Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Research Article - (2024)Volume 15, Issue 3
Background: To compare the visual and refractive outcomes, vault and rotational stability between horizontal and vertical toric Implantable Collamer Lens (ICL) placement.
Materials and methods: This retrospective case-control study comprised 36 eyes of 36 patients with vertical toric ICL placement and 36 eyes of 36 patients with horizontal placement. The two groups were matched strictly 1:1 from January 2020 to October 2020. The visual acuity, vault, manifest refraction, Efficacy Index (EI), Safety Index (SI), vector analysis and rotational stability were compared between the two groups.
Results: Residual astigmatism in the vertical group was slightly smaller than that in the horizontal group (P=0.024) and the Index of Success (IOS) was slightly greater in the vertical group than in the horizontal group (P=0.013). Furthermore, the vault was significantly higher in the horizontal placement group than in the vertical placement group (P<0.001). Compared to the preoperative design, the absolute degree of rotation at 3 months postoperatively was 3.44° ± 2.72° for the horizontal group and 4.83° ± 2.93° for the vertical group. However, if the reference was changed to 2 hours postoperatively, the absolute rotation degree was 1.81° ± 1.84° for the horizontal placement group and 1.97° ± 1.70° for the vertical placement group. There was no significant difference in other parameters between the two groups.
Conclusion: Vertical placement of a toric ICL can have clinical effects and rotational stability as good as those with horizontal placement. Moreover, compared with horizontal placement, vertical placement can effectively reduce vault.
Vertical placement; Visual acuity; Rotational stability; Lens implantation
There will be 4758 million people worldwide with myopia and 938 million people with high myopia by 2050 [1]. The Implantable Collamer Lens (ICL) is a safe and effective option for the correction of myopia [2-5]. With no corneal excision and fewer high-order aberrations, it is often the first choice for surgical correction of high myopia [6,7].
The ICL is a good option for correcting astigmatism [8]. Bamashmus, et al., [9] demonstrated that ICLs for the correction of moderate and high astigmatism and myopia provided predictable refractive results with good satisfaction. Sari, et al., [10] reported that toric ICL implantation yielded a relatively predictable and stable refractive correction of myopic astigmatism over a period of three years. Nakamura, et al., [3] found that the ICL had good efficacy, stability and safety in the correction of astigmatism and myopia through ten years of follow-up.
Most of the postoperative risks are associated with the vault, which refers to the distance between the posterior surface of the ICL and the anterior surface of the crystalline lens [11]. Low vault may lead to mechanical contact with the lens or inadequate aqueous humour circulation, which accounts for the high incidence of anterior capsular opacity and cataract formation [12,13]. Conversely, high vault can cause excessive mechanical contact between the ICL and iris, leading to inflammation and increased intraocular pressure [14,15]. In addition, the occurrence of pigment dispersion syndrome, iris atrophy and acute angle-closure glaucoma has also been associated with high vault [16-18].
The ciliary sulcus of the eyeball has a vertical oval shape [19,20]. Some surgeons have reduced vault by placing the ICL vertically and have thereby achieved satisfactory results [21]. However, for toric ICLs, the stability of vertical placement and the effect of postoperative refractive correction have not been reported. Therefore, in this study, we compared the rotational stability and clinical outcomes of horizontal and vertical ICL implantation to explore the effect of different ICL placements.
Study design and participants
This retrospective case-control study was approved by the Lixiang Eye Hospital of Soochow University Institutional Review Board and adhered to the tenets of the Declaration of Helsinki. All patients were examined, treated and followed at the refractive surgery centre of Lixiang Eye Hospital between January 2020 and October 2020. A total of 36 eyes from 36 subjects with vertical toric ICL placement were recruited for this study. After strict 1:1 matching according to preoperative astigmatism, ICL size, sex and laterality, 36 eyes of 36 individuals with horizontal toric ICL placement were obtained as the control group. Informed consent was obtained from each subject before surgery.
The inclusion criteria for this study were as follows:
• Patients aged 18-45 years.
• Patients with myopia between -0.50 DS and -21.00 DS and patients with astigmatism between -0.5 DC and -6.00 DC.
