Journal of Infectious Diseases & Preventive Medicine
Open Access
ISSN: 2329-8731
ISSN: 2329-8731
Research Article - (2021)Volume 9, Issue 10
Background: Globally, patients with accidental brain injury are a considerable reason for the disability and death rate and very serious health problem among low-income nations including Ethiopia.
Objective: This study aimed to explore predictors of outcomes in traumatic brain injury patients at public hospitals, Addis Ababa, Ethiopia.
Methodology: A retrospective cross-sectional quantitative study design was employed from a total of 371 randomly selected patients’ chart with traumatic brain injury who was admitted (hospitalized) to the study hospitals of trauma center from January 01, 2019 to December 31, 2020, and data was gathered from February 25 and April 15, 2021.
Results: From a total of 371 study participants, 260 (70.1%) were males. One-third, 129 (34.8%) of injuries were age group of 25–34-year, one hundred seventy (42.3%) of the patients were from an urban setting. This finding reveals that 36% were unfavorable outcomes of accidental traumatic injured patients were arrived at the health care institutions within four to twenty-four hours and more than twenty-four hours were more likely to have unfavorable outcomes AOR=2.857 [1.150,7.099], and AOR=7.623 [2.594,8.915] respectively.
Conclusion: This study showed that severity of the injury, age, oxygen saturation level, pupillary reactivity, and time of arrival, are associated with patient outcomes of traumatic brain injury and recommended improving time of arrival, oxygen saturation level and information delivery system in the respective health institution.
Traumatic; Brain injury; Predictors; Public; Hospitals
ABET: Addis Ababa Burn Emergency and Trauma; CDC: Center for Disease Control; CT: Computer Topography; GCS: Glasgow Coma Scale; GOS: Glasgow Coma Outcome Scale; HT: Head Trauma; JUTH: Jimma University Teaching Hospital; RTA: Road Traffic Accident; TASH: Tikur Anbessa Specialized Hospital; TBI: Traumatic Brain Injury; USA: United States of America.
Background information
Traumatic Brain Injury (TBI) is a prevalent condition of high burden to society and affecting mainly young age group [1]. Traumatic Brain injury may predispose to the alteration of cognitive function results in both short and prolonged effect [2]. There are many ways to categorizes patients and each of them may impact of prognosis and treatment [3]. Traditionally TBI has been classified based on the severity using Glasgow Coma Scale. The degree of TBI is lead to mild to severe memory loss and may worthy physical and psychological impairments [4-6].
According to data from the CDC showing accidental brain injury in different African countries ranging from 150-500/100,000 per year [7,8]. In Africa, one-third of all head-injured patients suffer poor outcomes and those patients with a severe head injury have almost twice the risk of dying compared to those in high-income countries [8]. Standard health care service including patient education on prevention of accidental road traffic injury and emergency care may improves the outcome of Traumatic Brain Injury [9,10].
Accidental injury is a serious health care problem in all regions of Ethiopia [11,12]. Even if the Ethiopian road authority in collaboration with other governmental organization worked in development of policies and related strategies to reduce or control accidental traffic injury including initiation of public media to teach the public still remains major health care gaps in the nation [13].
Statement of the problem
Accidental injury is a major issue across the globe and a research study reveal that top ten deaths across the world about five million deaths recorded annually. In addition to Africa's high rate of injury and death, Egypt has the lowest rate. South Africa and Ethiopia were second and third, respectively [5]. Accidental injury is one of the main causes of disability across the globe as the result worldwide with enormous economic consequences [14]. Thirty percent of accidental injuries outcome is lead to death that indicated a literature review and high incidence in low-income countries [15,16].
A population-based study conducted in Urban Tanzania and Ghana has demonstrated that accidental injuries are the main cause’s anatomical and physiological disability [17,18]. A research study indicates in Ethiopia at institution of Jimma University hospital in 2010 reveal that accidental brain injury is a preventable community health problem of public at large [19,20].
