occlusion; STR-Stent Retrieval; mTICI-modified Thrombolysis in Cerebral Infarction; IH-Intracranial Hemorrhage; mRS-modified Rankin Scale; ICA-Internal Carotid Artery; M1/M2/M3, M1/M2/M3-Trunk of middle cerebral artery; A2/A3, A2/A3-Trunk of anterior cerebral artery; PH-Parenchymal Hemorrhage; SAH-Subarachnoid Haemorrhage.
Table 1: Demographics, device profiles and outcomes of study participants.
In four patients, the ACE 068 reperfusion catheter was used as the first-line device without balloon guiding, and the DVO was successfully recanalized using the Trevo 4 × 20 mm via the modified STR technique. Overall, the primary LVO was fully recanalized, with mTICI 2a achieved in 33.3% (8/24) of patients and mTICI 2b achieved in 66.7% (16/24) of patients, with the condition being influenced by the presence of DVO in all cases. The modified STR technique for secondary DVO showed favorable outcomes, with a low number of procedural runs (mean 1.4 ± 0.6 times; range, 1–3) and achieved successful recanalization with TICI ≥ 2c in 95.8% (23/24) of patients, with a first-pass recanalization rate of 70.8% (17/24). In terms of overall time metrics, the average time from symptom onset to hospital admission was 70 ± 54 min. The time from symptom onset to femoral puncture for the procedure was on average 110 ± 82 min. The mean recanalization time was 63.6 ± 12 min, with 45.5 ± 17 min for primary LVO cases and 23.2 ± 14 min for secondary DVO cases (Table 2). During the removal of the secondary clot, four instances of vessel spasms and one case of dissection occurred, with no vascular perforation observed. The vessel spasms spontaneously resolved, but the dissection eventually led to occlusion after the procedure. Asymptomatic ICH was observed in six patients on post-procedural CT, consisting of minor Parenchymal Hematoma type 1 (PH1) in four patients and subarachnoid hemorrhage in two patients, with no neurological deterioration noted. A routine follow-up MRI within 24–48 hours was performed for all patients. The presence of local ischemic findings was correlated with the recanalization of DVO, resulting in complete infarction in eight cases, partial infarction in three cases, and no infarction in 13 cases. At the 3-month mark, 16 patients had mild neurological sequelae (mRS ≤ 2), while eight patients were disabled (mRS>2).In four patients, the ACE 068 reperfusion catheter was used as the first-line device without balloon guiding, and the DVO was successfully recanalized using the Trevo 4 × 20 mm via the modified STR technique. Overall, the primary LVO was fully recanalized, with mTICI 2a achieved in 33.3% (8/24) of patients and mTICI 2b achieved in 66.7% (16/24) of patients, with the condition being influenced by the presence of DVO in all cases. The modified STR technique for secondary DVO showed favorable outcomes, with a low number of procedural runs (mean 1.4 ± 0.6 times; range, 1–3) and achieved successful recanalization with TICI ≥ 2c in 95.8% (23/24) of patients, with a first-pass recanalization rate of 70.8% (17/24).
| Procedural time | Mean±SD (min) |
|---|---|
| Time from symptom onset to door | 70 ± 54 |
| Time from symptom onset to femoral puncture | 110 ± 82 |
| Time from femoral puncture to final recanalization | 63.6 ± 12 |
| Primary LVO | 45.5 ± 17 |
| Secondary DVO | 23.2 ± 14 |
Note: LVO- Large Vessel Occlusion; DVO- Distal Vessel Occlusion
Table 2: Time metrics of endovascular thrombectomy.