• Patients with an Anterior Chamber Depth (ACD) equal to or greater than 2.80 mm.
• Patients with an endothelial cell density greater than 2000 cells/mm².
• No patients with ciliary body cysts, obvious cataracts, glaucoma or retinal disease history or systemic diseases.
One eye was randomly selected for binocular surgery and the eye receiving monocular surgery was the recruiting eye.
Preoperative and postoperative examination
All subjects underwent a complete preoperative examination, including logarithm of the Minimal Angle of Resolution (logMAR) of Uncorrected Distance Visual Acuity (UDVA) and Corrected Distance Visual Acuity (CDVA), Intraocular Pressure (IOP) by tonometry (noncontact tonometer; NT-530, Nidek Co., Ltd., Aichi, Japan), slit-lamp microscopy, fundus examination by a three-mirror lens and manifest refraction measured with a standard phoropter. Spherical Equivalent (SE) was calculated as the original spherical diopter plus half of the astigmatism value. A Scheimpflug camera (Pentacam, Oculus, Germany) was used to measure the White to White (WTW), flat K, steep K, mean K, Central Corneal Thickness (CCT) and ACD. Axial Length (AL) was obtained with an IOLMaster 700 (Carl Zeiss Meditec AG, Jena, Germany). The horizontal and vertical Sulcus-to-Sulcus (STS) diameters were measured using an Ultrasound Biomicroscope (UBM) equipped with a 50 MHz transducer.
Postoperative examination included UDVA, CDVA, manifest spherical power and refractive cylinder and IOP. In addition, the axis of the toric ICL was measured using the internal Optical Path Difference (OPD) map obtained by an OPD-scan III device (Nidek Technologies, Gamagori, Japan). The internal OPD map displayed the two markers located on both sides of the ICL optical region and the direction of the connection between the two markers could be easily measured using the instrument's built-in software, as described [22,23]. The postoperative time points selected for the study were 2 hours and 3 months after surgery.
All examinations were performed in a room with constant temperature and humidity controlled by an air conditioning system. Phoropter, Pentacam and OPD-Scan III examinations were conducted in the darkroom and all other examinations were conducted under standard room lighting conditions. Each test was performed by the same experienced physician or technician.
Surgical procedure
All operations were performed according to standard surgical procedures and were performed by the same surgeon. In brief, first, four horizontal and vertical marks were made on the limbus using the slit lamp before surgery. Then, after topical anaesthesia (proxymetacaine hydrochloride, Nanjing, China) was applied, a 3 mm temporal clear corneal incision was made. A V4c model toric ICL (STAAR Surgical Co, Monrovia, California) was inserted into the anterior chamber following viscoelastic agent (hyaluronic acid, Shanghai, China) injection. Then, the ICL was placed in the posterior chamber and adjusted to the planned position. Next, the viscoelastic agent was completely removed from the eye using a manual Irrigation/Aspiration (I/A) instrument. All surgeries were uneventful and no intraoperative complications were observed. Following surgery, tobramycin 0.3%, dexamethasone 0.1% eye drops (Tobradex, Alcon, USA) were administered four times daily for the first 5 days; dosages were decreased every 5 days. The power calculations for the ICL were performed according to the manufacturer’s guidelines using a modified vertex formula [24]. There were four ICL sizes such as 12.1 mm, 12.6 mm, 13.2 mm and 13.7 mm. The ICL size was also selected by the manufacturer-based WTW and ACD. Horizontal or vertical placement of ICLs was determined by STS. All the ICLs were placed within 22° horizontally or vertically.
Effect analysis
Changes in astigmatism were analyzed using vector analysis of the Alpins method. The Correction Index (CI) is calculated by dividing Surgically Induced Astigmatism (SIA) by Targeted Induced Astigmatism (TIA), which indicates overcorrection if the value is greater than 1 and under correction if the value is less than 1. On the other hand, the Index of Success (IOS) is calculated by dividing the Difference Vector (DV) by the TIA and smaller values represent better correction [25,26].
The Efficacy Index (EI) is the ratio of UDVA postoperatively to CDVA preoperatively and the Safety Index (SI) is the ratio of CDVA postoperatively to CDVA preoperatively.
