Pancreatic Disorders & Therapy
Open Access
ISSN: 2165-7092
ISSN: 2165-7092
Case Report - (2017) Volume 7, Issue 1
Laparoscopic cholecystectomy is gold standard for symptomatic gallstone and is world widely used for decades. With this minimally invasive approach, patients recovered from operation quicker than traditional open method. But biliary complication during this operation was not rare and had been reported. Literatures had suggested many preoperative image studies and intraoperative methods to avoid biliary complications. However, patients with biliary tree variation may have higher risk of bile duct injury during operation. Here, we present the patient with extremely rare biliary variation who encountered bile duct injury during laparoscopic cholecystectomy. The preoperative images, intraoperative findings, managements for complications, outcome and short review of the literature were recorded.
<Keywords: Bile duct variation; Right hepatic duct; Laparoscopic cholecystectomy; Bile duct injury
Laparoscopic cholecystectomy is gold standard for symptomatic gallstone and is world widely used. Biliary complications during operation had been reported. Literatures had suggested many preoperative image studies and intraoperative methods to avoid biliary complications. However, biliary tree variation may increase the risk of bile duct injury during operation. In this article, we presented the patient with right hepatic duct drainage into gallbladder infundibulum and encountered biliary complication during laparoscopic cholecystectomy for symptomatic gallstones.
The complication was diagnosed and treated immediately in the same operation. And the patient recovered well after biliary reconstruction and biliary stent insertion. In conclusions, bile duct injury during cholecystectomy in this kind of variation is inevitable. Careful preoperative image interpretation and explanation, meticulous intraoperative technique, and multidisciplinary approach for biliary complications were important for the era of laparoscopic cholecystectomy.
Case Presentation
A 63 years old female, with gallstone history, presented with nausea and epigastralgia. Because of mild bilateral intrahepatic duct dilataion, the patient underwent further biliary study. Magnetic resonance cholangio pancreatiocography (MRCP) (Figure 1A) and endoscopic retrograde cholangiopancreatography (ERCP) (Figure 1B) before operation did not show biliary anomaly. Laboratory data of liver function and hemogram were within normal range.
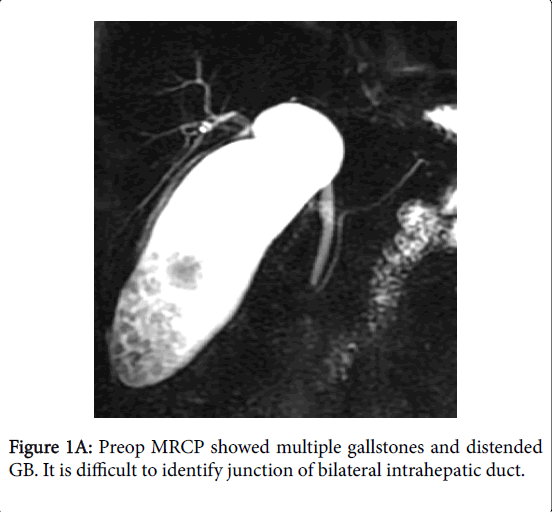
Figure 1A: Preop MRCP showed multiple gallstones and distended GB. It is difficult to identify junction of bilateral intrahepatic duct.
The patient was admitted for elective laparoscopic cholecystectomy. During operation, gallbladder was decompressed for achieving critical view. The cystic duct was divided close to the infundibulum after cystic artery division (Figure 2A). However, right hepatic duct (RHD) was injured during dissection of liver bed (Figure 2B).
The operation was converted to open surgery. Intraoperative cholangiography (IOC) through the stump of RHD (Figure 3A) and the cystic duct (Figure 3B) demonstrated transection of RHD.
The image of biliary variation and the biliary reconstruction with right hepatic duct to cystic duct stump (microsurgery) were sketched (Figure 4).
After operation, the bile leakage was treated with low pressure suction through abdominal drain, empiric antibiotics and plastic biliary stent inserted via ERCP. The patient was discharged smoothly. Three months after operation, the ERCP showed patent biliary anastomosis and the stent was removed. Two years after operation, the patient has normal liver function test and there was no biliary tree dilatation in MRCP study.
Laparoscopic cholecystectomy is gold standard surgery for cholelithiasis for decades. However, the incidence of bile duct injury was around 0-2.6% [1]. The risk factors of bile duct injury during laparoscopic surgery were inexperience, inflammation and aberrant anatomy [2]. Many types of bile duct variation had been reported in literatures. Main RHD drainage into cystic duct was extremely rare. The incidence was around 0.3-9% [3-5]. According to literatures, 11 patients, with right hepatic duct drainage into cystic duct, underwent laparoscopic cholecystectomy. But only 4 cases can be collected in this article and the detail demography was lack (Table 1).
Some patients encountered RHD injury but some did not. Our presented case was one of the right hepatic duct drainage into GB infundibulum. Many literatures had emphasized the importance of preoperative image such as MRCP and ERCP to map biliary tree anatomy. IOC was also suggested for identify bile duct variation and prevent bile duct injury [6].
In our presented case, MRCP and ERCP before operation cannot identify the bile duct variation. IOC before cystic duct division cannot prevent bile duct injury. Bile duct injury in this case is inevitable. The injury of this abnormal RHD was diagnosed based on two evidences. First, the RHD was injury during liver bed dissection which was encountered after cystic duct division and there was some distance between the injury site and the cystic duct. Second, there was absence of RHD when IOC was performed via divided cystic duct. Our patient received immediate biliary reconstruction with microsurgery. Our micro-surgeon was experienced in bile duct reconstruction during living donor liver transplantation. His was used to perform anastomosis with interrupt sutures at posterior wall and continuous suture anterior wall followed by interrupt tie [10]. He rarely uses internal biliary stent during bile duct reconstruction. Patient developed bile leakage with successful treatment by biliary stent after operation. The postoperative outcome is smooth at 2 years after operation.
Bile duct injury during cholecystectomy in this kind of variation is inevitable. Long-term follow-up for this patient is needed. Careful preoperative image interpretation and explanation, meticulous intraoperative techniques, and multidisciplinary approach for biliary complications were important for the era of laparoscopic cholecystectomy.
`We are grateful to the members of the Department of Surgery for the care of this patient.