Journal of Phonetics & Audiology
Open Access
ISSN: 2471-9455
ISSN: 2471-9455
Research Article - (2016) Volume 2, Issue 2
Introduction: Newborn hearing screening has enabled the professionals to successfully detect a hearing loss at earliest. Successful hearing screening protocol involves a battery of tests, which should have high sensitivity and reduced false positive and negative responses. Moreover, protocol should be cost effective and less time consuming. Such protocol calls immediate implementation in screening program to detect hearing loss and certainly benefit beneficiaries to enroll in habilitation and or rehabilitation.
Objective: To investigate sensitivity and specificity of individual and combined physiological hearing tests utilized in newborn hearing screening program.
Method: A total of 572 ears (286 infants) were screened using high frequency tympanometry, acoustic reflex measure and transient evoked oto-acoustic emission (TEOAE). Despite all screening tests were passed auditory brainstem response (ABR) was measured at 30 dBnHL for confirmation of normal hearing. However, in ear where either acoustic reflex threshold for broadband noise or TEOAE was failed then detailed diagnostic ABR was carried out.
Results: Sensitivity, specificity, false negative and false positive responses of individual test and combined physiological tests were determined. Results showed combined physiological measure revealed higher sensitivity (86%) and specificity (96%) and reduced false positive (0.3%) and false negative (1.3%) than each physiological measure.
Conclusion: The protocol of combined physiological test in hearing screening accounts reduced false positive response there by decreases number of referrals. This in turn certainly reduces unnecessary parent tension regarding hearing status of their ward.
Keywords: Screening; Hearing; Tympanometry; Acoustic reflex; Sensitivity; Rehabilitation; Auditory brainstem response
Hearing screening applies to a large population with no apparent signs or symptoms of the target disorder. Roush [1] defined screening program as a designed approach that separates disease group from clinically normal group. In any screening instrument four sets of result can be expected when administered on target population. In case of hearing screening they are, true positive (presence of hearing loss), true negative (absence of hearing loss), false positive (though in the absence of hearing loss, screening instrument indicate presence of hearing loss), and false negative (though in the presence of hearing loss, screening instrument indicate absence of hearing loss). The outcome of false positive result is costlier because patient has to undergo unnecessary detailed diagnostic evaluation. It consumes time and financially expensive for the patients. On the other hand, outcome of false negative is more erroneous, as this result definitely harm patients and falsify the statement of ‘early identification and intervention’. Additionally wrong information will be conveyed to the patient. Thus, screening hearing test should have higher sensitivity (true positive) and specificity (true negative). From many decades effort have been made to identify hearing loss at the earliest through new born hearing screening program and provide intervention as early as possible to avoid consequence of hearing loss.
In clinical practice immittance measure commonly used to inspect middle ear status, which uses either 226 Hz or 660 Hz; 1000 Hz test tones. Tympanometry using 226 Hz is not sensitive to detect all middle ear diseases [2]. The result obtained from 226 Hz probe tone produces more of false positive and false negative responses [3]. This is because the 226 Hz probe tone is not sensitive to detect pathology in mass component of middle ear. However, studies with the 1000 Hz probe in neonates have been shown to be efficient to detect middle ear alterations [4,5] opined that infant middle ear system is mass dominated and thus energy transferred is relatively more through high frequencies. A normal shaped single peak tympanogram is typically observed for probe tone frequency of 1000 Hz, if the middle ear is aerated and the ear canal is free from prolapsed. However, asymmetrical notched peak were also noted in infants [4]. Baldwin [6] reported tympanometry of 1000 Hz represented 92.3% of specificity in infants having normal middle ear status and remaining 7.7% showed false positive. In yet another study by Marchant, [7] reported sensitivity of 99% and specificity of 89%.
