Journal of Nutrition & Food Sciences
Open Access
ISSN: 2155-9600
ISSN: 2155-9600
Review Article - (2022)Volume 12, Issue 6
The goal of this study is to conduct a scoping evaluation of the global evidence on m-health interventions and to determine the efficacy of mobile based self-management interventions for type 2 diabetes mellitus.
A rigorous search of the PubMed and Scopus research databases was conducted. Studies on Type 2 diabetes conducted in age ranges 18-75 years and published in English worldwide from 2010 to 2020 are included. Randomized controlled trials (RCTs) using mobile based self-management for type 2 diabetes patients, as well as recording and analysis of results at the patient level, were among the studies. The studies were checked by the reviewer, and they were then independently reviewed by a second reviewer. The data was extracted, graphed, and the studies' quality was evaluated. To deliver study outcomes and 27 recommendations, the scoping study approach employs Arksey and O'Malley's operational framework. This work is presented using the PRISMA-SCR checklist.
The assessment comprised a total of 40 articles, all of which were RCT-based treatments studies with over 3800 participants. For this study, 40 original research publications were chosen. The chosen studies mostly focused on type 2 diabetes self-management (N=40) and hypertension self-management (N=2). The usage of mobile SMS (N=17) or mobile on phone (N=12), the content of session education with mobile (N=10) or the placement of mobile devices (N=4) were among the several treatments. The therapies were usually successful, resulting in better glucose control and improved health indices.
Conclusion: For patients with type 2 diabetes, mobile based self-management interventions appear to have beneficial benefits on self-care and management, as well as meaningful outcomes. Overall improvement in physiologic markers, self-care, and patient quality of life in Type 2 Diabetes patients. Though the research focused on results in small populations, there was little indication that the intervention will be scaled up in the future. Furthermore, the findings suggest that more research into self-management, which includes nutrition informatics in a self-care management regime, is needed, with a particular focus on the availability of nutrition informatics by area. This will also aid in diabetic and cardiovascular disease co-management. In low and middle income countries (LMICs), self-management looks to be an effective way of improving health outcomes, hence mobile-led selfcare management treatments incorporating nutritional informatics may be beneficial.
Type 2 diabetes; Self-management; Telehealth; m-Health; Chronic care management; Mobile health (CCM)
Background
Diabetes is a major public health issue in India and around the world. It has a negative impact on one's quality of life and is one of the most common causes of mortality and disability. Diabetes affects approximately 463 million persons worldwide, posing a significant threat to global health. By 2030, 578 million people will have diabetes if no action is taken to combat the pandemic. By 2045, 700 million people will be affected by this alarming trend. According to the IDF Atlas, 1 in every 6 people in India has diabetes, and diabetes is responsible for 1.2 million fatalities. This epidemic has afflicted 77 million people in India between the ages of 20 and 79, with a total cost of $ 8 billion in health expenditures, resulting in a massive burden and significant economic cost to public health. Type 2 diabetes mellitus is notorious for being one of the most challenging chronic illnesses to manage. Diabetes problems and the integration of sophisticated self-management treatments into daily life result in elevated levels of discomfort, frustration, and discouragement, all of which have a negative impact on a person's well-being. Nonetheless, patients and their families are responsible for most of the diabetes management, and the self-management regimen has shown to be the backbone of diabetes care.
Overall, diabetes complications must be carefully treated to prevent hospital admissions, morbidity, and mortality because of the pandemic. M-health treatments can help people manage their own health problems and contribute to universal health coverage [1]. The m-health application can be built for a better self-management regime with nutrition informatics, which the American Association of Physicians of Indian Origin (AAPI) recommends for diabetic care in the Indian community [2]. Mobile health, often known as m-Health, is the use of mobile and wireless technology to help people reach their health goals. Patients, clinicians, and pharmacists are gradually adopting mobile health, or m-health. Telehealth and telemedicine overlap with mHealth. Nonetheless, the phrases telemedicine and telehealth refer to all information and communication technologies used to improve clinical care, as well as public health administration and education. According to the National Health Authority of India, there are around 1.18 billion mobile phone users and 600 million smartphone users in India, with the number of smartphone users increasing by 25 million every quarter [3].
