
Journal of Clinical Trials
Open Access
ISSN: 2167-0870

ISSN: 2167-0870
Research Article - (2023)Volume 13, Issue 2
Purpose: To identify potential risk factors for cage subsidence after oblique Lumbar Interbody Fusion (OLIF) using imaging and clinical date, and provide guidance for surgical planning in clinical practice.
Methods: Data of 107 patients who underwent OLIF were retrospectively analyzed. Patients with cage subsidence distance >3 mm were included in the Cage Subsidence group (CS group), and the remaining patients were involved in the Non Cage Subsidence group (NCS group). The characteristics (age, gender, Body Mass Index (BMI), main diagnosis, comorbidities etc), vertebral body related variables (Disc Height (DH), endplate morphology, and Modic changes) and surgery related variables (internal fixation, cage position, and endplate injury) were collected. Moreover, the Visual Analog Scale (VAS) score, and the Japanese Orthopedic Association (JOA) score were determined preoperatively, postoperatively, and at follow up. Firstly, univariate analysis was used to compare the risk factors related to cage subsidence, and then, the multivariate logistic regression analysis was employed to determine the possible risk factors (p<0.10) for cage subsidence after OLIF.
Results: In total, 21 (19.63%) patients were involved in the CS group. The factors significantly associated with cage subsistence included intraoperative endplate injury (odds ratio (OR)=6.620; p=.020), osteoporosis (OR=6.179; p=. 004), irregular endplate morphology (OR=5.192; p=.012) and without internal fixation (OR=6.672; p=.013).
Conclusion: Cage subsidence did not affect the neurological function, while it led to low back pain in the later stage. The risk factors for cage subsidence included intraoperative endplate injury, osteoporosis, irregular endplate morphology, and treatment with standalone OLIF.
Lumbar degenerative disease; Oblique lateral interbody fusion; Cage subsidence; Risk factors
OLIF: Oblique Lumbar Interbody Fusion; CS group: Cage Subsidence Group; NCS group: Non-Cage Subsidence Group; DH: Disc Height; ΔDH: DH at the last follow up visit minus the postoperative DH
With the aging of the world population, a large number of people suffered from lumbar degenerative disease [1,2]. Clinical symptoms, such as low back pain, claudication, radicular pain, and neurological deficit caused by lumbar degenerative disease remarkably reduce the quality of life. Surgical treatment has shown a higher efficacy compared with multiple conservative methods for the therapy of lumbar degenerative disease [3,4]. There are several main approaches for the treatment of lumbar degenerative disease, including (PLIF), Transforaminal Lumbar Interbody Fusion (TLIF), Anterior Lumbar Interbody Fusion (ALIF), Lateral Lumbar Interbody Fusion (LLIF), and Oblique Lumbar Interbody Fusion (OLIF) [5]. OLIF was first proposed by Mayer 6 in 1997, and Silvestre et al. reported satisfactory results with minimal blood loss, short operation time, and excellent functional rehabilitation achieved in 179 patients who underwent OLIF. However, limited by supporting instruments and cages, it was not widely carried out until the appearance of special fusion cage for OLIF and its supporting channel system. This approach involves a minimally invasive access to the disc space via a corridor between the anterior vessels and psoas muscle to achieve an “indirect” posterior decompression [6,7]. OLIF possesses a variety of advantages, and compared with the posterior approach, the operation time, intraoperative blood loss, and para spinal musculature injury were reduced in patients undergoing OLIF. In addition, Minimally Invasive TLIF (MI-TLIF) is associated with para spinal iatrogenic injury. The abdominal and vascular complications associated with the anterior approach were also avoided in OLIF [8]. Compared with the LLIF, the OLIF did not dissect or traverse the psoas muscle and neuro monitoring was not requested [9].
However, several OLIF associated complications were reported, such as transient femoral nerve paralysis, cage subsidence, vertebral endplate injury, and main vascular injury [10]. Among them, cage subsidence is a common complication that could affect the clinical outcomes. Relevant studies have pointed out that the incidence of cage subsidence after OLIF was 7.3%~46.7%. However, few risk factors for cage subsidence after OLIF were reported. Hence, the present study aimed to identify potential risk factors for cage subsidence after OLIF using imaging and clinical date, and provide guidance for surgical planning in clinical practice.
