
Journal of Clinical Toxicology
Open Access
ISSN: 2161-0495

ISSN: 2161-0495
Case Report - (2023)Volume 13, Issue 1
Injectables such as Hyaluronic Acid (HA) and Botulinum Toxin (BoNT) may mediate great clinical improvement in the Quality of Life (QOL) of patients with facial asymmetry due to Facial Nerve Palsy (FNP). This condition is frequent in cancer patients and strongly affects social interactions. We described a case of melanoma 54-year-old female patient with paresis of the left side of the face caused by facial nerve damage during melanoma metastasis removal surgery in the parotid region. She received injections while she was being treated with anti BRAF adjuvant therapy. The patient showed no toxicity and/or adverse reactions to the injectables and drastically improved her quality of life. Maintaining patients’ QOL is of paramount importance and this can be accomplished through a multidisciplinary treatment approach.
Filler; Botox; Asymmetry; Facial; Melanoma; Botulinum toxin
The survival rate of cancer patients has significantly increased due to early diagnosis and the efficacy of available treatments. However, there is a new concept emerging which explores cancer as an increasingly chronic illness that needs to be cured [1]. Patients with cancer or a history of cancer such as melanoma, often experience discomfort with their own image due to disfiguring surgeries, scarring, or facial asymmetry [2,3]. In western countries, aesthetic treatments are increasingly in demand. These include treatments such as fillers, Botulinum Toxin (BoNT), or laser therapy [4]. The uses of dermal fillers and/or BoNT are considered minimally invasive procedures. Both procedures are useful adjuncts in the rehabilitation of patients, especially in Facial Nerve Palsy (FNP). They can be used alone or in combination, tailored to the individual needs of the patient [5]. Facial asymmetry encompasses a broad clinical spectrum. This article will focus on patients presenting with asymmetry and muscle dysfunction secondary to secondary surgery of left FNP from excision of melanoma metastases of the parotid region.
A melanoma 54-year-old female patient appeared at our dermatologic department with paresis of the left side of the face caused by FNP during melanoma metastasis removal surgery in the parotid region. The patient had undergone adjuvant therapy with anti-BRAF. She showed asymmetry at rest and dyskinesia while smiling, sulking, and kissing. Facial analysis was made by Vectra digital assessment (Figure 1). Difficulty speaking, eating, drinking, and social embarrassment was reported by the patient. The patient received injections of BoNT (onabotulinumtoxinA, Vistabex®, Allergan Aesthetics): 4 units in procerus, 4 units in right corrugator, 6 units in frontalis (right side, F), 12 units in orbicularis (OO), 2 units in the Depressor Septi Nasi (DSN), 2 units in right Levator Labii Superioris Alaeque Nas (LLSAN) and 2 units in right Levator Anguli Oris (LAO) muscles (Figure 2). After 15 days, we proposed the use of miomodulation (Myomo) with Hyaluronic Acid (HA) to impair muscular movement and face harmony. The technique used for MyoMo was the injection of HA as a multilayer approach, where a supraperiosteal and a subcutaneous injection of HA were performed (Figure 3). First, according to MD Codes and Dyna Codes a vycross® technology HA filler (Voluma® with Lidocaine; Allergan Aesthetics,) was selected for the supraperiostial injection in T1 (0, 3 ml for right side and 0, 7 ml for left sides), CK1 (0, 3 ml for right and 0, 3 ml for left sides), CK2 (0, 2 ml for right side and 0, 2 ml for left side) in order to modulate temporal and zygomaticus major and minor muscles respectively (Figure 3). To improve the movement and structure of the lower third of the face was selected a vycross® technology HA filler (Volux® with Lidocaine; Allergan Aesthetics,) for subcutaneous injection in C1 (0, 7 ml right side) and in C2 (0, 3 ml right side) to modulate depressor anguli oculii, depressor labii inferioris and mentalis muscles activity. The patient showed no severe adverse events and no interactions with therapy.
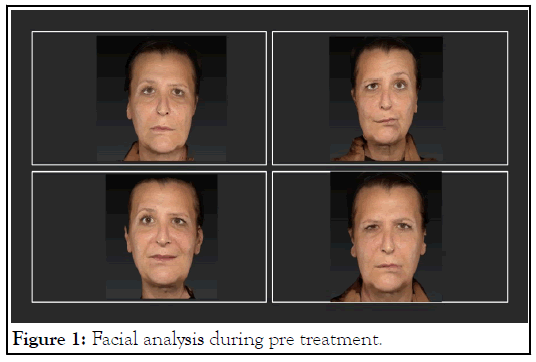
Figure 1: Facial analysis during pre treatment.