Model of self-care management
The self-management regime is a way for improving habits to attain goals by actively engaging in self-care activities. Meal nutrition planning, physical activity planning, blood glucose monitoring, diabetes medications, and dealing with high and low sugar levels with bouts of sickness are all part of self-management. In conjunction with the participants, various health care providers such as doctors, nurses, nutritionists, and pharmacists prepared Self-management action plans [4].
Self-care is a basic and integral aspect of treatment in the Chronic Care Model (CCM), and patients who have improved clinical results and engage in self-care management have a better quality of life, fewer hospitalizations, and a longer survival time [5].
Over the last decade, there has been an increase in the amount of information available on self-care management, possibly due to the availability of self-report instruments. Glycemic management is also monitored, which necessitates self-monitoring glucose levels several times each day and changing insulin, food, or physical exercise as appropriate. Management of type 2 diabetes patients is frequently centered on lifestyle changes (diet and physical exercise), and oral hypoglycemic medicines may be employed. To achieve optimal glycemic control, type 2 diabetes patients may use insulin in addition to or instead of other drugs. Diabetic self-management has been regarded as a cornerstone of diabetes care for decades. Healthy eating, physical education, diabetes physical activity, medication, and device usage; monitoring and using patient generated data to adjust behavior and medication doses; preventing, detecting, and treating acute and chronic complications; coping with psychosocial issues, and problem solving are all examples of self-care management.
What is known about the subject already?
In Chronic Care Management (CCM), self-care management has the potential to enhance health outcomes and lower the risk of diabetic complications. Mobile phone based technology, often known as m-health, has been employed in a variety of global programs aimed at self-care management. Patients' self-efficacy, self-care behaviors, health related quality of life, and clinical results are all being studied in several ways [6]. However, most m-health applications developed are clinical in nature and do not address self-care issues such as nutrition, diet, exercise, or blood glucose testing. Numerous studies on various self-care strategies have been conducted; however, no studies have ever been compared across conditions and outcomes to determine whether therapies are successful [6].
What will this paper contribute to?
This study demonstrates the effects of mobile phone based self-care and management interventions on enhancing self-efficacy, self-care management activities, health related quality of life, and clinical outcomes in patients with type 2 diabetes mellitus. The scoping review of various m-health self-care interventions can offer insight into building effective approaches, self-care management, and broader applicability on models for developing m-health that can be produced and tested on a variety of patient groups.
The mobile health app Healthcare has the potential to improve support for patients with type 2 diabetes and it is critical to improve patient outcomes by improving self-care management and incorporating nutrition informatics. Additionally, psychological support can help patients cope with diabetes and adhere to self-care activities. Most studies focused on healthy lifestyle practices such as physical activity and glucose testing. However, integrating diabetes management with signs and symptoms management and a nutrition regimen can be the most difficult self-care behaviors for patients. The goal of a scoping review is to determine whether a project is feasible.
The goal of this scoping review is to use the PRISMA-SCR tool to gain a better knowledge of various m-health enabled nutrition informatics treatments to assist type 2 diabetes self-care at home.
Question for research
• What is the scope and need for a health enabled nutrition informatics intervention in self-care management of type 2 diabetes at home?
• What is the current global m-health self-care management regime for nutrition informatics interventions in type 2 diabetes chronic care management?
A scoping review or scoping study is a sort of knowledge synthesis that addresses an exploratory research topic by carefully examining, choosing, and synthesizing existing knowledge to map key concepts, types of evidence, and gaps in research linked to a given region or field" [7]. A scoping review was undertaken systematically using Arksey and O'Malley's methodological framework to discover relevant research, select studies based on predetermined criteria, extract data, and analyze, summarise, and present results [8]. To improve reporting and fidelity, the Preferred Reporting Items for Systematic Reviews and Meta-analyses for Scoping Reviews (PRISMA-SCR) were utilized.