In terms of overall time metrics, the average time from symptom onset to hospital admission was 70 ± 54 min. The time from symptom onset to femoral puncture for the procedure was on average 110 ± 82 min. The mean recanalization time was 63.6 ± 12 min, with 45.5 ± 17 min for primary LVO cases and 23.2 ± 14 min for secondary DVO cases (Table 2). During the removal of the secondary clot, four instances of vessel spasms and one case of dissection occurred, with no vascular perforation observed. The vessel spasms spontaneously resolved, but the dissection eventually led to occlusion after the procedure. Asymptomatic ICH was observed in six patients on post-procedural CT, consisting of minor Parenchymal Hematoma type 1 (PH1) in four patients and subarachnoid hemorrhage in two patients, with no neurological deterioration noted. A routine follow-up MRI within 24–48 hours was performed for all patients. The presence of local ischemic findings was correlated with the recanalization of DVO, resulting in complete infarction in eight cases, partial infarction in three cases, and no infarction in 13 cases. At the 3-month mark, 16 patients had mild neurological sequelae (mRS ≤ 2), while eight patients were disabled (mRS>2).
Illustrative cases
Case 1 (Patient 5): A 67-year-old woman presented with suddenonset left-sided weakness and facial palsy, with an NIHSS score of 10. Initial CT revealed an ASPECTS of 8, whereas multiphase CTA revealed complete occlusion of the right ICA trunk with moderate collateral grade. Intravenous (IV) tPA was administered but proved ineffective. After continuous IV sedation, a 9 Fr balloon guide catheter was immediately placed at the proximal ICA. Using the ACE68 aspiration catheter with Trevo XP Provue 4 × 20 mm stent, successful recanalization of the distal ICA occlusion was achieved. However, a migrated embolus occurred at the right superior trunk of the M2 segment. The Trevo XP Provue 4 × 20 mm was immediately navigated to the DVO, and the modified STR technique was successfully applied to the migrated embolus, with full restoration of the blood flow as mTICI 2c Subsequent MRI the next day showed a minor infarction in the internal capsule. At the 3-month follow-up, the patient had mild left-side weakness and a mRS score of 1 (Figure 2).
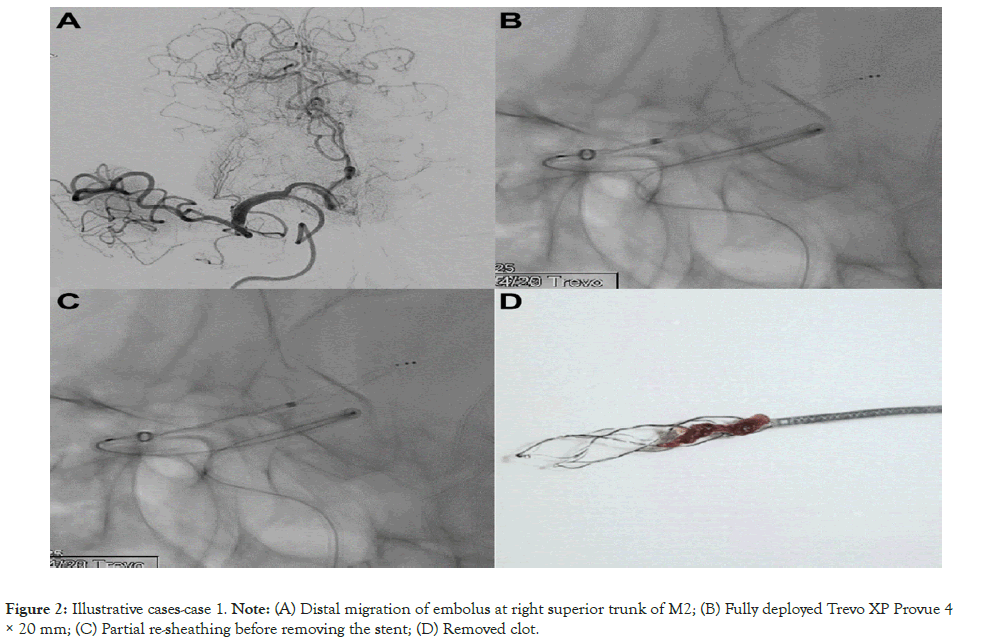
Figure 2: Illustrative cases-case 1.
Note: (A) Distal migration of embolus at right superior trunk of M2; (B) Fully deployed Trevo XP Provue 4× 20 mm; (C) Partial re-sheathing before removing the stent; (D) Removed clot.