Figure 2: After botulinum toxin treatment.
Figure 3: After hyaluronic acid treatment.
Cancer patients are experiencing an increase in overall survival because of earlier diagnoses and newer effective anticancer therapies. However, cancer survivors often face longtermconsequences from their original cancer diagnosis and longterm sequelae of anticancer treatment [6].
One of the key objectives in patients’ cancer care is improving their Quality of Life (QOL) and it is necessary to treat the patient in all aspects of the illness [2]. Loss of facial symmetry, synkinesis, and unpleasant appearance drastically reduce the (QOL). BoNT and HA have been used to improve facial symmetry and movement. Ipsilateral facial strength is frequently increased after contralateral botulinum toxin injection due to the strength redistribution phenomenon. This may be credited to either reduced dominance of the hyperdynamic side or to central cortical reorganization after BoNT [5,7]. Accurately placed BoTN decreases compensatory contralateral hyperkinesis and facilitates the symmetrical function of the cheek and periocular and perioral regions. Injectable fillers are unique in that they can simultaneously support weak muscles, locally block overactive muscles, and enhance toxin efficacy through a finetuned balance between antagonist and synergist groups [8]. In the authors’ practice, FNP is initially treated with conservative doses of BoNT. The patient has been reviewed at 2 weeks for possible touch-up treatment, allowing the opportunity for adjustment to altered muscle balance. During the initial visit, the patient was encouraged to chew on the weakened side and instructed to do basic facial retraining exercises. Further treatment with HA fillers, according to the principles of myomod, is established 15 days after BoNT. Specific contraindications for the use of BoNT in FNP include active infections, keratitis, symptomatic dry eye syndrome, myopathic or severe involutional ptosis, and myasthenia gravis. In the treatment of cancer patients, it is necessary paying particular attention to the presence of immunosuppression and the persistence of skin complications to avoid infections. In the author’s practice, fillers are performed in patients with stable FNP at least 1 month after starting therapy and 3 months after surgery. When treating patients with either BoNT or HA fillers, it is imperative that injectors have a deep understanding of agonist and antagonist muscle groups, as levators and depressors work in opposition for normal and balanced facial expression. Among melanoma therapies, immunotherapy drugs are considered as risk factors for developing foreign body reactions. BRAF inhibitors seem safer because to our knowledge, only one case of a granulomatous/sarcoid-like reaction has been described in patients receiving this therapy [9-11]. BoNT injections could be useful for treating conditions caused by cancer and the consequences of surgery, such as asymmetries, spasticity, and dyskinesias. When BoNT is combined with HA fillers, baseline function could be improved, but future randomized clinical trials are indicated in this regard. However, it must be kept in mind that some filler can appear with a similar appearance to malignant formations and can create interpretation problems when performing instrumental examinations (computed tomography, fluorodeoxyglucose-positron emission tomography, and magnetic resonance) [12]. Changes in physical appearance induced by cancer and its treatments are some of the greatest sources of stress for patients; therefore, it is essential to evaluate the safety of aesthetic treatments offered to them. Particularly in the use of fillers, it is essential to consider the possible interference of materials used with instrumental diagnostic techniques. Therefore, it will be important for the patient to report every possible consequence of the aesthetic procedure to their oncologist.
The treatment goals of BoNT and HA in FNP include an improvement of aesthetic patients’ appearance new dynamic balance between the paralyzed and non-paralyzed sides. Because impairment of cancer patients skin barrier and immune system, it will be essential to ensure maximum aseptic conditions. Physicians should monitor these patients more in order to avoid adverse events after procedures. Aestethic treatments are crucial in the management of this type of patients and should be involved in the multidisciplinary care of a cancer patient cohort with great potential for improving QOL. Injectables’ choices must take into account the interactions with anticancer therapy.
Our patient was fully informed about the publication.
The authors declare no conflicts of interest.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Proietti I, Potenza C (2023) Role of Hyaluronic Acid and Botulinum Toxin Infiltration in Correcting Facial Asymmetries after Melanoma Metastasectomy. J Clin Toxicol. 13:523.
Received: 01-Dec-2022, Manuscript No. JCT-22-19948; Editor assigned: 05-Dec-2022, Pre QC No. JCT-22-19948 (PQ); Reviewed: 19-Dec-2022, QC No. JCT-22-19948; Revised: 26-Dec-2022, Manuscript No. JCT-22-19948 (R); Published: 02-Jan-2023 , DOI: 10.35248/2161-0495.23.13.523
Copyright: © 2023 Proietti I, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.