This review of available literature did not require ethical approval.
There are five steps to a scoping study.
(Arksey and O'Malley's methodological framework)
1. Determine the research question.
2. Locate a study that is relevant.
3. Pick a subject to research.
4. Make a graph of the data.
5. Compile and summarize the report (Figure 1).
Figure 1: Steps to a scoping study.
Searching Techniques
• To appropriately classify original works to address the research questions, I would use PubMed and Scopus searches.
• Developed an initial search technique to discover relevant search phrases (keywords differ amongst databases).
• To be considered, works must have been published between 2010 and 2020.
Criteria for acceptance
• Studies that have been published in PubMed and the Scopus Library.
• Publications that are written in the English language.
• Between 2010 and 2020, a number of books were published.
• Self-care management and type 2 diabetes self-care, chronic care management, person centered care.
Criteria for exclusion
• Published prior to 2010.
• Not in a peer-reviewed journal or article.
• Publication in a language other than English.
• Letters, editorials, news stories, and conference abstracts are all welcome.
• The study did not make use of any technology.
Choosing a study
The keywords and abstracts of various researches were assessed, followed by technological assessments, and then full-text publications were examined for eligibility. The data from 38 study abstracts were plotted in a chart and a table was created, which led to the answers to the research questions.
Three more criteria were incorporated in the research review:
1. One or more reference databases were evaluated;
2. Inclusion and exclusion criteria were applied; and
3. The risk, bias, and quality of related investigations were assessed.
In addition to the primary studies discovered through scoping reviews, inclusion and exclusion criteria were used for the supplementary searches.
Extraction of data at the study level
The study design, population, setting, interventions, comparator, and findings were all retrieved in detail. We checked data for accuracy and extracted data on difference in differences, including p-values and confidence intervals (CI) if available and pre-post-differences in intervention and control groups if not, deciding on the significance of the findings in the study we decided "yes" if the study showed a significant between group difference and "no" if the study showed no significant between group differences, "could not determine" if the study showed no significant between.
Design of the research
Randomized controlled trials (RCTs), non-RCTs, and other observational studies with a comparator were all included. Registry studies were included to offer information on hazards that were not reported in another research. Studies that simply looked at pre-post differences in a particular group were eliminated.
We included studies in English as well.
Populations include
Adults (18+ years old) with type 2 diabetes made up the whole study population.
Exclude: Children, teenagers, pregnant women, people with prediabetes or diabetic risk factors, and women with gestational diabetes are all at risk.
Interventions contain
For diabetic self-management, use a mobile device (phone, tablet, or watch). At least one of the following must be included in any intervention.
Exclude: Artificial pancreas; texting interventions; medical gadgets that do not connect to a mobile phone or tablet (e.g., blood glucose meter).
Aspects to consider
No comparator but part of a registry study; usual care or another mobile or nonmobile diabetes self-management program; no comparator but part of a registry study
Outcomes include
Every patient's outcome
Exclude: Health care provider outcomes, health care system outcomes, and technology performance results
Synchronization/settings include
Any setting any length of study; only papers published after 2010 are eligible and in English. Included in the study design are Randomized controlled trials, nonrandomized controlled trials, or another observational study with a comparator are all examples of studies with a comparator (Figure 2).
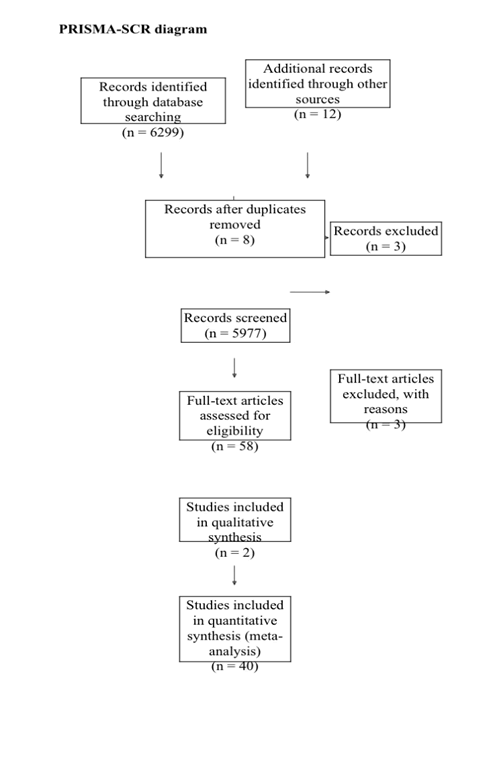
Figure 2: PRISMA-Scoping review diagram.