Statistical analysis
Data analysis was performed using Statistical Package for Social Sciences (SPSS) 18.0 (IBM Corp., New York, USA). The Kolmogorov-Smirnov test was performed for all measurement data. Data with a normal distribution are expressed as the means ± Standard Deviations (SDs); otherwise, the data are expressed as medians and quartiles. A paired t-test was used to compare the parameters between the two groups. Spearman’s correlation analysis was used to analyse the associations between residual astigmatism and other related factors. A p-value of less than 0.05 was considered significant.
In this study, no intraoperative or postoperative complications, such as acute angle-closure glaucoma, infection or anterior sub-capsular cataract, occurred. No ICL need to be exchanged.
Baseline data of subjects are shown in Table 1. There was no significant difference in WTW between the two groups of subjects, but both the horizontal and the vertical STS were longer in the horizontal placement group than in the vertical placement group (P=0.003, <0.001, respectively) (Table 1).
| Characteristics | Horizontal placement (range) | Vertical placement (range) | P-value |
|---|---|---|---|
| Age, years | 26.42 ± 5.98 (18 to 45) | 27.08 ± 7.07 (18 to 47) | 0.667 |
| Sex (male/female) | 14/22 | 14/22 | - |
| Laterality (right/left) | 16/20 | 16/20 | - |
| UDVA logMAR | 1.53 ± 0.19 (1.10 to 1.70) | 1.55 ± 0.20 (1.10 to 1.70) | 0.635 |
| CDVA logMAR | -0.045 ± 0.051 (-0.18 to 0) | -0.033 ± 0.045 (-0.18 to 0) | 0.314 |
| Refractive errors (D) | |||
| Spherical | -7.22 ± 1.83 (-11.00 to -2.50) | -7.01 ± 1.81 (-1.025 to -3.25) | 0.629 |
| Cylindrical | -1.57 ± 0.54 (-2.50 to -1.00) | -1.57 ± 0.54 (-2.50 to -1.00) | - |
| Spherical equivalent | -7.99 ± 1.92 (-12.00 to -3.25) | -7.79 ± 1.83 (-11.25 to -4.00) | 0.662 |
| Keratometric value (D) | |||
| Flat K | 42.88 ± 1.10 (40.30 to 44.90) | 43.26 ± 1.11 (41.20 to 46.10) | 0.140 |
| Steep K | 44.62 ± 1.27 (42.10 to 47.00) | 44.96 ± 1.03 (42.40 to 47.00) | 0.218 |
| Mean K | 43.75 ± 1.16 (41.20 to 45.70) | 44.11 ± 1.04 (41.80 to 46.55) | 0.166 |
| ICL size (12.1/12.6/13.2/13.7) | 1/13/21/1 | 1/13/21/1 | - |
| Crystalline LT (mm) | 3.68 ± 0.27 (3.23 to 4.22) | 3.69 ± 0.30 (3.10 to 4.29) | 0.187 |
| WTW diameter (mm) | 11.66 ± 0.36 (11.00 to 12.30) | 11.56 ± 0.37 (10.80 to 12.20) | 0.215 |
| STS diameter (mm) | |||
| Vertical | 12.04 ± 0.35 (11.24 to 12.72) | 11.78 ± 0.37 (10.97 to 12.43) | 0.003 |
| Horizontal | 11.66 ± 0.37 (10.88 to 12.40) | 11.32 ± 0.40 (10.55 to 12.25) | <0.001 |
| IOP (mmHg) | 13.51 ± 2.82 (9.30 to 20.00) | 14.05 ± 2.51 (9.70 to 19.00) | 0.389 |
| ACD (mm) | 3.24 ± 0.19 (2.91 to 3.66) | 3.23 ± 0.23 (2.80 to 3.61) | 0.872 |
| AL (mm) | 26.77 ± 1.15 (24.21 to 28.54) | 26.41 ± 1.10 (23.65 to 27.43) | 0.187 |
Note: UDVA: Uncorrected Distance Visual Acuity; logMAR: logarithm of the Minimum Angle of Resolution; CDVA: Corrected Distance Visual Acuity; D: Diopters; K: Keratometry; ICL: Implantable Collamer Lens; LT: Lens Thickness; WTW: White-to-White diameter; STS: Sulcus to Sulcus; IOP: Intraocular Pressure; ACD: Anterior Chamber Depth; AL: Axial Length.