Study population
In the present study, data of 107 patients with lumbar degenerative disease who underwent OLIF from May 2017 to May 2021 were retrospectively analyzed. This study protocol was approved by our institutional review board, and all patients provided informed consent.
The basic data, such as age, gender, Body Mass Index (BMI), Bone Mineral Density (BMD), diagnosis, comorbidities, operational level, operation time, and intraoperative blood loss were collected.
Inclusion criteria
• Patients with symptomatic lumbar degenerative disease (lumbar spine stenosis, grade I degenerative spondylolisthesis, degenerative scoliosis).
• Patients who had no obvious recovery after regular conservative treatment for at least 3 months.
• Patients with complete radiographic and clinical data.
• Patients who completed at least 12 months of follow up.
Exclusion criteria
• Patients who had previous adjacent segment lumbar surgery.
• Patients with severe osteoporosis (T-score<-3.5).
• Patients with spinal tumors or spinal inflammation.
• Patients with cage subsidence caused by a major accident.
Surgical procedures
The patient was placed in a right lateral decubitus position under general anesthesia. Anteroposterior and lateral C-arm fluoroscopic images were used to ensure that the patient was exactly in the lateral position. A 4 cm skin incision was made with 4 cm~6 cm distance from the disc space and paralleled to the fibers of the external oblique muscle. The skin and subcutaneous tissue were dissected in turn, and the external oblique, internal oblique and transverse abdominal muscles were bluntly dissected to the anterior retroperitoneal space located between the psoas muscle and abdominal aorta. The Kirschner wire was used under fluoroscopy to determine the surgical intervertebral space, and then, the working channel with light source was placed and fixed. The annulus fibrosis, disc, and endplate were excised sequentially. The contralateral annulus fibrosus was also released. An appropriate-sized cage filled with autologous iliac crest bone graft or allogeneic bone was passed into the disc space. The fluoroscopic image confirmed that the cage position was satisfactory. Incision was sutured without placement of drainage strips or drainage tubes. Some patients underwent lateral or posterior internal fixation.
Radiological and clinical evaluation
All patients underwent preoperative anterior and lateral lumbar radiography, Computed Tomography (CT), and Magnetic Resonance Imaging (MRI). Patients in an upright position underwent plain radiography during follow up. The vertebral body related variables (disc height (DH), endplate morphology, and Modic changes) and surgery-related variables (internal fixation, cage position, and endplate injury) were collected.
The DH was defined as the average value of the distance between the upper and lower endplates at the anterior, middle, and posterior sides. The cage subsidence distance was expressed by ΔDH, which was defined as the DH at the last follow-up visit minus the postoperative DH. Patients with cage subsidence distance >3 mm at the last follow-up visit were involved in the Cage Subsidence group (CS group), and the remaining patients were included in the Non Cage Subsidence group (NCS group). The morphology of the endplate was evaluated on sagittal T1- weighted MRI of the lumbar spine and classified as irregular or irregular. The cage position was calculated as follows: the distance from the front edge of the lower endplate to the center of the cage/the distance between the anterior and posterior edges of the lower endplate. According to the cage position value, patients were allocated to anterior (value<0.4), middle (value at the range of 0.4~0.6), and posterior (value>0.6) categories. Endplate injury was defined as endplate invaded on the lateral lumbar radiograph.
Clinical evaluation was conducted by questionnaire preoperatively, postoperatively, and at follow-up. The degree of back pain was evaluated by the Visual Analog Scale (VAS) score (full score, 10). The neurological function was assessed by the Japanese Orthopedic Association (JOA) score (full score, 29), and the recovery rate was calculated according to the preoperative and the last follow-up scores as follows: (JOA score at the last follow-up visit-preoperative JOA score)/(29–preoperative JOA score) × 100%.
