Angiology: Open Access
Open Access
ISSN: 2329-9495
ISSN: 2329-9495
Case Report - (2022)Volume 10, Issue 4
Background: Acute limb ischemia is a serious condition even in an era of highly comprehensive medical treatment. Despite the development of conservative and endovascular treatment, complete removal of the thrombus with antegrade thrombectomy via the femoral approach, especially in below-the-knee arteries, is still not possible. In addition, distal embolization of dislodged debris or thrombus during the procedure is another concern as this might cause severe complications, including amputation. Given the above-mentioned issues, retrograde surgical cut-down direct thrombectomy from the dorsalis pedis artery and posterior tibial artery could be an optimal option for complete revascularization in below-the-knee arteries.
Case presentation: We present one case where the limb was preserved after retrograde surgical thrombectomy. The standard antegrade thrombectomy procedure with a conventional surgical approach from the common femoral artery was performed. The patient underwent an intraoperative assessment of indications for dorsalis pedis artery and posterior tibial artery retrograde thrombectomy by the surgical cut-down method. After retrograde thrombectomy, direct evaluation of blood flow was the strongest evidence of revascularization. A retrograde angiogram showed revascularization of below-the-knee arteries. The patient had successful salvage procedures that prevented major limb amputation.
Conclusion: Retrograde surgical thrombectomy could be a salvage procedure for incomplete antegrade thrombectomy.
Acute limb ischemia; Retrograde surgical thrombectomy; Open thrombectomy
ALI: Acute Limb Ischemia; BTK: Below-The-Knee; CFA: Common Femoral Artery; SFA: Superficial Femoral Artery; PAD: Peripheral Artery Disease; DUS: Duplex Ultrasonography; CTA: Computed Tomography Angiography; PTA: Posterior Tibial Artery; TP: Tibioperoneal; ATA: Anterior Tibial Artery; DPA: Dorsalis Pedis Artery.
Acute Limb Ischemia (ALI) is a limb-threatening disease that has a poor prognosis if quick and appropriate treatment is not administered [1-3]. Treatment includes conventional surgical thrombectomy, bypass, and endovascular revascularization, or a hybrid procedure [2,4-6]. However, the amputation rate has remained high at approximately 5% to 12% [4,6]. Aside from delayed diagnosis and treatment, another reason for a poor outcome is the incomplete restoration of perfusion in Below- The-Knee (BTK) arteries mostly induced by propagation of the thrombi, which are difficult to remove via an antegrade approach from the Common Femoral Artery (CFA) [6-8]. The retrograde approach with surgical cut-down is a novel and effective option for limb salvage. Here, we present one case of ALI that underwent an emergency operation with incomplete antegrade thrombectomy followed by successful retrograde thrombectomy. The patient’s leg was finally preserved without any amputation.
A 62-year-old male patient with nasopharyngeal carcinoma, who was under radiation therapy, was admitted to the emergency room due to sudden onset left whole leg numbness with weakness. The patient was a heavy smoker. The problem was initially considered as a stroke, and treatment was delayed beyond the ideal time. Upon consultation, cyanotic changes were found on the left first and second toes, which progressed to the sole near the ankle. While electrocardiography showed normal sinus rhythm, Computed Tomography Angiography (CTA) revealed a mural thrombus in the distal aorta and an occlusion over the left iliac artery to the proximal Superficial Femoral Artery (SFA) (Figures 1A and 1B). There was no flow recanalization on the BTK arteries.
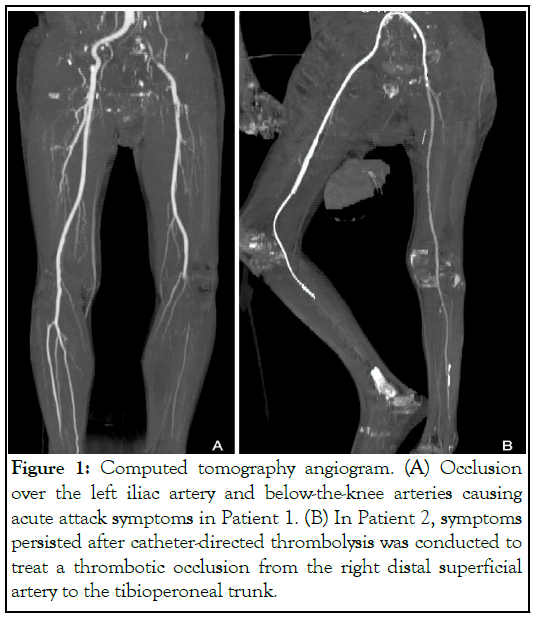
Figure 1: Computed tomography angiogram. (A) Occlusion over the left iliac artery and below-the-knee arteries causing acute attack symptoms in Patient 1. (B) In Patient 2, symptoms persisted after catheter-directed thrombolysis was conducted to treat a thrombotic occlusion from the right distal superficial artery to the tibioperoneal trunk.
The patient underwent an emergency open thrombectomy. Under general anaesthesia and before we performed a left CFA cutdown, routine bedside sonography showed a thrombus in the distal Anterior Tibial Artery (ATA) and Posterior Tibial Artery (PTA). We first performed a thrombectomy proximal to the aorta with a python over-the-wire embolectomy catheter. Then, we passed the guidewire anterogradely as far as possible to the Tibioperoneal (TP) trunk, performed thrombectomy again, and removed as much distal thrombus as we could. However, antegrade angiography revealed a residual thrombus distally and an occlusion over the proximal ATA and distal PTA (Figures 2A and 2B).
Figure 2: Intraoperative angiogram. (A) Only the peroneal artery below the knee was patent with occlusion in the orifice of the anterior and posterior tibial arteries before treatment. (B) After antegrade thrombectomy, occlusion was still present in the proximal anterior and distal posterior tibia arteries. This is one of the indications for retrograde surgical cut-down direct thrombectomy.