Table 1: Baseline clinical characteristics of the study eyes.
The clinical outcomes of the two groups are presented in Table 2 and Figures 1a and 1b, whereas Figures 1c and 1d describe the ICL rotation of the two groups The residual astigmatism of the vertical group was slightly smaller than that of the horizontal group (P=0.024) and the IOS of the vertical group was slightly greater than that of the horizontal group (P=0.013). In addition, the vault of the horizontal placement group was significantly higher than that of the vertical placement group (P<0.001), although the horizontal and vertical STS were larger than that of the vertical placement group. There was no significant difference in other parameters between the two groups (Figures 1a-1d and Table 2).
| Variables | Horizontal placement (range) | Vertical placement (range) | P-value |
|---|---|---|---|
| UDVA logMAR | -0.046 ± 0.059 (-0.30 to 0) | -0.055 ± 0.048 (-0.18 to 0.10) | 0.472 |
| CDVA logMAR | -0.120 ± 0.063 (-0.30 to 0) | -0.119 ± 0.072 (-0.30 to 0) | 0.948 |
| Efficacy index | 1.02 ± 0.17 (0.83 to 1.67) | 1.07 ± 0.14 (0.80 to 1.50) | 0.157 |
| Safety index | 1.21 ± 0.20 (1.0 to 1.67) | 1.24 ± 0.22 (1.00 to 1.67) | 0.472 |
| IOP (mmHg) | 13.25 ± 2.76 (9.10 to 19.70) | 14.01 ± 2.62 (9.20 to 19.00) | 0.421 |
| Vault | 612 ± 210 (280 to 1040) | 429 ± 173 (100 to 850) | <0.001 |
| Residual astigmatism (D) | -0.28 ± 0.27 (-0.75 to 0) | -0.16 ± 0.18 (-0.50 to 0) | 0.024 |
| Postoperative SE (D) | -0.07 ± 0.28 (-0.5 to 0.5) | -0.08 ± 0.30 (-0.75 to 0.38) | 0.883 |
| Correction index | 1.02 ± 0.17 (0.67 to 1.45) | 0.99 ± 0.11 (0.74 to 1.22) | 0.315 |
| Index of success | 0.20 ± 0.16 (0 to 0.5) | 0.11 ± 0.13 (0 to 0.5) | 0.013 |
Note: UDVA: Uncorrected Distance Visual Acuity; logMAR: logarithm of the Minimum Angle of Resolution; CDVA: Corrected Distance Visual Acuity; D: Diopters; IOP: Intraocular Pressure; SE: Spherical Equivalent.
Table 2: Clinical outcomes of the two groups.

Figure 1: Clinical outcomes and rotational stability. (a): Uncorrected Distance Visual Acuity (UDVA); (b): Residual astigmatism; (c): Rotation
relative to the preoperative design; (d): Rotation relative to 2 hours postoperatively. 
Tables 3 and 4 describe the ICL rotation of the two groups. Compared with the preoperative design, the amount of ICL rotation in the horizontal placement group was slightly smaller than that in the vertical placement group, although the difference did not appear to be statistically significant (P=0.052). In the horizontal placement group, the number of eyes with rotation of less than 5°, greater than or equal to 5° but less than 10° and greater than or equal to 10° was 25 (69.44%), 10 (27.27%) and 1 (2.78%), respectively, while that in the vertical group was 18 (50%), 16 (44.44%) and 2 (5.56%). However, when referring to the axial position two hours after surgery, there was no significant difference in the amount of rotation between the two groups. The number of eyes with rotation less than 5° and greater than or equal to 5° but less than 10° was 33 (91.67%) and 3 (8.33%) in the horizontal group, respectively, while it was 32 (88.89%) and 4 (11.11%) in the vertical group; there were no subjects with rotation greater than 10° in either group (Tables 3 and 4).
