Pediatrics & Therapeutics
Open Access
ISSN: 2161-0665
ISSN: 2161-0665
Case Report - (2023)Volume 13, Issue 5
Pyloric atresia is a rare entity, especially in association with epidermolysis bullosa, of autosomal recessive transmission. The diagnosis is based on genetic study, the treatment of atresia is surgical according to the anatomical type of atresia. We report a rare case of pyloric atresia type 1 with skin involvement type epidermolysis bullosa with all the difficulties of follow-up and diagnosis in a country with limited resources.
Pyloric atresia; Epidermolysis bullosa; Respiratory distress
Pyloric Atresia (PA) is a rare congenital gastric obstruction and disease, accounting for less than 1% of bowel atresia. Its estimated incidence is approximately 1 in 100,000 live births [1]. Pyloric atresia manifests in three types: Type 1, characterized by a pyloric diaphragm or membrane; Type 2, where the pyloric tissue is replaced by a solid structure; and Type 3, which involves a gap between the stomach and pyloric region [2]. Furthermore, pyloric atresia is often accompanied by other bowel and nonbowel conditions, with skin involvement, such as epidermolysis bullosa, being the most frequently reported association [3]. In this report, we present a case of pyloric atresia associated with epidermolysis bullosa, which was initially identified due to respiratory distress in a preterm new-born.
A 2330 g girl was born through normal delivery at 36 weeks of gestation. The pregnancy was complicated by gestational diabetes and resulted from a first-degree consanguineous marriage. The mother had previously experienced two miscarriages, and a premature baby had passed away at 15 days old. The girl was admitted to our hospital due to respiratory distress, accompanied by episodes of non-bilious vomiting. Upon physical examination, initial findings revealed skin fragility, but no abdominal distension was observed. Meconium was passed. A plain abdominal X-ray displayed a dilated stomach, with no presence of gas in the bowel (Figure 1). A barium enema confirmed significant gastric stasis (Figure 2). The baby underwent surgery with a diagnosis of pyloric atresia type 1. Postsurgery, the baby girl rapidly developed tense vesicles, scattered areas of erosion, and bullae, affecting various parts of her body, including the hands, nails, mouth, and vulva (Figure 3). Following a dermatological examination, the diagnosis of epidermolysis bullosa was made without the need for a skin biopsy. The baby remained intubated for three days after the surgery, and subsequently, extubation took place. Oxygen therapy and physiotherapy were administered due to the presence of epidermolysis bullosa and bronchial secretions. Antibiotics were prescribed, resulting in a notable improvement. Breast milk feeding was initiated, but the patient experienced abdominal distension with gastric stasis despite effective but limited transit. The plain abdominal x-ray appeared normal. After three weeks of hospitalization, the baby was discharged with a favourable clinical course and was scheduled for regular clinical check-ups and respiratory physiotherapy. Genetic testing for genetic counselling and postnatal diagnosis could not be performed due to its unavailability in our hospital. The subsequent progression was marked by recurrent respiratory infections and the infant's underweight status, falling below-3 standard deviations. Unfavorably the infant passed away at 13 months of age.
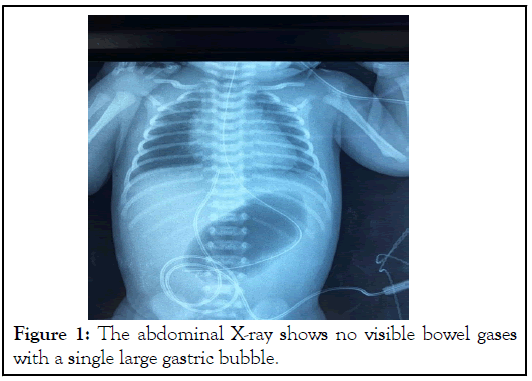
Figure 1: The abdominal X-ray shows no visible bowel gases with a single large gastric bubble.
Figure 2: The barium enema confirmed significant gastric stasis.
Figure 3: Epidermolysis bullosa lesions.