We used the surgical cut-down approach on the Dorsalis Pedis Artery (DPA) and PTA and performed retrograde thrombectomy via a 3F Fogarty catheter under a 0.035 inch guidewire support. After successful revascularization, pulses were detected in both the DPA and PTA. The wound was closed layer by layer after final retrograde angiography showed no specific stenotic lesion that needed to be treated (Figures 3A-3D).
Figure 3: Retrograde angiography performed after retrograde thrombectomy. (A,B) Bi-directional angiograms of the posterior tibia artery and (C,D) the anterior tibial artery was obtained to ensure complete revascularization.
Within the post-operation period, reperfusion injury occurred, which was treated with hydration and acidosis correction. Though fasciotomy is avoided in this hospital, transmetatarsal amputation was performed on the left foot in the outpatient clinic due to the development of dry gangrene. The patient was treated with oral aspirin (100 mg once daily), cilostazol (50 mg twice a day), and rivaroxaban (2.5 mg twice daily). Major amputation was prevented, and the patient can now walk by himself.
ALI is a critical medical condition due to embolic ischemia or thrombotic occlusion [1]. The incidence is approximately 1.5 cases per 10,000 persons per year. Despite prompt surgery and advancements in techniques, there are still poor outcomes. Within 30 days post-operation, 15% of ALI cases result in amputation. The mortality rate in one year is approximately 20% [4,6].
Immediate diagnosis and rapid revascularization are important, but incomplete restoration of perfusion should always be considered, especially in BTK arteries. It is difficult to completely remove the thrombus present within the tibial artery, where the embolectomy catheter or guidewire cannot pass through easily, or there is propagation of the thrombi related to the thrombectomy causing a poor outcome [7-9].
Conventional open thrombectomy or endovascular intervention cannot always completely remove thromboembolism [8]. Up to 30% of procedures may demonstrate residual thrombus in a large fraction of vessels on an angiogram. The essential step is the advancement and crossing of the guidewire through the lesion. It should be performed carefully without causing an intimal flap. However, procedural failure occurs in up to 20% of the cases, even when performed by experienced surgeons [9].
Retrograde surgical cut-down direct thrombectomy could be an effective method to deal with this problem, especially when the embolic lesion is found in BTK arteries. The indications for our proposed technique include the following: 1) Failure of guidewire passage into BTK arteries, 2) Incomplete revascularization with a poor flow rate of ATA and PTA on angiogram, 3) No flow detected by intraoperative bedside sonography after revascularization, and 4) Thrombotic occlusion of BTK arteries documented by preoperative sonography. The patient presented here had one or more of the indications mentioned above.
Figures 4A-4E shows the procedural details of this approach. First, we used antegrade thrombectomy with a conventional surgical approach from CFA. This is considered the best method for removal of a large thrombus in ALI [6,7]. After antegrade thrombectomy, all patients received an intraoperative assessment. Retrograde thrombectomy by the surgical cut-down method was indicated if any criteria matched. Then, direct reanastomosis of CFA was done. Second, one or both DPA and PTA dissection was performed, followed by arteriotomy. A 2F Fogarty catheter was used for embolectomy with guidewire support [10,11]. Direct evaluation of the blood flow was the strongest evidence of revascularization. Then, a retrograde angiogram provided us the whole picture of BTK arteries, indicating whether there were residual thrombi or stenotic lesions, which may need balloon angioplasty. After we finished re-anastomosis of the DPA and PTA, complete angiography was performed as a final check.
Figure 4: Procedure for retrograde surgical cut-down direct thrombectomy. (A,B) A direct approach is made to the target vessel, such as the dorsalis pedis or posterior tibia artery. (C,D) After open retrograde thrombectomy and re-anastomosis of the vessels, bedside duplex ultrasonography can be used to detect blood flow. (E) Finally, the wound is closed layer by layer.
Although the development of endovascular treatment showed evidence of good outcomes in BTK thrombotic occlusion even with a retrograde method, we considered direct surgical thrombectomy for ALI as the better treatment. Aside from the optimal assessment of blood flow, the endovascular approach could not remove the thrombus completely as with open surgery. The residual thrombus might become a distal embolic occlusion, which may increase the risk for amputation or may adhere to the vessel wall after balloon angioplasty, which could be a risk for critical limb-threatening ischemia. There was no better way other than direct removal of the thrombus.
In conclusion, retrograde surgical thrombectomy could be a salvage procedure for incomplete antegrade thrombectomy. In this case presented here, the limb of the patient was successfully salvaged after the combination of antegrade and retrograde thrombectomy.
Our patient’s medical record review was approved by the Institutional Review Board of the Chang Gung Memorial Hospital. Our patient was fully informed about the nature of this report, and Informed Consent forms were signed by our patient.
Our patient was fully informed about the publication, and Informed Consent forms were signed by our patient.
YS-Li, the corresponding author, served as the director of the case report. YC-Lu, the first author, is a resident physician who cared for the patient.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Li YS, Lu YC (2022) Retrograde Surgical Cut-down Direct Thrombectomy as a Salvage Procedure for Acute Limb Ischemia Especially under the Knee Thrombotic Occlusion: A Case Report. Angiol Open Access. 10:289.
Received: 31-Oct-2022, Manuscript No. AOA-22-19000; Editor assigned: 02-Nov-2022, Pre QC No. AOA-22-19000 (PQ); Reviewed: 16-Nov-2022, QC No. AOA-22-19000; Revised: 23-Nov-2022, Manuscript No. AOA-22-19000 (R); Published: 30-Nov-2022 , DOI: 10.35248/2329-9495.22.10.289
Copyright: © 2022 Li YS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.