Accidental brain injury indicates that one of a major community concern and controllable issues through identification of predisposing factors and appropriate public health intervention. And also understanding the outcomes of predictors is useful in making important decisions making process particularly helpful to manage methods of treatment for the health care professionals and in communication with the patient’s family [21]. The current assessment is aimed to explore the determinant factor of accidental brain injury outcomes of patient with TBI at Addis Ababa public Hospitals.
Significance of the study
The outcome of accidental brain injury is a considerable health institution challenge of every nation across the world. This study identifies key predictors of the outcomes of TBI that help in designing health education on the prevention of road traffic accidents, effective treatment strategies for TBI and this finding provides baseline information for other larger-scale studies. As a whole, the result of this study used public health workers, health service planners, community workers for planning and interventions to optimize management protocol both in the institutions and at the community level.
Conceptual framework
In this study, a conceptual framework is established after reviewing different literatures related to similar socio-demographic characteristics of the study population and identified variable as depicted in Figure 1 below. According to the literature, the outcomes of TBI can be predicted based on the socio-demographic status, history, clinical factors, and diagnostic results of the patient [22-24].
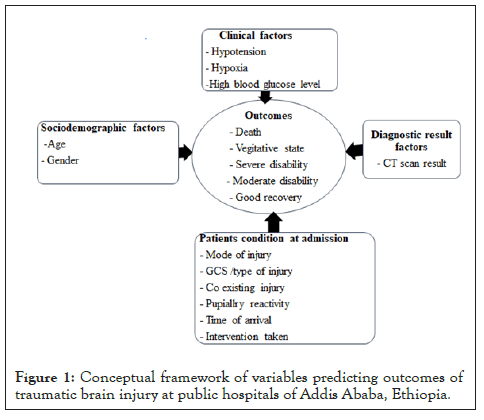
Figure 1: Conceptual framework of variables predicting outcomes of traumatic brain injury at public hospitals of Addis Ababa, Ethiopia.
Study setting
The assessment was undertaken at two randomly chosen public (governmental) institutions at capital city of Abet and Alert hospital at Ethiopia. Abet hospital is a 250 beds institution with 12 Intensive care unit beds and one of general public hospital in Addis Ababa city administration. Annually the hospital serves 5000-7000 patients.
Alert Hospital is another public hospital in Addis Ababa. The trauma center includes four rooms: Emergency, ICU, OR, and Surgical ward. In the third quarter of 2016, the center reported more than 1603 emergency visits. The trauma center is the first area hospital to have this designation [21].
Study design and period
A retrospective health care institution based cross-sectional study design was conducted to determine the predictor of accidental brain injury patients among selected health care institutions. The outcome of accidental brain injury assessment for survivors of data from the patients’ medical records who were admitted to the study hospitals for the period of January 01, 2019 to December 31, 2020 and data gathered from February 25 to April 15, 2021 using client’s charts.
Study participants
Clients who were admitted to the study health care institutions from January 01, 2019 to December 31, 2020.
Inclusion and exclusion criteria
Inclusion criteria: All records of TBI patients who were admitted to Abet and Alert health institutions were collected in January, 2019-December 2020, whose age was greater than 18 years.
Determination of sample size
Sample size was determined by a single population proportion formula by considering the following assumptions.
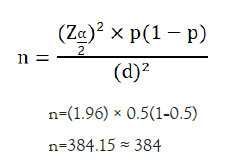
p=proportion of mortality (50%)
Z α/2=the corresponding Z score of 95% CI,
d=Margin of error (5%) and
n=required Sample size
Correction methods applied due to n<10000.
nf=Sample size
n=Desired sample size
N=Source population
Adding 10 % contingency rates and the final sample size 371.