Statistical analysis
All data were analyzed using SPSS 25.0 software (IBM, Armonk, NY, USA). Quantitative data (age, BMI, operation time, intraoperative blood loss, DH, VAS score of low back pain and JOA score of lumbar vertebrae before surgery, immediately after surgery, and at the last follow-up visit) were analyzed by the Student's t-test or the Wilcoxon test. Qualitative data (gender, main diagnosis, comorbidities, osteoporosis, combined application of internal fixation, operational level, position of cage, intraoperative endplate injury, endplate morphology, and Modic changes) were analyzed by the χ2 test. Potential risk factors were first examined by the univariate logistic regression analysis and risk factors with p<0.10 were tested by the multivariate logistic regression analysis. Then, predictors for cage subsidence after OLIF were determined by the multivariate logistic regression analysis with adjusted odds ratios (ORs) and 95% Confidence Intervals (CIs). p<0.05 was considered statistically significant.
There were 21 (19.63%) patients with cage subsidence distance >3 (4.41 ± 1.88) mm in the CS group (Figure 1). The remaining patients (1.07 ± 0.76 mm) were involved in the NCS group (Figure 2). There was a significant difference in cage subsidence distance between the two groups (p<0.001).
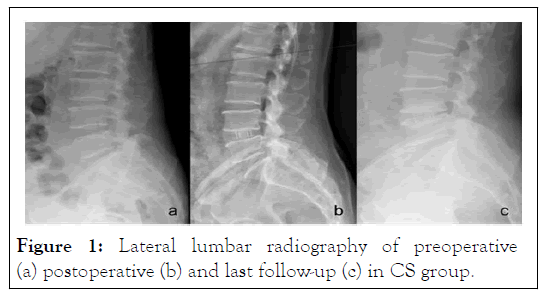
Figure 1: Lateral lumbar radiography of preoperative (a) postoperative (b) and last follow-up (c) in CS group.
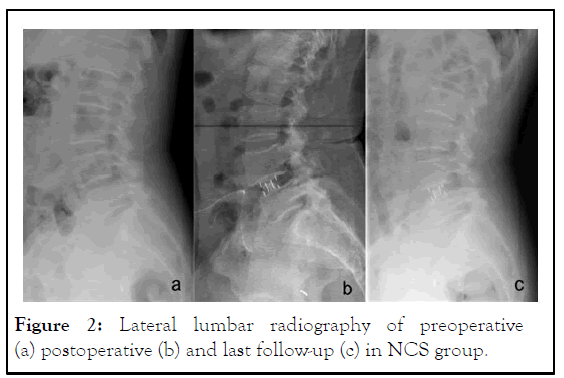
Figure 2: Lateral lumbar radiography of preoperative (a) postoperative (b) and last follow-up (c) in NCS group.
Among 107 patients, there were 19 men and 88 women with an average age of 58.50 ± 7.87 years old. The mean follow-up time was 12.57 ± 1.65 months. The mean BMI was 23.40 ± 2.21 kg/m2. The mean operation time and the mean intraoperative blood loss were 106.68 ± 32.79 min and 135.23 ± 94 ml, respectively. In addition, 70 cases of lumbar spinal stenosis, 31 cases of spondylolisthesis, and 6 cases degenerative scoliosis were diagnosed. Among them, 68 cases were treated with standalone OLIF and 39 cases underwent OLIF combined with internal fixation; 79, 19, 7, and 2 cases underwent L4/5 level, L3/4 level, L2/3 level, and L1/2 level, respectively (Table 1). The mean preoperative DH was 8.79 ± 2.20 mm, which was immediately extended after surgery to 12.45 ± 1.83 mm and this increase was statistically significant (p<0.001). At the last followup visit, the mean intervertebral DH was reduced to 10.77 ± 2.26 mm. The mean cage subsidence distance was 1.72 ± 1.71. The cage subsidence level was L2-L3 in 1 patient, L3-L4 in 4 patients, and L4-L5 in 16 patients.