| Variables | Mean rotation (°, range) | Rotation <5° (n,%) | 5° ≤ rotation <10° (n,%) | Rotation ≥ 10° (n,%) |
|---|---|---|---|---|
| Horizontal | 3.44 ± 2.72 (0 to 10) | 25 (69.44%) | 10 (27.78%) | 1 (2.78%) |
| Vertical | 4.83 ± 2.93 (0 to 11) | 18 (50%) | 16 (44.44%) | 2 (5.56%) |
| P-value | 0.052 | - | - | - |
Table 3: Distribution of the absolute rotation degree in the two groups compared to the preoperative design.
| Variables | Mean rotation (°, range) | Rotation <5° (n,%) | 5° ≤ rotation <10° (n,%) | Rotation ≥ 10° (n,%) |
|---|---|---|---|---|
| Horizontal | 1.81 ± 1.84 (0 to 7) | 33 (91.67%) | 3 (8.33%) | 0 (0%) |
| Vertical | 1.97 ± 1.70 (0 to 6) | 32 (88.89%) | 4 (11.11%) | 0 (0%) |
| P-value | 0.692 | - | - | - |
Table 4: Distribution of the absolute rotation degree in the two groups compared to 2 hours postoperatively.
Figures 2a-2d shows the Spearman correlation analysis of residual astigmatism and other factors. Residual astigmatism seemed to have a weak negative correlation with axial length but no significant correlation with other factors (Figures 2a-2d).
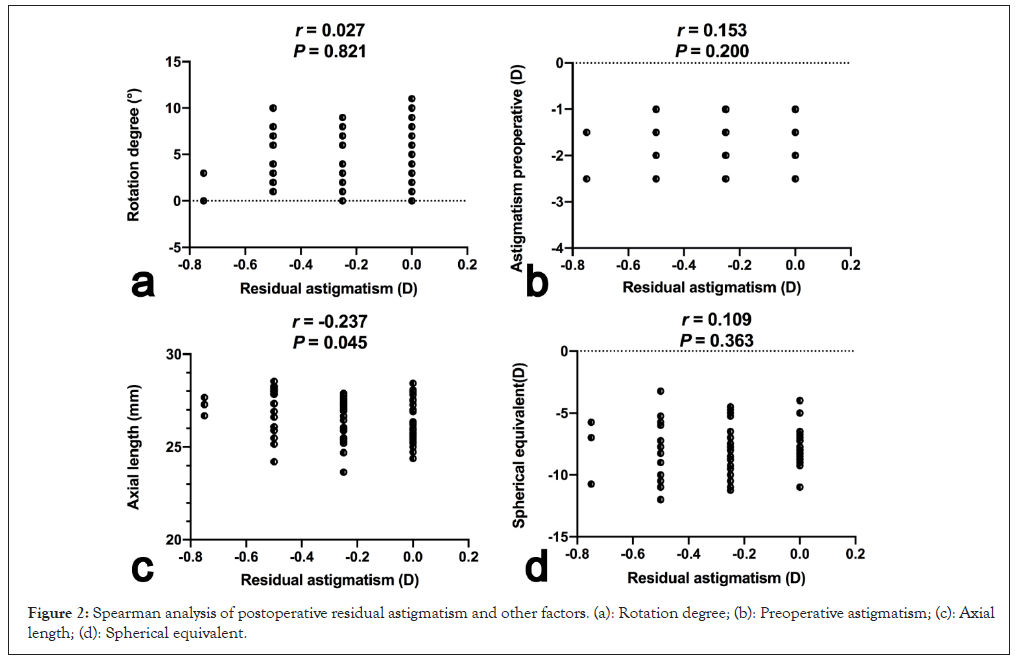
Figure 2: Spearman analysis of postoperative residual astigmatism and other factors. (a): Rotation degree; (b): Preoperative astigmatism; (c): Axial length; (d): Spherical equivalent.
In this retrospective study, we analysed the differences in visual and refractive outcomes, vault and rotational stability between horizontal and vertical toric ICL placement by strict 1:1 matched comparison. Although there have been several articles on the safety and efficacy of ICLs, as well as some reports on rotational stability, for the first time, our study investigated the differences in clinical outcomes and rotational stability of toric ICLs at different placement positions [27].