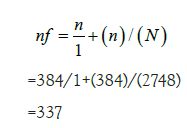
Sampling technique and procedure
The two trauma centers were selected based on the declaration of the Federal Ministry of health as trauma centers and high trauma patient flow. The Number of TBI patients within two years has taken and a sample size of three hundred seventy-one has been determined as shown in Figure 2 below. The samples were proportionally allocated to the two selected trauma center of hospitals and the data was collected by using a simple random sampling frame.
Figure 2: The samples were proportionally allocated to the two selected trauma center of hospitals and the data was collected by using a simple random sampling frame.
Identification of variables
DV: Outcomes of TBI
Independent variable: Age, Sex, Mechanism of head injury, GCS scale/Type of TBI, Time of arrival (time between injury and arrival), Interventions, co-existing injuries, hypoxia, hypotension, blood glucose level, pupillary reactivity and CT scan result.
Operational definitions
Anisocoria: It is the size of pupil varied or unequal in size due to various type of pathological problem or injury of the eye. Identified during patient assessment and helpful for clinical diagnosis.
Trauma: A term used in a physical sense as a wound or injury – such as a severe blow, which leads to a fracture.
Traumatic (accidental) brain injury: Disturbance or harm to brain anatomical or physiological changes in brain function caused by confusion, coma, seizure, etc.
Glasgow coma Outcome Scale (GCS): GCS applied for the examination of a neurological assessment of a client. The Glasgow coma outcome scale is applied to the examination in different conditions of the outcome of death and patient is certified dead in vegetative state; patient exhibits no obvious cortical function.
• Severe disability (conscious but disabled) patient depends upon others for daily support due to a mental or physical disability or both.
• Moderate disability (disabled but independent) patient is independent as far as daily life is concerned. The disabilities found include varying degrees of dysphagia, hemiparesis, or ataxia, as well as intellectual and memory deficits and personality changes.
• Good recovery: resumption of normal activities even though there may be minor neurological or psychological deficits.
• A positive outcome is defined as a Glasgow Coma Outcome Scale of IV or V. Unfavorable outcomes are graded on the Glasgow Coma Outcome Scale I-III.
Trauma: It is an anatomical and physiological damage of a body part as the result of accident injury.
Mild traumatic brain injury: In accordance with GCS from 13 to 15 head injury.
Moderate traumatic brain injury: In accordance with GCS from 6 to 13 head injury.
Severe traumatic brain injury: In accordance with GCS<8 [22-24].
Data extraction tools and procedures
The medical files of patients presented with TBI were retrospectively collected by using checklists. The guidelines list that was used for the assessment of the outcome was adopted from the Glasgow coma outcome scale (GOS). It has been widely accepted as a standard means of describing outcomes in head injury patients and has a high degree of validity (0.80%) and reliability (95%) [25,26]. The extraction tool for predictors was adopted and modified from different kinds of literature [22,27,28].
Procedure of data analysis
After data checked carefully, coded and entered into EPI data version 4.4 then export to Statistical Package for the Social Sciences (SPSS) 24 version to analyze. Before running simple and multiple linear regressions the data was tested to fit the model. Normality and linearity assumption was tested and it was satisfied. Multi categorical variables were coded into dummy variables. Multi-collinearity test was employed to test the correlation between independent variables. Variables which found association with the outcome variable at p<0.25 in simple linear regression were entered into multiple linear regressions to test for independent association. Crude beta and adjusted beta along with 95% Confidence Interval (CI) were calculated. P values below 0.05 were considered to be statistically significant.
Sociodemographic characteristics
A total of 2,748 patients admitted to the hospitals due to TBI. During the study period, 371 study participants’ charts were randomly selected. Of these, about 260 (70.1%) were males as depicted in Table 1 below, one third, 129 (34.8%) of injuries occurred among ages 25-34-year-old. One hundred seventy (42.3%) of the patients were from urban areas.
| Characteristics | Category | Frequency | Percentage (%) |
|---|---|---|---|
| Age | 18-24 | 82 | 22.1 |
| 25-34 | 129 | 34.8 | |
| 35-44 | 70 | 18.9 | |
| 45-54 | 40 | 10.7 | |
| ≥ 55 | 50 | 13.5 | |
| Gender | Male | 260 | 70.1 |
| Female | 111 | 29.9 | |
| Residency | Urban | 157 | 42.3 |
| Rural | 214 | 57.7 |
Table 1: Sociodemographic status of patients with traumatic brain injury in Alert and Abet hospitals (n=371).
