Journal of Food: Microbiology, Safety & Hygiene
Open Access
ISSN: 2476-2059
ISSN: 2476-2059
Review Article - (2019)Volume 4, Issue 1
Food-borne; Gastroenteritis; Virulence; Epidemiology; Campylobacteriosis
Campylobacter species are Gram-negative, rod-shaped, spiral or curved bacteria with a flagellum single polar, bipolar, or no flagellum, depending on the species [1]. Campylobacter species do not form spores, having size of 0.2 to 0.8 by 0.5 to 5 m, and are chemoorganotrophs, amino acids or tricarboxylic acid cycle intermediates are the energy molecules [2]. Most Campylobacter species are micro aerobic and have a respiratory type of metabolism; however, several species (Campylobacter conscious, Campylobacter curves, Campylobacter rectus, Campylobacter mucosalis, Campylobacter showae, Campylobacter gracilis, and, to a certain extent, Campylobacter hyointestinalis) require hydrogen or formate as an electron donor for microaerobic growth. In addition, certain species prefer anaerobic conditions for growth.
The Campylobacter genus was demonstrated in 1963 following the renaming of Vibrio foetus to Campylobacter foetus, forming the type species of this genus [3]. The Campylobacter genus belongs to the family Campylobacteraceae, the order Campylobacterales, the class Epsilonproteobacteria, and the phylum Proteobacteria. Since its first description, this genus has grown to include several important human and animal pathogens that are primarily classified through phylogenetic means. The genus Campylobacter consists of 26 species, 2 provisional species, and 9 subspecies. In humans, Campylobacter species have known to cause a range of gastrointestinal infections, including inflammatory bowel diseases (IBD), Barrett’s esophagus, and colorectal cancer [1]. Campylobacteriosis is commonly characterized by gastroenteritis; it can also lead to septicemia, post-infectious arthritis, Guillain-Barré syndrome (GBS), or Miller Fisher syndrome [4]. Furthermore, Campylobacter species have recently been found to be associated with diseases such as Crohn’s disease and ulcerative colitis [5,6].
The major increase of both incidence and prevalence of campylobacteriosis in Europe, Australia and North America is worrisome, and data from Asia, Africa, and the Middle East shows that campylobacteriosis has become endemic in these areas, especially in young children [7]. The objective of this paper is to highlight the dreadful pathogen Campylobacter and more importantly emphasizing the pathogenic and virulence mechanisms. As it is a prevailing problem worldwide so, this attempt has been made to give a better look and understanding about its transmission. Moreover, review of literature and an epidemiological view from Pakistan is given to estimate Campylobacter infections rate as few data has been available from Pakistan. The prevention and treatment options to cope with Campylobacter infections are also discussed.
According to a report, infections cases caused by Campylobacter are 14 per year per 100,000 of population in United Sates of America [8]. The problem of infections has increased 30 times more reported by the data on an outbreak [9]. In a separate study, isolation and characterization of Campylobacter, 13 species out of 23 were found to be other than C. jejuni, C. coli or C. lari [10]. The transmission and spreading of Campylobacter infections found to have 42% prevalence rate, encountering traveling as the major culprit [11]. Reports from South America also highlighted its increased prevalence i.e. 4.6 to 30.1% in C. jejuni infections while from Argentina three studies showing 0 to 1.4% prevalence rate of C. coli. The range between 4.4 to 10.5% of C. jejuni infections reported from Bolivia. Moreover, C. jejuni cases were present at the range between 5.8-9.6% and of C. coli were 2.2-6.0%. The Campylobacter infections rate found in Chile ranged 0-14.1%, in Colombia 0-14.4%, in Ecuador 0-23.0%, in Paraguay 0.6-18.4%, in Peru 0-23.0%, in Uruguay 0-14.3% and in Venezuela 0-13.0% [12].