Pyloric atresia is a rare disease, accounting for less than 1% of gastrointestinal atresia [2-4]. The exact etiology of pyloric atresia remains unknown, but it is believed to result from developmental arrest between 5 and 12 weeks of intrauterine life [4-8]. Prenatal diagnosis is possible through third-trimester ultrasound, which may reveal hydramnios, a single gastric dilation, and the absence of a double gastric bubble appearance [9,10]. However, in our context, prenatal follow-up and antenatal diagnosis were lacking in all hospital centers. The clinical manifestations of pyloric atresia typically include non-bilious vomiting in the early days of life, intrauterine growth retardation, and abdominal distension. However, the clinical presentation can go unrecognized, and diagnosis may only occur following respiratory complications such as pulmonary infection, sepsis, or even post-mortem death [2,11-13]. The diagnosis is easily made through plain abdominal X-rays, which reveal a large single air bubble without gas distally [9,12]. Various classifications exist for pyloric atresia, including anatomical classifications (Types 1, 2, and 3) and clinical classifications based on whether pyloric atresia is isolated or associated with other abnormalities, such as gastrointestinal abnormalities or agenesis of the gall bladder. Additional associations have been reported, including genital and urinary tree abnormalities, cardiac and skeletal abnormalities, dysmorphism, and neurological abnormalities. Pyloric atresia is also associated with skin and genetic abnormalities such as Epidermolysis Bullosa (EB) or congenital skin aplasia [2,13-16]. Epidermolysis bullosa is a rare genodermatosis characterized by structural fragility of the skin, leading to blister formation. Its prevalence and incidence are difficult to determine [17]. EB is classified based on the level of blister formation in the skin, including EB simplex (EBS), Junctional EB (JEB), Dystrophic EB (DEB), and Kindler syndrome [18]. The association between pyloric atresia and epidermolysis bullosa is well-documented, with autosomal recessive transmission [19]. Pyloric atresia is often associated with the junctional form of epidermolysis bullosa, resulting from altered expression of α6β4 integrin. Recently, an association with the simplex form, caused by altered expression of plectin, has also been described. Altered expression of α6β4 integrin is attributed to homozygous or compound heterozygous mutations in the ITGA6 and ITGB4 genes [19-20]. Histopathological examination reveals the level of blister formation (intraepidermal for EB simplex and intra-lamina lucida for junctional EB), while immunohistochemistry confirms the diagnosis by revealing reduced or completely absent expression of α6β4 integrin or plectin [19,20]. There is no definitive treatment for EB with pyloric atresia, and management is mainly symptomatic, involving the use of dressings, antiseptics, and healing creams. Topical steroids can be used to manage inflammation. Pyloric atresia requires surgical treatment, depending on the anatomical type. Although some cases with a good prognosis have been reported, the overall prognosis of this disease is poor due to skin infections, sepsis, and visceral complications. The majority of children do not survive beyond one year, with the EB simplex subtype considered to be lethal [17,20].
Pyloric atresia is a rare disease, especially in association with epidermolysis bullosa. The diagnosis of epidermolysis bullosa and pyloric atresia is clinical, paraclinical, histopathological and immunohistochemical. There are no definite modalities in the treatment and the prognosis is poor, the majority of children die before first year. Hence the importance of follow-up pregnancies, prenatal diagnosis, and genetic counselling.
We have no conflicts of interest to disclose.
[Crossref] [GoogleScholar] [PubMed]
[Crossref] [GoogleScholar] [PubMed]
[Crossref] [GoogleScholar] [PubMed]
[GoogleScholar] [PubMed]
[Crossref] [GoogleScholar] [PubMed]
[Crossref] [GoogleScholar] [PubMed]
[Crossref] [GoogleScholar] [PubMed]
[Crossref] [GoogleScholar] [PubMed]
[Crossref] [GoogleScholar] [PubMed]
[Crossref] [GoogleScholar] [PubMed]
[Crossref] [GoogleScholar] [PubMed]
[Crossref] [GoogleScholar] [PubMed]
[Crossref] [GoogleScholar] [PubMed]
[Crossref] [GoogleScholar] [PubMed]
[Crossref] [GoogleScholar] [PubMed]
[Crossref] [GoogleScholar] [PubMed]
[Crossref] [GoogleScholar] [PubMed]
[Crossref] [GoogleScholar] [PubMed]
Citation: Mariam E, Widade K, Moustapha H (2023) Respiratory Distress Revealing Pyloric Atresia with Epidermolysis Bullosa. Pediatr Ther. 13:523.
Received: 04-Sep-2023, Manuscript No. PTCR-23-26532; Editor assigned: 06-Sep-2023, Pre QC No. PTCR-23-26532 (PQ); Reviewed: 20-Sep-2023, QC No. PTCR-23-26532; Revised: 27-Oct-2023, Manuscript No. PTCR-23-26532 (R); Published: 04-Oct-2023 , DOI: 10.35841/2161-0665.23.13.523
Copyright: © 2023 Mariam E, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.