Patients’ condition at admission
Accidental injury may predispose of TBI indicates 174 (46.9%), followed by assault 96 (25.9%) and fall down accident 73 (19.7%). In arrival time to the health care institution after injury, 141 (38%) patients were presented within the first 1-4 hours duration, 27.4% within 4-24 hours and 21% arrived in less than one hour. One hundred ten (29.6%) had a severe type of TBI in line with the score of the Glasgow coma scale. Among the 255 patients with co-existing injuries, 197 (77.3%) had skull injury. Among 371 study participants, a total of 201 (54.1%) patients had normal pupil reactivity and 239 (64.4%) of patients were treated conservatively.
Clinical and diagnostic factors
Information on patients’ vital sign was taken from medical records. Accordingly, 175 (47.1%), 246 (66.3%) and 211 (56.9%) of patients’ blood pressure, respiratory rate, and pulse rate was indicating within the normal range at the time of arrival respectively.
Outcomes of traumatic brain injury
Patients with traumatic brain injury outcome reveals that majority of the patients 71 (19.1%) were dead, 13 (3.5%) were in a vegetative state, 40 (10.7%) were severely disabled, 8 (2.1%) were referred, 62 (16.7%) were moderately disabled and 177 (47.7) had a good recovery.
Outcomes of traumatic brain injury
Outcomes of predictive factors of TBI with COR and AOR with 95% CI as shown in Table 2 below ages had more favorable outcomes. Time of arrival to the health care institution after injury, severity of TBI pupil reactivity, and oxygen saturation shows a statistically significant predictive value for unfavorable outcomes of TBI.
| Variables | Category | Outcomes | OR with 95% CI COR | p-value | OR with 95% CI AOR | p-value | |
|---|---|---|---|---|---|---|---|
| Age in years | FO | UO | |||||
| 18-24 | 64 | 18 | 0.172 (0.079, 0.374) | 0 | 0.067 (0.007, 0.622) | 0.018 | |
| 25-34 | 95 | 34 | 0.219 (0.110, 0.438) | 0 | - | ||
| 35-44 | 44 | 26 | 0.362 (0.171, 0.766) | 0.008 | - | ||
| 45-54 | 17 | 23 | 0.829 (0.355, 1.936) | 0.665 | - | ||
| ≥ 55 | 19 | 31 | 1 | 1 | |||
| Mechanism of injury | RTA | 79 | 95 | 4.409 (1.704, 11.410) | 0.002 | ||
| Assault | 77 | 19 | 0.905 (0.322, 2.542) | 0.849 | |||
| Fall down | 61 | 12 | 0.721 (0.322, 2.155) | 0.559 | |||
| Others | 22 | 6 | 1 | 1 | |||
| Time of arrival | >1 hour | 64 | 14 | 1 | 1 | ||
| 1-4 hour | 107 | 34 | 1.453 (0.725, 2.911) | 0.293 | |||
| 4-24 hours | 48 | 54 | 5.143 (2.562, 10.324) | 0 | 2.857 (1.150, 7.099) | 0.005 | |
| >24 hours | 20 | 30 | 6.857 (3.053, 15.39) | 0 | 7.623 (2.594, 10.399) | 0 | |
| Severity | Sever | 37 | 73 | 13.153 (7.178, 20.1) | 0 | 5.224 (2.562, 8.915) | 0 |
| Moderate | 62 | 38 | 4.086 (2.218, 7.528) | 0 | 2.851 (1.298, 6.262) | 0.009 | |
| Moderate | 62 | 38 | 4.086 (2.218, 7.528) | 0 | 2.851 (1.298, 6.262) | 0.009 | |
| Mild | 140 | 21 | 1 | 1 | |||
| Pupillary reactivity | Normal | 175 | 26 | 1 | 1 | ||
| Dilated | 34 | 58 | 11.48 (6.360, 20.72) | 0 | |||
| Anasorcia | 26 | 48 | 12.426 (6.615, 21.3) | 0 | 3.941 (1.766, 5.793) | 0.001 | |