A report evaluation shows high rate prevalence of Campylobacter infections in Bulgaria i.e. 13,500 cases per 100,000 population while less incidences in Finland and Sweden [13]. The Rate of Campylobacter was 9.3% per 1000 cases per year in a report surveyed from United Kingdom and Campylobacter was found to be the major gastroenteritis causing bacteria [14]. According to report cases of campylobacteriosis infections ranged 2005-2011 found to be 53.4-81.4% per 100,000 of population in Germany [15]. In Paris year 1996-2007, level of campylobacteriosis found to be increased in association with the number of rising cases of C. jejuni-related GBS [16]. The study estimating the diseases burden of food-borne origin in Netherland during 2020-2060 will be the same as was in year 2011 [17]. While from Poland a study suggested that the incidence rate of Campylobacter infections has been underreported and under- diagnosed as 1.12 cases of infections per 100,000 reported [18].
The reports from China showed 4.84% prevalence of C. jejuni infections and 14.9% patients suffered from gastroenteritis in a hospital of Beijing [19,20]. In Another study the rate of campylobacteriosis is associated with consumption of chicken meat and raw meat that was 1.6% in urban and 0.37% in rural settings respectively [21]. In Japan, because of unexpected outbreaks the campylobacteriosis infections were found to be 100 cases per 100,000 of population each year [22]. The patients suffered in India having gastroenteritis were found to be culture positive for Campylobacter, C. jejuni was found to be in 70% cases while another study revealed 16.2% cases accounted various Campylobacter species [23,24]. In another study from South India the rate of infections caused by Campylobacter in Children age less than 5 years were found to be 4.5% [25]. Furthermore, a case-control study including, Kolkata (India), Mirzapur (Bangladesh) and Karachi (Pakistan) highlighted the C. jejuni association with the diarrhoea among children 0-59 months off age [26].
The transmission of Campylobacter is less well understood. It is hypothesized that most poultry and many household pets are Campylobacter carriers in Pakistan; a report shows (7%) Campylobacter isolates were detected in children under five years, and the most frequently isolated Campylobacter species was C. jejuni [27,28]. In a 11 year period study from 1992-2002, isolation rate is 24.8% of C. jejuni and Isolation rate of Campylobacter was higher (45.7%) among children under 2 years of age as compared to other age groups [29]. In 3 year period study, from January 2002–December 2004, three big cities of Pakistan (Faisalabad, Lahore and Islamabad), results shows among meat samples, the highest prevalence (48%) of Campylobacter was recorded in raw chicken meat followed by raw beef (10.9%) and raw mutton (5.1%) [30]. A recent cross-sectional study, shows a high prevalence of Campylobacter in chicken meat (29%) followed by mutton (18%) and beef (15.5%) [31].
Campylobacter needs the use of culture-dependent and culture independent techniques for growth, Campy or skirrow agar medium is used that is supplemented with antibiotics to inhibit the growth of other enteric flora. Campylobacter grows at 42°C, needs H2-enriched atmosphere [32]. There is no Gold stranded method used to cultivate Campylobacter, different selective media are used such as, blood-based agar or blood-free agar, have been used for the isolation of Campylobacter species [33]. A more efficient method is the “Cape Town protocol” that needs filtration of clinical samples through pores of membrane filters, of size having 0.45 or 0.65 micro meter, then poured onto blood agar (with or without vancomycin supplementation). Then incubation of plates are set to 37°C under the microaerophilic conditions i.e. (5%O2) enriched with CO2 and H2 [34]. Optimum value of H2 enhances growth of bacteria; the Cape Town protocol is being successful in isolating different species of Campylobacter from faecal, intestinal biopsy, and saliva samples [34]. The most frequently used alternatives to conventional cultivation are cultivation independent techniques i.e. DNA-based or molecular assays, for example, polymerase chain reaction (PCR) or real-time PCR assays [35]. Furthermore, Successful attempts also have been made with recombinant Campylobacter proteins as antigens in ELISA assays [36], these assays are validated and supported [37]. Oxidase activity is present in all species except for C. gracilis [38]. Under unfavourable growth conditions, these microorganisms have the ability to form viable but non-cultivable cells (VBNC), there are still questions to answer about whether or not the non-cultivability is equal to non- viability or whether it is possible to convert VBNC form to a cultivable form, and does the VBNC form of Campylobacter actually exists? [39-41].