Acoustic reflex is one among the test battery used to evaluate hearing function at the level of brainstem in which test completes rapidly and easy to administer [8]. Acoustic reflex involves bilateral contraction of middle ear muscles in response to high level sound presented to either ear [9]. Acoustic reflex threshold is the lowest level of a sound at which a change in acoustic admittance of the ear is monitored. The clinical implication of acoustic reflex threshold is to predict pure tone thresholds [10] also to detect the presence and absence of sensorineural hearing loss. Keefe [11] studied acoustic reflex using broadband noise. The median value of acoustic reflex threshold elevate by 24 dB in infants, who had passed in acoustic reflex using broadband noise. Mazlan [8] reported 100% specificity in healthy newborn using acoustic reflex elicited by broadband stimulus. In yet another study by Nozza, Bluestone and Kardatzke [12] who reported that combined use of acoustic reflex and tympanometry revealed 86% of specificity and remaining 14% leads to false positive outcome.
Otoacoustic emission (OAE) is yet another test to assess the integrity of outer hair cell function [13]. Transient otoacoustic emission (TEOAE) is most commonly used in clinic, as it is easy to perform and the result obtained from this test is fast and accurate. Further, sensitivity and specificity of TEOAE test is 67.1% and 85.0% respectively [14]. It is elicited by brief stimulus i.e., click stimulus presented either in linear or nonlinear manner. However, absent TEOAE are noted in patients with from moderately severe hearing impairment [14]. Additionally, though the integrity of cochlear function is normal, absent OAE is because of middle ear pathology as it obstructs the emission path [15]. Thus, above mentioned strength of TEOAE made several investigators to utilize in test battery to assess the middle ear and cochlear hearing status of infants.
Though OAE is sensitive to identify cochlear lesion leading to hearing loss, false positive result is more likely in the presence of mild conductive pathology and also in auditory neuropathy spectrum disorder. Thus, in screening protocol, including both tympanogram and OAE helps to differentially diagnose the presence of hearing loss attributed either by conductive or sensory pathology. However, the sensitivity and specificity is 92.5% and sensitivity is 98.6% [16]. OAE and tympanometry in screening protocol is sensitive to identify the pathology confined to middle ear and or cochlear part of ear leading to hearing loss, false negative is more likely. That is the outcome of these test infers absence of hearing loss but actually pathology present in the retro-cochlear pathway. In yet another combination of test such as in tympanometry and acoustic reflex, false negative is commonly seen though cochlear lesion attributed mild hearing loss in infants. Further, in OAE and acoustic reflex, mixed result is more likely because in mild hearing loss OAE will be absent and reflex might be present which leads to confusion in diagnosing hearing status.
From the literature review it is noted that individual test has questionable sensitivity and specificity in identifying the hearing loss attributed by particular part of the ear. Administering individualized test might miss to identify pathology at the different part of auditory system. Hence, there is a need to have combined physiological hearing screening tests, which identify pathology pertain to different parts of ear using non-invasive method. It is thus hypothesized that combined physiological hearing screening tool is more accurate than individualized test. The present study focused to solve research question on sensitivity and specificity of individualized test and combined physiological hearing screening tests.
Newborn hearing screening program for infants who are at risk require special attention, as there is high chance of its manifestation on hearing impairment. Hearing screening program helps the audiologists, medical and nonmedical practitioners to detect the hearing loss to the earliest in infants, thereby its negative consequences might be minimized [17]. Hearing screening program should include a test battery such that it is sensitive enough to identify hearing loss in infants who genuinely suffer from hearing impairment and also to specify normal hearing status in which the hearing sensitivity is well within normal limit. Thus, the present study aimed to investigate percentage of sensitivity and specificity in individualized test and combined physiological tests. The following objectives were formulated a) to determine sensitivity and specificity of each hearing test (tympanometry using 1000 Hz, ART (BBN) and TEOAE), b) to investigate sensitivity and specificity of combination of hearing tests and c) to differentiate between types of hearing loss from combined hearing tests.