| Unable to assess | 4 | 0 | - | 0.999 | |||
| Blood pressure | Increased | 43 | 33 | 7.626 (3.842, 15.13) | 0 | ||
| Decreased | 37 | 83 | 22.29 (11.711, 42.4) | 0 | |||
| O2 saturation | Normal | 190 | 42 | 1 | 1 | ||
| Hypoxia | 49 | 90 | 8.309 (5.129, 13.46) | 0 | 3.490 (1.845, 6.603) | 0.001 | |
| Hematocrit | <30% | 65 | 67 | 4.066 (2.188, 7.555) | 0 | ||
| >30% | 102 | 47 | 1.818 (0.976, 3.386) | 0.06 | |||
| Not investigated | 71 | 18 | 1 | 1 | |||
| Ct scan result | No ct | 41 | 0 | 0.028 (0.004, 0.213) | 0 0.997 | ||
| Normal ct | 42 | 0 | 0.027 (0.003, 0.207) | 0.997 | |||
| Hematoma | 14 | 92 | 4.200 (2.124, 8.305) | 0 | |||
| Brain contusion | 55 | 1 | 0.041 (0.009, 0.182) | 0 | |||
| Subarachnoid bleeding | 59 | 4 | 0.314 (0.145, 0.581) | 0 | |||
| Others | 28 | 35 | 1 | ||||
Note: FO: Favorable Outcome; UO: Unfavorable Outcome
Table 2: Bivariate and Multivariate logistic regression analysis of predictors of outcomes traumatic brain injury, Alert and Abet hospitals, Addis Ababa, Ethiopia (n=371).
The current study aimed to evaluate the predictors of the outcome TBI at study health care institution of Alert and Abet hospitals in Addis Ababa city administration. The study found that severity of TBI, arrival time after injury, reactivity of pupil, age and oxygen saturation were found to be predictors of TBI.
This study showed the outcome of patient with TBI, a considerable number of patients, 71 (19.1%) were dead. This result indicates less figure compared with a study done in Greece which reported 27.38% death among traumatic brain injury patients. The difference may be attributed to the severity of injury. The majority type of TBI in the current study is mild, which has a good recovery (43.3) compared to that of the study in Greece (37.03) [22]. It is also showed less unfavorable outcome compare to Kenyatta National Hospital, a tertiary referral center in Kenya which showed an unfavorable outcome of 83.8%. The difference may attribute the type of severe TBI has worsened outcomes [27].
The study showed that patients whose age younger than 25 years old was more likely to have favorable outcome compared to other age groups. The current study is matched with a study conducted in Greece indicates patients greater than 75 years old had not as good as outcomes compared with the youngest age group of patients [22]. This may be due to multi-factorial reasons that the aging brain seems more complex to ischemia and regenerative impaired capacity. It may also be due to much greater occurrence of elderly patients with chronic concomitant diseases.
This study also revealed that patients arriving 4-24 hours and greater than 24 hours had an unfavorable outcome compared to those who came in less than 4 hours. The current finding is comparable with a study conducted in Kenyatta National Hospital, at referral center in Kenya which showed patients who arrived between 4 and 24 hours after injury had high mortality rate.
The mortality in this study could be explained by greater incidence of numerous damages and delayed arrival of health care institutions [27].