Case 2 (Patient 14): A 59-year-old man presented with suddenonset left-sided weakness with a National Institutes of Health Stroke Scale (NIHSS) of 8. Initial CT showed an Alberta Stroke Program Early CT Score (ASPECTS) of 9, whereas multiphase CTA revealed right M1 trunk occlusion with good collateral grade. Given that the symptom onset was greater than 4.5 hours, IV tPA was not administered. An 8 Fr balloon guide catheter was immediately placed at the right proximal ICA, and using a Solitaire Platinum 4 × 20 mm stent, recanalization of the right M1 occlusion was successfully achieved. During retrieval of the stent, new embolic migration occurred in the right A3 trunk. Continuously, the modified STR technique was applied to the targeted vessel using the same Solitaire stent, and the DVO was successfully recanalized to TICI 3. Procedure-induced vasospasm spontaneously resolved without sequelae. On the MRI taken the following day, a small infarction was noted in the left basal ganglia, insular, and frontal lobe area. At the three-month mark, the patient had recovered, with a mRS score of 2, indicating minimal speech disturbance (Figure 3).
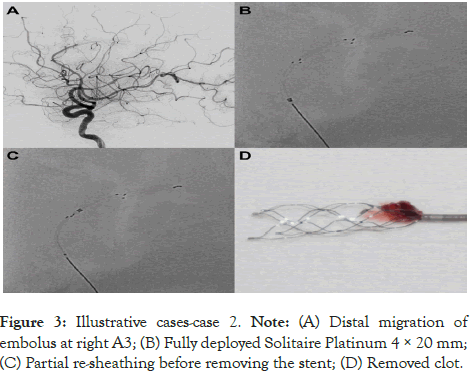
Figure 3: Illustrative cases-case 2.
Note: (A) Distal migration of embolus at right A3; (B) Fully deployed Solitaire Platinum 4 × 20 mm; (C) Partial re-sheathing before removing the stent; (D) Removed clot.
In this retrospective study, we examined the safety and effectiveness of a modified Short Tandem Repeat (STR) technique for removing migrated emboli in the M2, M3, A2, and A3 segments during mechanical thrombectomy for acute LVO. Although a prospective randomized study has not yet conclusively established the safety and effectiveness of mechanical thrombectomy beyond the proximal segment, the American Heart Association and American Stroke Association (AHA-ASA) currently recommend it as a viable treatment option for selected patients. This recommendation is based on evidence from subgroup analyses of five randomized trials and meta-analyses [8,20]. Some studies have also suggested that untreated distal occlusions could progress into significant ischemic areas [4,6-8,21]. Interestingly, recent reports have demonstrated favorable outcomes with a higher reperfusion rate in distal arterial occlusions, such as M2-3, A2-3, and P2-3, using smaller instruments and experienced techniques. These reports did not show statistical differences in procedure-related complications, such as symptomatic ICH, vascular dissection, or perforation, compared to the treatment of proximal occlusions. Furthermore, they indicated clinical improvement by achieving better TICI scores through effective treatment of DVO [11- 13,15,20].
Refining the approach to secondary DVOs that manifest during a procedure is important, given their conceptual distinctions from primary DVOs. Despite these differences, secondary DVOs often manifest with severe clinical symptoms, aggravated neurological deficits, larger ischemic extents, and increased clot fragility [10]. In a pioneering meta-analysis of safety and efficacy outcomes related to mechanical thrombectomy involving STR and aspiration in secondary DVOs, Rodriguez-Calienes, et al. examined data from 14 studies encompassing 291 patients. Their findings revealed favorable outcomes, with a successful reperfusion rate (mTICI, ≥ 2b) of 82% and a symptomatic ICH rate of 6% [22].