| Variable | Total patients (n=107) | Subsidence (n=21) | Non-subsidence (n=86) | P-value |
|---|---|---|---|---|
| Age (years) | 58.50 ± 7.87 | 57.98 ± 8.34 | 60.62 ± 5.14 | 0.116 |
| Gender (male/female) | 0.852778 | 03:18 | 0.715278 | 0.884 |
| Body mass index | 23.40 ± 2.21 | 23.39 ± 2.17 | 23.43 ± 2.41 | 0.838 |
| Diagnosis | ||||
| lumbar spine stenosis | 70 | 17 | 53 | |
| Spondylolisthesis | 31 | 4 | 27 | 0.19 |
| Degenerative scoliosis | 6 | 0 | 6 | |
| Follow-up period | 12.57 ± 1.65 | 12.48 ± 1.63 | 12.95 ± 1.75 | 0.148 |
| Medical comorbidities | ||||
| Hypertension | 27 | 6 | 21 | 0.694 |
| Diabetes | 18 | 4 | 14 | 0.761 |
| Cardiac disease | 20 | 7 | 13 | 0.108 |
| Cerebrovascular disease | 13 | 4 | 9 | 0.48 |
| Operation levels | ||||
| L1/2 | 2 | 0 | 2 | |
| L2/3 | 7 | 1 | 6 | 0.883 |
| L3/4 | 19 | 4 | 15 | |
| L4/5 | 79 | 16 | 63 | |
| Operation time | 106.68 ± 32.79 | 110.71 ± 39.19 | 105.70 ± 31.22. | 0.67 |
| Intraoperative blood loss | 135.23 ± 94.14 | 150.48 ± 96.51 | 131.51 ± 93.75 | 0.333 |
Table 1: Comparison of patients' characteristics between CS and NCS groups.
The preoperative DH was 8.67 ± 3.01 mm, and it was 12.77 ± 2.43 mm immediately after surgery. Besides, ΔDH was 4.09 ± 1.96 mm in the CS group, and 8.82 ± 1.97, 12.37 ± 1.66, and 3.55 ± 1.63 mm in the NCS group. The DH increased immediately after surgery in both groups. The difference in DH between the two groups was not statistically significant. Additionally, DH at the last follow-up visit in the CS group was 8.36 ± 2.66, which was lower than that in the NCS group (11.36 ± 1.71), indicating a significant difference between the two groups (p<0.001) (Table 2). There were 12 patients with intraoperative endplate injury, 31 patients with osteoporosis, 53 patients with irregular endplate morphology, and 39 patients who received internal fixation. In the present study, intraoperative endplate injury was found in 7 (33.33%) patients in the CS group and 5 (5.81%) patients in the NCS group and there was a significant difference between the two groups (p=0.001). In the CS group, 12 (57.14%) patients were complicated with osteoporosis, in which the incidence of osteoporosis was higher in the CS group than that in the NCS group (22.09%), and the difference between the two groups was statistically significant (p=0.002). Moreover, 16 and 37 patients had irregular endplate morphology in the CS and NCS groups, and its incidence was 76.19% and 43.02%, respectively, indicating the existence of a significant difference between the two groups (p=0.006). The proportion of patients who received internal fixation in the CS group (14.29%) was lower than that in the NCS group (41.86%), and there was a significant difference between the two groups (p=0.019).
| Variable | Total patients (n=107) | Subsidence (n=21) | Non-subsidence (n=86) | P-value |
|---|---|---|---|---|
| Disc height (mm) | ||||
| Preoperative | 8.79 ± 2.20 | 8.67 ± 3.01 | 8.82 ± 1.97 | 0.785 |
| Postoperative | 12.45 ± 1.83 | 12.77 ± 2.43 | 12.37 ± 1.66 | 0.5 |
| Latest follow-up | 10.77 ± 2.26 | 8.36 ± 2.66 | 11.36 ± 1.71 | <0.001 |
| ΔDH(Cage subsidence) | 1.72 ± 1.71 | 4.41 ± 1.88 | 1.07 ± 0.76 | >0.001 |
| Endplate injury | 12 | 7 | 5 | 0.001 |
| Osteoporosis | 31 | 12 | 19 | 0.002 |
| Endplate morphology | ||||
| Regular | 54 | 5 | 49 | 0.006 |
| Irregular | 53 | 16 | 37 | |
| Internal fixation | 39 | 3 | 36 | 0.019 |
| Cage position | ||||
| Anterior | 40 | 8 | 32 | 0.939 |
| Middle | 44 | 8 | 36 | |
| Posterior | 23 | 5 | 18 | 0.389 |
| MODIC | 8 | 3 | 5 | |
Table 2: Comparison of cage subsidence between CS and NCS groups.