The study finding showed the severe and moderate type of traumatic brain injury had a higher unfavorable outcome compared to a mild type of traumatic brain injury. The study showed similarity with a study done in Greece society which presented a high correlation between low GCS level and mortality [22]. This may be due to increased brain tissue damage with a moderate and severe type of traumatic brain injury.
This study finding showed patients with unequal pupil reactivity had unfavorable outcomes. It also showed patients who presented with hypoxia had an unfavorable outcome. This study shows similarity with a study done in Greece in which the death of clients indicates the ability to react pupils were very poor [22]. This elevated unfavorable outcome for both variables may be due to increased damage to the brain.
Study limitations
Current investigation was exposed to incomplete recorded data (variables) that are not included in the study and external validity of the result might be limited as the study included the trauma centers.
This study was done on outcomes and predictors of traumatic brain injury on Alert and Abet trauma centers. The result of this study showed that there were 36% of unfavorable and 64% of favorable outcomes. Young age is related to favorable consequences in accidental TBI patients, while immediate coming to health care institutions, the severity of the injury, pupillary reactivity, and oxygen saturation were associated with unfavorable outcomes among traumatic brain injury patients.
Governmental and non-governmental organizations have termed for action in response to the findings of this study. The identified predictors should be taken to under consideration by health care providers, concerned bodies, and policymakers of the trauma centers to plan an optimized management protocol. Since the main source of accidental injury is due to road traffic accident precautions should be taken to reduce the incidence of TBI related mortality both by pedestrian and Ethiopian transportation authority’s by focusing on the implementation of policies on the road traffic and educating all individuals and the Ethiopian Broadcasting service (the media) should work on policies and guide line to teach public at large.
The thesis was conducted as partial fulfillment of the requirement for postgraduate adult health nursing in Addis Ababa University supported for stationary item and paper binding cost only.
The authors strongly declare that we did not receive any fund in any institution and authors strongly declare that this thesis has not been submitted to any other institution or anywhere for the award of any academic certifications.in any fund in any intuitions or agency [28].
This paper presented as partial fulfillment of the requirement for the MSc degree from the school of post graduate Studies at AAU, School of Nursing and Midwifery. The thesis is deposited in the Library of Addis Ababa University is made available to the user under the rules of the university library. The authors strongly declare that this thesis has not been submitted to any other institution anywhere for the award of any academic certifications. The authors professed that they have no contending interest exist in this research study.
BN: data cu ration; formal analysis, interpretation of data and original drafting the article; ZA and TG: revising critically, editing and project administration and TH: conceptualization; revising critically for important intellectual content, editing and manuscript preparation. Final approval, all authors read and approved the final version to the submitted article.
Ethical clearance and approval were obtained from Institutional Review Board (IRB) of Addis Ababa University, College of Health Sciences, Department of Nursing approved with written letter and Permission was obtained from clinical director of each study hospitals, Matron and heads of the respective ward. After explaining the purpose of the study, possible benefit of the study and time to complete the questionnaire and why the participants are chosen, oral and written informed consent was obtained from each participant nurses before preceding the procedure. The participants were fully explained that they have the right not to participate in the study, to stop at any time in between or not to answer any questions they were not willing to answer. Confidentiality was maintained; no unauthorized person had access to the information and names or other identifiers were not recorded. All methods and subjects provided written consent, and the study was conducted according to the declaration of Helsinki.
Consent for publication
Not applicable.
Additional data available on the reasonable request from corresponding author.
Availability of data and materials
All relevant data are included with in the manuscript document. If it is necessary, it is possible to contact the corresponding author to get additional materials.
Citation: Nigussie B, Argaw Z, Gebreyohannis T, Habte T (2021) Retrospective Study on the Predictors of Outcomes in Traumatic Brain Injury Patients at Public Hospitals, Addis Ababa, Ethiopia. J Infect Dis Preve Med. 9: 241.
Received: 18-Nov-2021 Accepted: 02-Dec-2021 Published: 09-Dec-2021
Copyright: © 2021 Nigussie B, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.