Participants
A total of 286 (572 ears) infants were involved in the study. High risk register was administered to each parent infant. The number of infants in each category is tabulated in Table 1. Further, information about the child’s detailed pre-, peri- and postnatal history, family history and other relevant information were obtained from medical record section and through personal interview with the parents. The chronological age at the time of testing ranged from 2nd day to 15th day with mean age of 4 days. External ears abnormality or any other conditions, which prevent the completion of either one of the tests, were excluded from the study.
| SI.No | Categories | Number of infants |
|---|---|---|
| infants | ||
| 1 | Without any risk factors | 180 |
| 2 | History of consanguineous marriage | 20 |
| 3 | Positive family history of speech and hearing problems | 11 |
| 4 | Hyperbilirubinemia | 24 |
| 5 | Low birth weight | 40 |
| 6 | Birth asphyxia | 11 |
| Total | 286 |
Table 1: Representation of number of infants under each category.
Instruments
The following instruments were used in the present study. Middle ear analyser GSI tympstar (version 2) was used to obtain 1000 Hz probe tone tympanogram and also to record acoustic stapedial reflexes (ASR) for broadband noise stimulus. Natus Biologic Auditory evoked potential (version 6.3.0) was used to record auditory brainstem responses as part of diagnostic procedure. Same instrument was also used to record transient evoked oto acoustic emissions (TEOAE) using the SCOUT OAE software.
Procedure
All the tests were carried out sound treated room with ambient noise levels within permissible limits [18]. The procedure involves two stages. In stage-1 screening tests such as tympanometry using 1000 Hz, ART(BBN) and TEOAE were performed on each infant. In stage-2, diagnostic auditory brainstem response was carried out on infants who have failed either in one of the screening tests or indicate risk factor for hearing loss outlined in Table 1. In addition, ABR was performed at 30 dBnHL on those infants who have passed in all screening tests and no indicative of risk factor.
Stage-1: Hearing screening tests procedure: Three tests were performed on each infant. It includes physiological hearing screening tests such as tympanometry using 1000 Hz, ART(BBN) and TEOAE. All these screening tests were carried out in sound proof room in which the permissible noise level was with respect to standards of American National Standard Institute. The order of physiological hearing screening tests was randomized and it was purely based on the state of infants.
Tympanometry for 1 KHz: The probe was inserted into the infant test ear of ear canal by pulling the helix part of pinna slightly upward and backward. After ensuring proper seal, a probe tone of 1 kHz was delivered at 75 dB SPL. Ear canal pressure was varied from 200 to -400 daPa at a pump speed of 600 daPa/sec [14,19]. An admittance tympanogram which plots uncompensated admittance (in mmho) against ear canal pressure (in daPa) was obtained. For reliability, the test was repeated. The static admittance at the peak pressure was calculated by subtracting the admittance obtained at the peak with that obtained at the positive extreme pressure. The criterion used for pass was an admittance value greater than or equal to 0.1 mmho [19].
Acoustic reflex threshold (ART) for broadband noise stimulus: Acoustic reflex threshold was done immediately after tympanometry using same instrument in screening mode. Stimulus used was broadband noise presented at 85 dB SPL. Intensity level was changed automatically until a change in admittance greater than or equal to 0.03 mmho [8] was noted and it was accepted as reflex level.
Recording and analysis of the otoacoustic emissions by transient stimulus (TEOAE): TEOAE recording and analysis procedure was adopted from Finitzo’s criteria [20]. Oto-acoustic emission was collected for click stimulus with the duration of 100 μsec, which was presented at 75-83 dBpeSPL. The presentation rate of the clicks was 10/ sec. Click stimulus of 250 sweeps were delivered to the test ear using Etymotic ER-2 insert earphone. The output was fed to an analog-digital converter at a sample rate of 48,000 Hz /sec. The response of 250 clicks was average as followed. The 40 ms sample of response window to the set of 4 clicks (linear manner) was summed with the previous set of clicks in that sequence. Additionally, if the noise level exceeded 45-52 dBpeSPL, the recording was paused and continued once the noise level reduced below the rejection level. OAE data was considered, if the accepted number of sweeps is well above 85%. Three trials were obtained in the test ear on same participants to check the reliability of TEOAE. TEOAE was considered present (i.e., pass criteria) when the signal/noise ratio of 3 dB in four out of five half-octave bands.