A large and diverse number of risk factors contribute to the susceptibility of humans to campylobacteriosis. A current meta- analysis report shows that traveling is the most important risk factor for campylobacteriosis, followed by consumption of undercooked chicken, environmental exposure, and direct contact with farm animals [42]. Some of the important risk factors in transmission of campylobacteriosis have been discussed below and others are depicted in Figure 1.
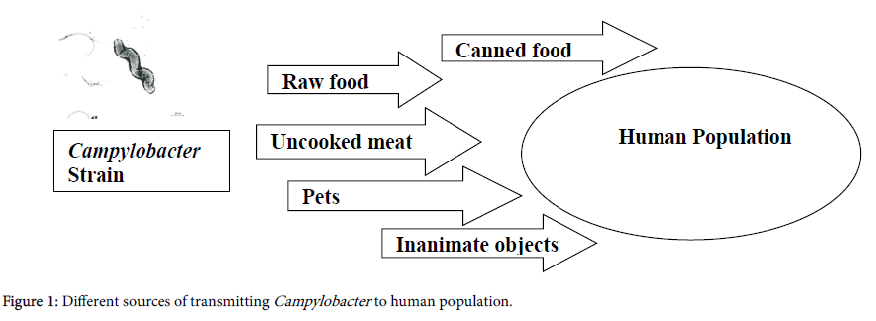
Figure 1. Different sources of transmitting Campylobacter to human population.
Environmental exposure
The incidence of campylobacteriosis is associated with the seasonal increase with flies according to a report from England, the seasonal increase in fly population in the warm summer months because of high temperature and also of rainy weather that makes favourable conditions in the development of flies. This results in contact of flies with human and animal faeces, supporting the idea of environmental conditions, responsible for observed seasonal outbreaks prevalent during the warm summer months [43]. Organic and conventional environment conditions also have been found to be associated with campylobacteriosis [44]. In other report from Denmark, as ambient temperature increases there is a parallel increase in the incidence of human campylobacteriosis, the largest increase in incidence is between 13°C and 20°C [45].
Poultry
Poultry is one of the major food-related sources in transmission of campylobacteriosis, to humans, especially the broiler chicken [46]. Moreover, poultry sector also act as an important reservoir of other Campylobacter species, such as C. lari, C. upsaliensis, and C. concisus [6,47]. Both, domestic and imported broilers chicken increases the incidence of campylobacteriosis and other campylobacter infections worldwide [48]. In addition, campylobacter are shed in faeces and found ubiquitously in the environment, including surface water, potential transmission to broiler houses via vectors such as flies, insects, rodents or via vehicles as aerosols or dust can be occurred [49].
Wildlife Campylobacter species (primarily C. jejuni and C. coli) are essentially commensals in birds and frequently colonize the intestine in high numbers [50]. Wild animals are also the potential reservoir but the wild birds are found to be potential transmission vector. Campylobacter jejuni has been isolated from wild birds such as pigeons, crows, geese, ducks, gulls and cranes [51,52]. It is noteworthy that migratory birds can travel long distances and could be a potential source of new campylobacter species genotypes within different animals as such as cattle, sheep and broiler [53-55]. Furthermore, Town parks and recreation places are the regular environment for wild birds, especially pigeons and crows. Thus, children are more prone to acquire the campylobacter infections and also to people those having negligible or poor hygiene practices [56].
Domestic animals Beside the broad spectrum of food products obtained from the group of animals, like poultry, the most common source of infection are also includes pets (particularly cats and dogs), and livestock plays an important role as infection vectors [57]. Ruminants, such as cattle, sheep, and goats, also act as a reservoir for campylobacter bacteria [57,58]. Campylobacter species are present mostly in the gut (duodenum, jejunum, small and large intestines), rather than in rumen [59]. Hence, meat consumption from domesticated animals or contact with domesticated and companion animals impart a significant risk for the transmission and spread of Campylobacter species [60-62].