According to the recommendation of the Starr company, all ICLs should be placed within a horizontal 22° deviations (Visian ICL product information: Visian ICL for myopia. Available at: http:// www.accessdata.fda.gov/cdrh_docs/pdf3/p030016c.pdf). On the one hand, it is difficult to accurately measure the vertical corneal diameter. On the other hand, the rotational stability and clinical effect of vertical placement have not been reported.
Matarazzo, et al., [21] first reported a case of successful vault reduction by vertical placement of the ICL in their study. Subsequently, Kojima, et al., [28] and Fernandez, et al., [29] also reported several cases of extremely high vault reduction by rotation to the vertical position in their respective studies. In our study, the vault of the vertical placement group was significantly lower than that of the horizontal placement group (429 μm ± 173 μm vs. 612 μm ± 210 μm), although there was no statistically significant difference in white-to-white diameter between the two groups and even the horizontal and vertical sulcus-to-sulcus diameters were smaller in the vertical placement group than in the horizontal placement group. This might indicate that vertical placement of the ICL can effectively reduce postoperative vault, especially for patients at the critical value of ICL size selection and a larger size and vertical placement might be adopted to achieve an ideal vault.
The horizontal placement group in our study, similar to that in previous studies, had a good SI and effective index in terms of visual outcomes. In our study, the SI was 1.21 ± 0.20, no eye lost lines of CDVA and 66.67% of eyes gained lines of CDVA after the surgery. In addition, the efficacy index was 1.02 ± 0.17 and 100% of eyes had a UDVA of 20/20 or better. A recent study by Chen, et al., [30] found that the SI was 1.19 ± 0.23 and the EI was 1.04 ± 0.27 for ICL (model V4c) implantation. Similarly, Ye, et al., [17] also reported in their two studies that the safety factors of ICL implantation were approximately 1.11 ± 0.15 and 1.33 ± 0.60 and the efficacy factors were approximately 1.06 ± 0.15 and 1.14 ± 0.54. These reports were highly consistent with our results. On the other hand, in our study, the clinical outcomes of the vertical placement group were as good as those of the horizontal placement group, with a SI of 1.24 ± 0.22 and an EI of 1.07 ± 0.14. A total of 97.2% of eyes had a UDVA of 20/20 or better and 100% of eyes had a UDVA of 20/25 or better. There was no significant difference in postoperative UDVA between the two groups (-0.046 ± 0.059 vs. -0.055 ± 0.048, P=0.472).
Rotational stability is crucial for astigmatism correction by toric ICLs. In this study, OPD-scan III was used to measure the axial direction of the toric ICLs. Previous studies have shown that compared to conventional methods, OPD-scan III yields a lower standard deviation value and higher accuracy in measuring the axial direction of the toric ICL. In our study, the absolute degree of rotation at 3 months postoperatively was 3.44° ± 2.72° for the horizontal group and 4.83° ± 2.93° for the vertical group compared to that in the preoperative design. In the two studies in which the crystals were placed horizontally, the absolute degree of rotation at 3 months postoperatively was 3.75° ± 2.92° and 3.39° ± 2.36°, which were similar to the results for our horizontal placement group [31]. Rotation degrees appeared to be higher in the vertically placed group than in the horizontally placed group, although this difference was not statistically significant (P=0.052). However, if the reference was changed to 2 hours after surgery, the absolute rotation degree was 1.81° ± 1.84° for the horizontal placement group and 1.97° ± 1.70° for the vertical placement group. This suggests that most of the rotation measured at 3 months after surgery might have occurred within 2 hours after surgery and there was no significant difference in rotation degree between horizontal and vertical placement 2 hours postoperatively. There might be several reasons for this phenomenon. First, in the early postoperative period, the haptics of the ICL might not have been located in the right position of the ciliary sulcus and it was not sufficiently supportive of the ICL. With the narrowing of the pupil, the iris exerted a downward pressure on the ICL, which can cause the haptics to be better fixed in the corresponding position of the ciliary sulcus and in turn provide the ICL better stability; this is also one of the reasons for the change in the vault after lens implantation [32]. Second, there was usually some viscoelastic agent left under the ICLs in the early postoperative period, which made the ICLs easier to rotate and this part of the viscoelastic agent would be slowly metabolized. Third, because the upper and lower eyelids cover part of the limbus of the cornea, it is more difficult to create the upper and lower marking points, which might cause certain systematic errors. This might be the reason for the greater deviation of the vertical placement group relative to the planned axis direction.