There was no significant difference in age (p=0.116), gender (p=0.884), BMI (p=0.838), main diagnosis (p=0.190), and comorbidities (hypertension (p=0.694), diabetes (p=0.761), cardiac disease (p=0.108), and cerebrovascular disease (p=0.480)) between the two groups. There was no significant difference in operational level (p=0.883), operation time (p=0.670), and intraoperative blood loss (p=0.333) between the two groups. Modic changes occurred in 8 (7.48%) patients. In the CS group, there were 3 (14.29%) cases, whereas there were 5 (5.81%) cases in the NCS group. The incidence of Modic changes in the CS group was higher than that in the NCS group, however, the difference between the groups was not statistically significant (p=0.389). In the CS group, there were 8 cases in the anterior position, 8 cases in the middle position, 5 cases in the posterior position, and there were correspondingly 32, 36, and 18 cases in the NCS group, respectively. There was no significant difference in the position of cage between the two groups (p=0.939). The preoperative JOA score and VAS score were 17.43 ± 2.75 and 3.76 ± 0.94 in the CS group, and 17.56 ± 2.59 and 3.38 ± 0.97 in the NCS group, respectively. After surgery, these scores were 21.57 ± 2.99 and 1.52 ± 0.87 in the CS group, and 22.17 ± 3.23 and 1.16 ± 0.91 in the NCS group, respectively. There were no significant differences in the JOA score and the VAS score between the two groups before and after surgery. However, there was no significant difference in lumbar JOA score at the last follow-up visit between the two groups (p=0.324). The VAS score in the CS group (2.33 ± 0.97) was higher than that in the NCS group (1.37 ± 0.90), and the difference between the two groups was statistically significant (p<0.001) (Table 3).
| Variable | Total patients (n=107) | Subsidence (n=21) | Non-subsidence (n=86) | P-value |
|---|---|---|---|---|
| VAS | ||||
| Preoperative | 3.46 ± 0.97 | 3.76 ± 0.94 | 3.38 ± 0.97 | 0.102 |
| Postoperative | 1.23 ± 0.91 | 1.52 ± 0.87 | 1.16 ± 0.91 | 0.108 |
| Last follow-up | 1.56 ± 0.98 | 2.33 ± 0.97 | 1.37 ± 0.90 | <0.001 |
| JOA | ||||
| Preoperative | 17.53 ± 2.61 | 17.43 ± 2.75 | 17.56 ± 2.59 | 0.822 |
| Postoperative | 22.06 ± 3.18 | 21.57 ± 2.99 | 22.17 ± 3.23 | 0.486 |
| Last follow-up | 24.16 ± 2.69 | 23.67 ± 2.33 | 24.28 ± 2.76 | 0.324 |
| JOA recovery rate (%) | 54.86 ± 29.18 | 50.84 ± 26.12 | 55.84 ± 29.94 | 0.304 |
Table 3: Comparison of clinical outcomes between CS and NCS groups.
Univariate analysis showed endplate injury (p=0.001), osteoporosis (p=0.002), irregular endplate morphology (p=0.009) and without undergoing internal fixation (p=0.027) were selected into multivariate logistic model of predictors. In multivariate logistic regression (Table 4), endplate injury (OR=6.620, 95% CI=1.354-32.368, p=0.020), osteoporosis (OR=6.179, 95% CI=1.773-21.536, p=0.004), irregular endplate morphology (OR=5.192, 95% CI=1.446-8.641, p=0.012) and without undergoing internal fixation (OR=6.672, 95% CI=1.493-29.815, p=0.013) were identified to be potential risk factors for cage subsidence following oblique lumbar interbody fusion.