Characteristics of the 40 reviews included in the study
The examination of 40 papers, the majority of which were conducted in the United States, focused on the detailed research features of the 40 reviews: more than ten studies were conducted in the United States. Other experiments were conducted in Australia (n=1), Canada (n=1), China (n=3), Germany (n=1), New Zealand (n=1), South Korea (n=1), Spain (n=1), and the United Kingdom (n=1), with a total of n=1. More than 18 of the evaluations were based on clinical trials, with 9 of them consisting solely of RCTs and 6 including quasiexperimental studies. Six RCTs were used to conduct eta-analyses for diverse health outcomes. When comparing the intervention and control groups, the mean difference was computed by subtracting the level of clinical outcomes at the end of follow up from the baseline. This enabled a comparison of clinical improvement because of mHealth interventions vs the control group.
Mobile health interventions: What are they and how do they work?
There are several types of mHealth intervention studies.
1. Mobile application based, which uses smartphones as a medium to self-manage and assist patients in improving their health/ ailments
2. Advice on self-management by using web-based tools to assist patient instruction and information on self-management
3. Mobile text messaging SMS, which is the primary mode of communication between patients and health care providers
4. a portable monitoring device/personal digital assistant (PDA), which is typically used to monitor and assist patients in improving their health/ailments The most extensively examined intervention type was mobile apps (15 studies), followed by text messaging (11 reviews), and personal digital assistants (11 reviews) (5 reviews).
Self-monitoring and management were the most common targeted functions of the mHealth interventions assessed (15 reviews), followed by education or health promotion (8 reviews), reminders, or alerts (5 reviews).
As outcomes, all 40 evaluations looked at changes in clinical biomarkers, while 9 looked at health-related behaviors and 7 looked at treatment adherence. Although there is a lot of interest in mHealth therapies for the treatment of diabetes and obesity among researchers, health care workers, and patients, little is known about their effectiveness. Furthermore, the utilization of mobile health solutions for these illnesses is still limited. This is the only study that we are aware of that presents a complete review of evidence on the effectiveness of mHealth therapies for these illnesses. The assessment included 40 articles, all of which were RCT-based treatments studies with over 3800 participants. For this study, 38 original research publications were chosen. The selected studies mostly focused on type 2 diabetes self-management (N=38) and hypertension selfmanagement (N=2). The use of mobile SMS (N=17) or mobile on phone (N=12), the content of session education with the use of mobile (N=10) or the location of mobile devices (N=4) were among the several treatments. The therapies were usually successful, resulting in better glucose control and improved health indices.
The results of published research have been mixed. This systematic review looked at evidence from 38 evaluations that looked at a total of 55,604 original papers and showed that the impact of mHealth interventions on diabetes management is promising in general, especially in the areas of glycemic control and weight management. The majority of the 20 reviews focused on mHealth's self-monitoring capabilities. To date, the most common mHealth interventions have been text messaging and health apps. Despite this, all 17 reviews indicated that mHealth was practical and might potentially enhance health outcomes among type 2 diabetes patients.
I'd sort the results by target audience, intervention kind, study duration, sample size, intervention duration, and assessed outcomes (Table S1) [9-45].