Water
In some reports from previous studies, drinking water is considered to be a major threat of transmitting the disease campylobacteriosis [63,64]. Campylobacter can colonize in water pipes of broiler houses, make biofilms, this character further enhances the survival and growth of Campylobacter species and pose a major threat of colonization in chicken flocks [65]. According to a recent study in Ireland, there is a significant problem facing in removing Campylobacter species colonies in water pipes after disinfection in 7 out of 20 farms [66].
People consuming water from private wells rather than municipal surface water systems as a drinking water source are more prone to campylobacteriosis than other reportable enteric diseases [67]. The contamination of outdoor water due to wild bird’s faeces and wastes shedding from contaminated domesticated animals are also the contributing factors in Campylobacter transmission [68].
Other sources Person-to-person transmission (faecal-oral or via fomites), are not so common mean of transmission but has a significant potential and have a tendency to transmit. In United kingdom, a report from Health Protection Agency found to have 3% person-person transmission in campylobacteriosis cases [69]. Unpasteurized milk consumption from dairy cattle’s also have provoked many outbreaks of campylobacteriosis [70-72]. Unpasteurized milk is also the source of several other Campylobacter species, including C. hyointestinalis subsp. hyointestinalis, C. foetus subsp. foetus, C. conscious, and C. ureolyticus, the genomic analysis reveals the significant contamination of milk with faecal matter [73-75]. Insects such as flies, travelling and poultry products are also the typically potential and hazard full aspects of Campylobacter infections transmission [76,77].
Zoonotic impacts
The incidence rate of infections caused by Campylobacter species has been constantly increasing. Currently; it is the most common food borne bacterial zoonosis in the world [78,79]. It is estimated that Campylobacter species cause 500 million infections each year worldwide [79]. Since 2005, in European Union the number of cases campylobacteriosis has been the highest of all zoonosis, after 2010, the campylobacteriosis patients has been over 200 thousand each year. According to a report from EFSA In 2012, cases were 214,268 and then in 2015 increases up to to 229, 213 and in 2016, further increased to 246,307 [80-83]. In the United States, campylobacteriosis affects a million people a year, in Canada, there are more than 200 thousand cases registered each year and the cases of campylobacteriosis also become common in Africa, Asia, and the Middle East, particularly in children [84-86].There are several distinct potential factors that pose specific influence in the pathogenesis of disease like motility and chemotaxis, adhesion, invasion, and toxin production [87]. Furthermore there are several genes flaA (flagellin gene), cadF (adhesion gene), racR, and dnaJ were selected as pathogenic genes responsible for adherence and colonization; virB11, ciaB, and pldA as pathogenic genes responsible for invasion; cdtA, cdtB, and cdtC as pathogenic genes responsible for the expression of cytotoxin production (Table 1) [88,89].
| Sl. No. | Virulence factors | Responsible genes & proteins |
|---|---|---|
| 1 | Chemo-taxis | flaA and flab |
| 2 | Adhesion | CadF, CapA, PEB1, JlpA |
| 3 | Invasion | Cia, CiaB, CiaC, CiaD, CiaI |
| 4 | Toxins Production | CDT (cdtA, cdtB, cdtC) |
Table 1: Virulence factors of Campylobacter aiding in Pathogenesis.
Motility Flagella is the main and essential component in the movement in response of the chemosensory system, because of the corkscrew shape and the presence of flagella, Campylobacter are capable for swimming through the mucus layer that covers the epithelial lining of the intestine, helping the pathogen to reach its favoured colonization site, the inner mucus layer of the intestine. The principal flagellum filament proteins are the major and minor, that includes flagellin subunits FlaA, and the minor subunit FlaB, encoded by the genes i.e. flaA and flaB [90].
Adhesion Adhesins are located on the bacterial surface and are major components in triggering the disease by binding to epithelial cells [91]. CadF, is a 37-kDa fibronectin-binding outer membrane protein, lack of CadF in mutant strains shows avoiding of colonization by Campylobacter [92]. In addition, other identified proteins that includes in colonization are CapA, the periplasmic-binding protein PEB1, and the surface-exposed lipoprotein JlpA [91].
