Clinical & Experimental Cardiology
Open Access
ISSN: 2155-9880
ISSN: 2155-9880
Short Communication - (2023)Volume 14, Issue 8
Sinus of Valsalva Aneurysms (SOVA) are classified as congenital or acquired. Congenital SOVAs are caused by the separation or failed fusion of the aortic media with the fibrous annulus of the aortic valve. A ruptured aneurysm in this location has historically been repaired surgically. However, since Cullen described the first percutaneous closure in 1994, this less invasive approach has been increasingly used and can be a viable alternative to closure in select cases. But severe AR and a ruptured SOVA still serve as disqualifiers for device closure. Beginning with our most recent case experience, we are going over the idea of the device closure option in RSOV with severe AR.
Sinus of valsalva aneurysm; Aortic regurgitation; Amplatzer duct occlude; Non coronary cusps; Ventricular septal defect; Transoesophageal echocardiography
In individuals with SOVAs, AR ranks second after Ventricular Septal Defects (VSD) in terms of the frequency of concomitant lesions. AR is more common in patients with ruptured SVAs, with 50% of ruptured SOVAs having concomitant AR requiring aortic valve surgery [1-3]. The aortic sinus and annulus lose their support in the presence of a ruptured SOVA. Additionally, the outflow from the rupture creates a Bernoulli effect, which tends to draw the associated aortic cusps away from the closure line, leading to inefficiency [4]. Chu have reported the presence of aortic incompetence in 35% of their cases. Aortic incompetence appears to be more common when there is an associated septal defect, i.e., 43.3%, as compared to 25.9% of patients who had an intact septum [5]. Choudhary reported that Aortic incompetence was found in 43.3% of their patients who underwent SOVA repair and in 17 (37.8%) it was severe. A retrospective review of the Mayo Clinic’s database showed AR in 44% of patients, and in 61%, it was severe [6]. The aortic valve was found to be deformed in 45 patients (43.26%) [5].
The operative mortality rate for ruptured SOVA is 1.9%-3.6% with 90% survival at 15 years [7]. The accurate mortality associated with percutaneous closure of ruptured SVA is not available due to the paucity of large-scale data, but multiple studies have shown good outcomes in selected patients.
Most SOVAs are asymptomatic before they rupture into adjacent structures. They usually arise in the right coronary sinus. As a result of the rupture, heart failure progresses, and if left untreated, patients with ruptured SOVA have a poor prognosis and high mortality rates. But considering the immediate intervention requirement and inoperable hemodynamic percutaneous device closure plays a vital role even if ruptured SOVA is associated with severe AR. Few case reports are showing that PC could be a viable option in severely ill patients with ruptured SOVA. Dobarro described a case in which severe AR developed after device closure [8]. Where they believed it to be related to prolapse of NCC caused by ADO device. The example we report here may mark the first instance of a ruptured SOVA with significant AR being successfully closed with a device.
The Venturi effect causing AR are classically been described in SOVA with peri membranous VSDs [9]. Here the high-velocity jet via VSDs generates a venturi effect which will pull away the aortic sinus/aortic cusps from closure, resulting in AR. Recently, a similar patient with ruptured SOVA aneurysm and severe AR but no concomitant VSD was encountered. In this instance, the venturi effect served as a blessing in disguise. We were unable to detect any intrinsic abnormalities in the aortic leaflets or annulus during the Transesophageal Echocardiogram (TEE) evaluation that could have caused severe AR. Hemodynamically the flow through the ruptured sinus produces the venturi effect, the tendency for the related aortic cusps to pull away from closure. Despite the fact that a ruptured SOVA with severe AR is a contraindication to ruptured SOVA device closure, we chose to do so because of the patient's deteriorating hemodynamic condition. Our hypothesis about mechanism of AR tested positive in the procedure when we kept a large sheath across the defect and the plastered aortic leaflet came back to its position decreasing the AR. This gave us confidence in proceeding with the device deployment. Once the device (22 × 20 mm ADO 1) was placed, TEE demonstrated rather surprisingly complete and proper coaptation of all three aortic cusps causing the disappearance of AR (Figure 1).
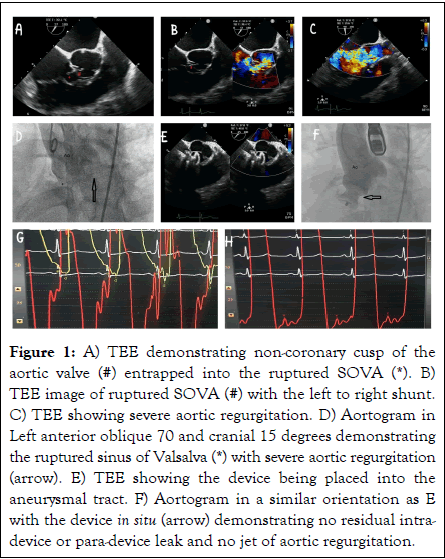
Figure 1: A) TEE demonstrating non-coronary cusp of the aortic valve (#) entrapped into the ruptured SOVA (*). B) TEE image of ruptured SOVA (#) with the left to right shunt. C) TEE showing severe aortic regurgitation. D) Aortogram in Left anterior oblique 70 and cranial 15 degrees demonstrating the ruptured sinus of Valsalva (*) with severe aortic regurgitation (arrow). E) TEE showing the device being placed into the aneurysmal tract. F) Aortogram in a similar orientation as E with the device in situ (arrow) demonstrating no residual intradevice or para-device leak and no jet of aortic regurgitation.
The physical displacement of the cusp back into its place after a large‐sized device across the defect into the sinus may act as contributing mechanism for the resolution of AR. However, it is yet unclear if the placement of the rigid device changes the mechanical behaviour of the neighbouring sinus wall, which may be essentially aberrant, or redistributes wall stresses. Ruptured SOVAs that have hemodynamically significant AR typically become candidates for surgical repair, however those who suffer entrapment of a leaflet due to the venturi effect might experience complete resolution of AR after device implantation.
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar ] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Kesavan V, Kumar D, Lanjewar CP (2023) Ruptured Sinus of Valsalva Aneurysm with Severe Aortic Regurgitation: Can a Device Modify the Puzzle? J Clin Exp Cardiolog. 14:835.
Received: 10-Aug-2023, Manuscript No. JCEC-23-26056; Editor assigned: 14-Aug-2023, Pre QC No. JCEC-23-26056 (PQ); Reviewed: 28-Aug-2023, QC No. JCEC-23-26056; Revised: 04-Sep-2023, Manuscript No. JCEC-23-26056 (R); Published: 11-Sep-2023 , DOI: 10.35248/2155-9880.23.14.835
Copyright: © 2023 Kesavan V, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.