More thorough study designs and approaches are needed for future scoping reviews and evaluations of mHealth interventions to draw more precise conclusions about their use and effectiveness for type 2 diabetes management. User experiences, ratings, and experiences may be used in the development of evidence based interventions for m-health app design. The effectiveness of patient and user engagement with these mHealth apps is still unknown, and apps must be user-friendly, engaging, and human centered.
In behavioral change, patient centered self-monitoring with tailored feedback is critical, and it has been found to boost user engagement and adherence. The effectiveness and target on mHealth incursions could be improved by making app functions relevant to users based on their age and sex, type of diabetes, and geographical area. Several validation tests and, when necessary, rules will be required to support an evidence based approach to mHealth use for diabetes treatment. When researching behavioral changes following mHealth interventions, validated metrics and objectives should be used. Furthermore, because most previous reviews did not include studies conducted in these target groups/populations, it is necessary to identify and focus on a high risk population with low socioeconomic status.
The 40 identified reviews had a high amount of variation in their characteristics and findings, according to the analysis results. Because of the various study designs, settings, objectives, and context, it was difficult to clearly describe the value of mHealth therapies across reviews. Despite these limitations, this study provided a better degree of analysis and a comprehensive presentation of the findings in the rapidly emerging field of mHealth. The current study has various unique contributions as compared to earlier studies, including the following:
1. Whereas previous studies were general and narratively described mHealth effects on diverse diseases using a small number of lowquality articles, our study added quantitative evidence specifically on the applications of mHealth in diabetic research and studied objective changes in biomarkers, treatment adherence, and health behaviors after a mHealth intervention
2. We conducted a meta-analysis on the intervention effects of clinical outcomes, which was lacking
3. We conducted a meta-analysis on the intervention effects of clinical outcomes, which was lacking. This aids in the identification of best practices for combating the diabetes and obesity epidemics. In addition, we found that mHealth interventions consistently reduced HbA1c and body weight across multiple reviews.
Finally, the outcomes of the 17 reviews, including six meta-analyses published since 2005, revealed promise but limited data on the effectiveness of mobile health interventions for diabetes control. The key target functions and application kinds of mHealth researched in the field include self-management, monitoring, and the use of text messaging and apps. Future studies should use more rigorous study designs to investigate the impact of mHealth interventions on diabetes and obesity control. Studies are needed to determine the best formats and frequency of contacting patients using theory based interventions; to better tailor messages to the specific needs and communication styles of recipients; and to improve usability by adapting approaches to recipients with varying degrees of technological and health literacy, thus placing a greater emphasis on maintaining effectiveness over time. To summarize, the scoping study reveals a small number of digital health interventions for persons living with NCDs in India, which is rapidly expanding. Most intervention studies have found a wide variety of favorable health outcomes because of the therapies, highlighting the potential for reducing health problems among people with various NCDs. Nonetheless, in addition to the current evidence, our study highlights the limitations that may have an impact on the overall development of digital health interventions for NCDs in India. These limitations and challenges are crucial for the widespread adoption of evidence based therapies, as well as the development and implementation of innovative interventions for NCD patients. To promote patient centered NCD treatment in India in the digital era, future research and practice should involve important stakeholders and address challenges raised in this study.
The authors are the only contributors to this manuscript and are acknowledged.
All authors have contributed to the design of the study, development of the questionnaire, preparation of the manuscript, and have approved the manuscript for publication.
None.
[Crossref]
Citation: Abhijeet PS, Manmohan S, Mansi G, Ashish J (2022) Scoping Review Using PRISMA-SCR on m-health Interventions on Self-care Management of Type 2 Diabetes at Home. J Nutr Food Sci. 12:864.
Received: 20-Jun-2022, Manuscript No. jnfs-22-17986; Editor assigned: 22-Jun-2022, Pre QC No. jnfs-22-17986 (PQ); Reviewed: 06-Jul-2022, QC No. jnfs-22-17986; Revised: 11-Jul-2022, Manuscript No. jnfs-22-17986 (R); Published: 18-Jul-2022 , DOI: 10.35248/2155-9600.22.12.1000864
Copyright: © 2022 Abhijeet PS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.