Liu and colleagues identified a distinctive interaction between thrombus and stent retriever in the context of utilizing primary stents for DVOs and observed that the connection is superficial rather than the thrombus merging into the stent retriever, particularly when the embolus partially extends into the stent through its mesh [6]. In such cases, the stent, with its smaller diameter and narrower mesh, grips the embolus during partial retrieval. In our modified STR approach for local DVOs, the primary objective is to reduce the frictional force between the stent and the parent artery, minimizing the risk of vascular injury during the procedure. We recommend using stents like Trevo ProVue 4 × 20 mm and Solitaire Platinum 4 × 20 mm for vessels with a diameter of 2 to 4 mm. However, when applied in vessels with a diameter of 2 mm or less, retrieving the entire stent with its original radial force can often induce traction or shearing stress on the targeted vessels. Considering that migrated clots in distal vessels are usually fragmented into smaller sizes than primary clots, the radiopaque property of these stents allows operators to control friction at the M2 to M3 and A2 to A3 segments by adjusting the covering length of the microcatheter. After fully deploying the stent at the DVO to enhance clot entrapment, the microcatheter can be re-sheathed while providing local compression on the stent, confirmed by jammed resistance in the retrieval system.
The deployment of low-profile stents and aspiration catheters, such as Baby Trevo, Catch Mini, various intermediate catheters, and Penumbra 3 or 4 Max, has shown potential outcomes in terms of both successful recanalization rates and one-pass success rates in cases of DVO [11-13,20,23]. Consistent studies have reported a meaningful success rate in vascular recanalization (TICI ≥ 2b), approximately ranging from 76%–85%. This underscores the efficacy of these low-profile devices in effectively reopening obstructed blood vessels. Furthermore, the one-pass success rate, indicating successful vascular recanalization in a single attempt using these devices, has been reported to be approximately 48%– 60%. In a comparative analysis of favorable outcomes associated with these innovative low-profile devices in DVO treatment, our research reveals highly comparable and, in some respects, more impressive results. Specifically, it demonstrated a significantly higher success rate of mTICI 2c-3 reperfusion, accomplishing this outcome in 23 of 24 patients (95.8%) at the final recanalization stage, coupled with a superior one-pass success rate of 70.8%.
Based on the available data, the reported rates of complications associated with supplementary procedures for secondary DVO align with findings from previous thrombectomy investigations [22,24-26]. Specifically, procedure-related vascular injuries have been reported in approximately 1–2% of cases, while postprocedural hemorrhagic tendencies have been observed in 4% of instances. Notably, this study identified the incidence of vessel spasm and dissection to be less than 1%, with these complications effectively addressed without resulting in severe consequences. Moreover, severe hemorrhagic changes linked to the procedure were also found to be less than 1%, indicating a low risk of significant bleeding complications. The occurrence of asymptomatic ICH was relatively rare, and importantly, no instances of neurological deterioration were observed in the patients. These findings robustly support the contention that the modified STR procedure represents a generally safe option, characterized by low complications and a favorable risk profile.
When restoring blood flow to salvage brain tissue within an appropriate timeframe, the overall vascular distribution plays a important role in determining the extent and progression of cerebral infarction [27,28]. Several studies have reported that the initial status of collateral circulation significantly influences the size and scope of cerebral infarction, as well as the ultimate clinical outcomes following mechanical thrombectomy [29,30]. In the 24-hour follow-up diffusion-weighted image results assessing the occurrence of cerebral infarction after modified STR, individuals with good collateral status (8 cases) experienced partial infarction in 1 case, those with moderate collateral status (9 cases) exhibited partial infarction in 1 case, complete infarction in 2 cases, and those with poor collateral status (7 cases) had partial infarction in 1 case and complete infarction in 6 cases. At the 3-month followup, neurologically favorable outcomes were observed in 12 out of 13 cases without local infarction, 2 out of 3 cases with partial cerebral infarction, and 2 out of 8 cases with complete cerebral infarction. This suggests that, under certain circumstances with favorable initial collateral circulation, additional intervention with modified STR for DVO may lead to improved clinical outcomes.