| Variable | Adjusted odds radio | 95% Confidence interval | P-value |
|---|---|---|---|
| Endplate injury | 6.62 | 1.354-32.368 | 0.02 |
| Osteoporosis | 6.179 | 1.773-21.536 | 0.004 |
| Endplate Morphology | 5.192 | 1.446-18.641 | 0.012 |
| Internal fixation | 6.672 | 1.493-29.815 | 0.013 |
Table 4: Predictors for cage subsidence following oblique lumbar interbody fusion
Mayer first presented the OLIF approach in 1977, which involves a minimally invasive access to the disc space via a corridor between the anterior vessels and psoas muscle, leading to achieve an “indirect” posterior decompression. OLIF does not require laminectomy, facet resection or peeling of spinal or para spinal muscles. It is appropriate for degenerative lumbar disease, spinal tuberculosis, tumor, kyphosis, postoperative revision, traumatic fracture, etc. OLIF possesses the advantages of less surgical trauma, less intraoperative bleeding, and fast recovery, and the retroperitoneal approach can avoid damage to abdominal organs. However, OLIF had resulted in several complications, such as vascular injury, ureter injury, abdominal organ injury, low back pain, and cage subsidence. Relevant studies have pointed out that the incidence of cage subsidence after OLIF was 7.3%~46.7%. The influence of cage subsidence on clinical curative effect is still controversial, and some scholars demonstrated that the mild cage subsidence was the normal change in the fusion process of upper and lower vertebral bodies in the surgical segment, and have no significant effect on the postoperative therapeutic effect. With further deepening of clinical research, a great number of scholars pointed out that severe cage subsidence had led to narrowing of intervertebral space, nerve compression, recurrent low back pain, lower limb pain, numbness and motor sensory disturbance, which seriously influence the therapeutic effects and mainly require a secondary surgery.
Factors leading to cage subsidence have not been fully clarified. In order to improve the outcomes following OLIF and reduce the incidence of cage subsidence, we included as many factors as possible that could increase the risk of cage subsidence, and analyzed the correlation between cage subsidence and clinical outcomes. In our study, the risk factors of fusion cage subsidence were intraoperative endplate injury, osteoporosis, irregular endplate morphology, and uncombined application of internal fixation.
The results of the present showed that the incidence of cage subsidence was higher in patients with intraoperative endplate injury, which is basically consistent with Park, et al.'s findings. The significance of the endplate has been previously confirmed in several studies. Removal of the endplate can significantly decrease the structural properties of the lumbar vertebral bodies. Kim, et al. showed that endplate injury is a representative of cortical bone injury and it could be affected by cortical bone strength. The injured endplate reduces the ability to balance the cancellous bone pressure under the endplate, increasing the risk of cage subsidence. Osteoporosis was found as a risk factor for increasing the incidence of cage subsidence in the present study. Hou, et al. conducted biomechanical tests on the human lumbar spine, and their results showed that the decrease in BMD was positively correlated with endplate destruction. Multiple studies have reported that the Hounsfield Unit (HU) measurement is predictive for osteoporosis. Ran, et al. demonstrated that patients with lower preoperative HU values were more likely to the risk of cage subsidence, and preoperative HU measurement is recommended to predict interbody cage subsidence. Antiosteoporosis therapy has been advised to effectively reduce the cage subsidence after lumbar interbody fusion. Therefore, BMD or HU should be routinely measured before OLIF, and active anti-osteoporosis treatment should be carried out to reduce the occurrence of postoperative cage subsidence.