Invasion A set of proteins called Campylobacter invasion antigens (Cia), plays an important role in consistent campylobacteriosis [93]. There are three Cia proteins: CiaB related with adherence to the target cells, CiaC required for full invasion of INT-407 cells, and CiaI which has been reported to play an essential role in surviving intracellularly, another recently discovered fourth protein is CiaD, has been found to be an important factor required for maximal invasion of the host cells [94].
Toxin production
Campylobacter, like other gram negatives, produces cytolethal distending Toxin (CDT), encoded by the cdtABC operon. While cdtA and cdtC are involved with binding and internalization into the host cell, cdtB encodes the enzymatically active/toxic subunit [70]. CDT contributes to pathogenesis by inhibiting both cellular and humoral immunity, via apoptosis of immune response cells [95].Campylobacteriosis is the major disease caused by two species i.e. C. jejuni and C. coli. Furthermore, C. jejuni is found on the basolateral surface of endothelial cells and undergoes exocytosis. C. jejuni causes extraintestinal infections and therefore leads to long-term complications, including septicemia, meningitis, pancreatitis, abortion of pregnant women, reactive arthritis, Guillain-Barré syndrome, Miller Fisher syndrome [96,97].
According to a recent diagnostic and therapeutic approach to Campylobacter, ICT (In-circuit test), have good diagnostic importance and should be recommended as a first-line test for patients with diarrhoea syndrome. Another approach is the use of Eva Green real- time PCR method for the simultaneous detection and identification of C. jejuni and C. coli directly from faeces, this test with high sensitivity and specificity, which is applicable mostly in molecular epidemiology and difficult diagnostics [98].
Campylobacter infections are normally self-resolving but may become severe in patients having bacterimia, therefore needs antimicrobial therapy. Erythromycin is considered as the key drug for treatment of campylobacteriosis, because it is easy to administer and has a narrow spectrum of activity [99]. In past, fluoroquinolones were the drug of choice for patients to treat campylobacteriosis, without waiting for results of stool culture, as Campylobacter. Also, macrolides other than primarily erythromycin or alternatively clarithromycin or azithromycin are also in use as the drugs of choice [100].
Macrolides, such as azithromycin and fluoroquinolones, such as ciprofloxacin are the effective drug therapy to campylobacteriosis, but the emergence of resistance to these drugs has posed a major threat to “One health” approach, causing over about 300,000 infections per year [101]. Researchers confirm that Campylobacter species have an antibiotic resistance rate over the past 20 years, particularly quinolones, fluoroquinolones and macrolides over the world [102].
There are several approaches needed to be considered to control campylobacteriosis, especially bio-security measures and personal hygiene practices, to avoid poultry contamination and transmission between batches. The use of various substances is also recommended to control Campylobacter such as essential oils, prebiotics, probiotics, bacteriocins, bacteriophages and immunization measures.
It is now estimated as common matter of fact that the infections caused by Campylobacter are increasing due to its easy transmission routes and sources. The neglecting precautionary measures in handling and supplying food to geographical locations worldwide have also taken part in prevailing infections. Furthermore, improper unpasteurized canned food and its huge consumption in today’s industrial era also act as a predisposing element in propagating the infections. So, we suggest addressing people by developing and organizing awareness campaigns, acknowledgment and briefing by medical experts, doctors etc. hoped to be a better way to tackle it. In addition proper cooking, controlling food quality during handling, preparation and freezing have also a major role in spreading diseases, so proper measures should be adapted. Moreover, we recommend more investigations and surveillance program globally to identify specific strains especially in areas like tropical regions, so that a proper comprehensive picture should be established in understanding Campylobacter infections.
The authors declare that there are no conflicts of interest.
Citation: Shad AA and Shad WA (2019) Review of Food-borne Micro-organism: Campylobacter Species. J Food Microbiol Saf Hyg 4: 141.
Received: 26-Feb-2019 Accepted: 25-Mar-2019 Published: 01-Apr-2019
Copyright: © 2019 Ahtesham AS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.