Furthermore, it offers advantages in terms of efficient time management and cost-effectiveness. Reported average procedural times for small-profile stents ranged from approximately 70–80 min, while aspiration catheters with a small diameter demonstrated procedural times of approximately 42–67 min for primary DVO [11-13,31]. In this specific context, the average procedure time for the modified STR technique was 23.2 ± 14 min, indicating a notably shorter duration compared to previous results targeting DVOs. These variations naturally depend on the preparation of the guiding and additional devices. Essentially, the stent initially employed for LVO can be utilized for secondary DVO without the need for additional tools. This repetitive use not only provides financial benefits to specific patients but also offers a practical solution for DVO, particularly in countries with limited reimbursement policies for available devices.
The modified STR technique showed remarkable success in achieving mTICI 2c-3 reperfusion, with a high rate of 95.8% and minimal occurrence of severe complications. Additionally, we achieved a one-pass rate of 70.8%, surpassing the rates reported with other small devices. These results provide strong evidence for the safety and effectiveness of the modified STR technique in effectively resolving DVO caused by migrated emboli.
First, the retrospective design and relatively small sample size limit the generalizability of our findings. However, it is important to note that all data related to angiographic or clinical outcomes were prospectively registered in a core lab, ensuring the validity of the collected information. Second, the decision to perform the modified STR technique at the new embolic territory was based on the discretion of each neurointerventionalist, which may introduce a selection bias. Nonetheless, it is worth mentioning that all physicians involved in the study had extensive experience in performing mechanical thrombectomy for over 10 years, and the technique was a consensus among them in similar situations. Although the modified STR technique demonstrated promising application and reliable results for secondary migrated emboli beyond the proximal segment, further investigation is warranted to assess its specific benefits. Prospective comparisons with smallprofile devices in primary DVO cases would provide a more comprehensive understanding of its efficacy and safety.
Author contributions
Conceptualization: Lead (author 1), Supporting (author 4) Data curation: Lead (author 1), Supporting (author 4) Formal analysis: Lead (author 1), supporting (author 2,3) Funding acquisition: Lead (author 4), supporting (author 5) Investigation: Lead (author 1), supporting (author 2,3,4) Methodology: Lead (author 1), supporting (author 2,3) Project administration: Lead (author 4), Supporting (author 1) Resources: Lead (author 4), Supporting (author 5) Software: Lead (author 1), Supporting (author 2,3,4,5) Supervision: Lead (author 4), supporting (author 5) Validation: Lead (author 3), supporting (author 2) Visualization: Lead (author 1) supporting (author 3) Writing–original draft: Lead (author 1), supporting (author 4) Writing–Review and editing: Lead (author 1), Supporting (author 5)
Statements and declarations
This retrospective study was approved by the local institutional review board, and all participants provided informed consent. (IRB number: KANGDONG 2023-07-010) All procedures in studies involving human participants were performed in accordance with the ethical standards of the institutional and/or national research committee and the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
The authors confirm that the data supporting the findings of this study are available within the article. Raw data that support the findings of this study are available from the corresponding author upon reasonable request.
This study was supported by the Hallym University Research Fund (Grant number: H20191021).
All procedures in studies involving human participants were performed in accordance with the ethical standards of the institutional and/or national research committee and the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent was obtained from all study participants.
The authors declare no conflicts of interest related to the content of this article.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Ahn HS, Park JH, Ahn JH, Jeon HJ, Cho BM (2024). Resolving Distal Vessel Occlusions Caused by Migrated Emboli: Outcomes of Modified Stent Retrieval Technique. Angiol Open Access. 12:480.
Received: 08-Jul-2024, Manuscript No. AOA-24-32713; Editor assigned: 11-Jul-2024, Pre QC No. AOA-24-32713 (PQ); Reviewed: 25-Jul-2024, QC No. AOA-24-32713; Revised: 01-Aug-2024, Manuscript No. AOA-24-32713 (R); Published: 08-Aug-2024 , DOI: 10.35841/2329-9495.24.12.480
Copyright: © 2024 Jeon HJ, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.