In the present study, the results of the multivariate logistic regression analysis revealed that preoperative endplate morphology in the surgical level was associated with postoperative cage subsidence. The DH in patients with irregular endplate was lower, and the hardness was higher than that of regular endplate. Patients with irregular endplate tolerated higher pressure and uneven stress, increasing the risk of cage subsidence. In the current study, the preoperative DH was 8.67 ± 3.01 in the CS group, which was lower than that in the NCS group (8.82 ± 1.97), whereas there was no statistical significance between the two groups. Zhou, et al. reported that after the implantation of the cage, the stress concentration of the harder endplate in the contact area increases, and the stress further propagates into the vertebral body, entering an area where such high stress is not normally experienced. These findings can explain the correlation between irregular endplate and cage subsidence. In addition, the results of the present study showed that OLIF combined with lateral or posterior internal fixation could effectively reduce the incidence of cage subsidence. Alvi, et al. found that the incidence of cage movement was greater in patients undergoing standalone OLIF compared with those receiving posterior internal fixation. Combined with internal fixation, the local stress of the cage was shared and the load of the cage was reduce. Therefore, for cases that are at a high risk of cage subsidence, we strongly recommend the supplementary application of posterior or lateral internal fixation to prevent the cage subsidence.
In contrast to some published studies, age, Modic changes, and cage position were not correlated with the cage subsidence in the present study. Kotheeranurak, et al. reported that patients who aged 60 years and older were at a significantly higher risk of cage subsidence. Campbel, et al. demonstrated that the risk of cage subsidence increased with each additional year of age. It could be related to the fact that older patients are more likely to be complicated with severe osteoporosis, which was not included in the present study. In the current study, only a small number of cases had Modic changes, and there were only 3 and 5 cases in the CS and NCS groups, respectively, therefore, it was impossible to confirm the relationship between Modic changes and cage subsidence. A previous study indicated that Modic changes did not affect the fusion rate after interbody fusion, while the risk of cage subsidence could increase when there was type I or II Modic changes. The correlation between the cage position and the cage subsidence remains controversial. Alimi, et al. reported that cage position did not determine the cage subsidence. However, Kim, et al. showed that anterior cageposition could be a risk factor of cage subsidence. In the presentstudy, the cage position was divided into three groups: Anterior, middle and posterior, and the results showed that there was no significant correlation between these cage position-dependentgroups and the cage subsidence.
The current study indicated that there was no significant difference in immediate clinical efficacy between the two groups. Cage subsidence did not affect the neurological function, while the VAS score in the CS group was significantly higher than that in the NCS group at the last follow-up visit. To some extent, this showed that the cage subsidence reduced the therapeutic efficacy.
This study had several limitations. First, the retrospective, singlecenter design of the study might cause bias. Second, the sample size was relatively small and the follow-up time was also relatively short. Last but not least, this study only included patients who underwent single-segment OLIF, rather than patients who received multi-segment OLIF.
The incidence of cage subsidence after OLIF was 19.63%. The results showed that cage subsidence did not affect the neurological function, while it led to the low back pain in the later stage. The risk factors for cage subsidence included intraoperative endplate injury, osteoporosis, irregular endplate morphology, and treatment with standalone OLIF. Active antiosteoporosis treatment should be performed to reduce the occurrence of postoperative cage subsidence. We also recommend the supplementary application of posterior or lateral internal fixation to prevent the cage subsidence.
This study protocol was approved by our institutional review board.
Not applicable.
The datasets generated and analyzed during the current study are not publicly available because they are licensed for use in the current study, but are available from the corresponding author on reasonable request.
The author(s) declare that they have no competing interests with respect to the research, authorship, and/or publication of this article.
Not applicable.
ZZ and XG contributed equally to this study. All the authors read and approved the final manuscript.
We sincerely thank all the patients and individuals for their participation and the entire researcher for contribution to this article.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Ding W (2023) Risk Factors for Cage Subsidence Following Oblique Lumbar Interbody Fusion for Patients with Lumbar Degenerative Disease: A Retrospective Cohort Study. J Clin Trials. 13:523.
Received: 10-Oct-2022, Manuscript No. JCTR-22-19513; Editor assigned: 13-Oct-2022, Pre QC No. JCTR-22-19513 (PQ); Reviewed: 28-Oct-2022, QC No. JCTR-22-19513; Revised: 31-Jan-2023, Manuscript No. JCTR-22-19513 (R); Published: 08-Feb-2023 , DOI: 10.35248/2167-0870.23.13.523
Copyright: © 2023 Ding W. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.