In this study, we also analysed the influencing factors for postoperative residual astigmatism. Interestingly, postoperative residual astigmatism was not significantly associated with any of the three factors, including ICL rotation, except for a weak positive correlation with AL. In addition to rotation, there seem to be other factors that are more important in influencing postoperative residual astigmatism. We speculated that the stability of the ICL, such as its position deviation and tilt, might have a certain influence on postoperative residual astigmatism. We suspect that due to gravity, the two haptics on the bottom might be more conducive to support of the ICL, making it more likely to remain in the right position. This may explain why the residual astigmatism of the vertical placement group was smaller than that of the horizontal placement group. However, further research is needed to confirm the above speculation. Of course, there is an important premise for the above speculation, that is, the rotation degree of the ICL was small, less than 11° in this study. If the rotation degree was further increased, a large probability of postoperative residual astigmatism would be associated with the rotation degree. In addition, the postoperative residual astigmatism of the two groups was small, which was not enough to have a significant impact on postoperative visual acuity. Therefore, there was no significant difference in postoperative visual acuity between the two groups.
In this study, vector analysis by the Alpins method was used to determine the effect of the toric ICL on astigmatic correction in the two groups. The CI of the horizontal placement group was 1.02 ± 0.17 (range is 0.67 to 1.45), indicating slight overcorrection, while the IOS was 0.20 ± 0.16 (range is 0 to 0.5). For the vertically placed group, the Confidence Interval (CI) was 0.99 ± 0.11 (range is 0.74 to 1.22), indicating slight under correction and the IOS was 0.11 ± 0.13 (range is 0 to 0.5). There was no significant difference in CI between the two groups, while the results for IOS were similar to those for postoperative residual astigmatism. Lee, et al., [26] reported a CI of 0.91 ± 0.21 (range is 0.43 to 1.82) and an IOS of 0.17 ± 0.14 (range is 0.00 to 0.86) in their study on the clinical efficacy of ICLs and there was an IOS of 0.19 ± 0.11 (range is 0.01 to 0.39) in the study of Hyun, et al. [31], these findings were similar to the results from our horizontal placement group.
There are several limitations in this study. First, the sample size was not large compared with those of similar studies; however, we adopted a 1:1 paired study that controlled for other factors and consequently, this study was highly reliable. Second, the follow-up duration of this study was short, but by 3 months after surgery, corneal surgery-induced astigmatism is basically stable; thus, this time point is more commonly used for the study of postoperative astigmatism [33]. Finally, the ICL placement position in the participants included in this study was within 22° of horizontal or vertical. The other placement positions were not within the scope of this investigation and will be further analysed in follow-up studies.
This study demonstrated that vertical placement of the toric ICL can have clinical effects and rotational stability that are as good as those with horizontal placement. Moreover, compared with horizontal placement, vertical placement can effectively reduce vault.
We thank Dr. Chen Qing and Dr. Yu Peng for their help in patient management.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Zhu QJ, Xing XY, Zhu WJ, Zhu MH, Ma L, Yuan Y (2024) Rotational Stability and Clinical Effects of Different Toric Implantable Collamer Lens Placements: A Case-Control Study. J Clin Exp Ophthalmol. 15:978.
Received: 01-Apr-2024, Manuscript No. JCEO-24-30583; Editor assigned: 03-Apr-2024, Pre QC No. JCEO-24-30583 (PQ); Reviewed: 17-Apr-2024, QC No. JCEO-24-30583; Revised: 24-Apr-2024, Manuscript No. JCEO-24-30583 (R); Published: 02-May-2024 , DOI: 10.35248/2155-9570.24.15.978
Copyright: © 2024 Zhu QJ, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.