Stage-2: Diagnostic Procedures: Purpose of diagnostic evaluation for all babies was to detect hearing impaired babies because of the low incidence of hearing impairment in the general population (< 1%). Further to calculate true sensitivity and specificity, and also to document false- negative and positive rates accurately. To iterate, in those ears where all the screening tests were passed and no indicative of risk factor for hearing loss then ABR was performed at the intensity of 30 dBnHL using click. However, in ear whom either one screening test was failed or indicative of risk factor then detailed diagnostic ABR procedure was carried out. Further, if in any case, click ABR was absent then tone burst ABR for 500 Hz was performed.
Auditory brainstem responses for click and tone burst for 500 Hz stimuli: Auditory brainstem response was recorded by far field recording using Biologic Auditory evoked potentials version 6.3.0 instrument. Three electrodes were placed on the test ear mastoid (inverting), forehead (ground) and vertex (non-inverting) such that each electrode and inter-electrode impedance was 1000 Ohms. Click stimulus had duration of 0.1 ms clicks was used as the test stimulus. The stimulus was delivered through insert earphone in rarefraction polarity at 90 dBnHL to record ABR in 15 msec. of post-stimulus time window and 5 msec. of pre-stimulus time window. Sweeps of 2000 click stimulus were presented at the repetition rate of 11.1/sec. Further, each epoch elicited was filtered online by 100 Hz to 3000 Hz. The epoch was rejected if the amplitude exceeded ± 23 μV. Finally epochs, which were free from artifacts, was averaged. The intensity was reduced till the lowest intensity level at which V peak was identified. In addition, tone burst 500 Hz stimulus was delivered through insert earphone in alternative polarity at 80 dBnHL to record ABR in 25 msec. of post-stimulus time window and 5 msec. of pre-stimulus time window. Sweeps of 2000 tone burst of 500 Hz were presented at the repetition rate of 11.1/sec. Further, each epoch elicited was filtered online by 100 Hz to 1500 Hz. The epoch was rejected if the amplitude exceeded ± 23 μV. The lowest intensity level at which V peak identified was noted.
A total of 572 ears were screened to check the hearing sensitivity. From high risk register it was observed that 212 ears had history of high risk to hearing impairment and remaining 360 ears had no risk. The hearing screening protocol comprised of three physiological tests that were administered on each test ear (TEOAE, 1 kHz tympanometry, broadband noise acoustic stapedial reflex with a 1 kHz probe tone). After screening protocol, in those ears that had obtained refer in any one among three tests and pass in all three tests was sent for detail audiological evaluation. The data obtained from infants screening were subjected to descriptive analysis. Besides, formulas were used to calculate the sensitivity, specificity, false positive and false negative responses from each test and combined physiological test. Diagnosis was sought from a pattern of results obtained from three physiological tests.
Pass and refer results from hearing screening protocol
Figure 1 shows pass and refer percentage result for individual and combined physiological tests. Of the 572 ears who underwent screening test in tympanometry, 99.3% (n=568) of them had passed, while 0.7% (n=4) of them had refer results. In TEOAE, 98.3% (n=562) of them had passed, while 1.7% (n=10) of them had refer results. However in ART for BBN, 96.9% (n=554) of them had passed, while 3.71% (n=18) of them had refer results. It revealed that higher pass percentage obtained from tympanometry, followed by TEOAE and then BBNART. However, highest refer percentage observed in BBN ART followed by TEOAE and then tympanometry. The combined physiological screening test revealed 96.2% (n=550) of them passed, while 3.8% (n=22) of them had refer results.
Diagnostic evaluation
The diagnostic evaluation was conducted on all 572 ears which includes the cases those who are referred and passed in the hearing screening test protocol. The referred and passed ears were sent for diagnostic evaluation for the purpose of detecting the true negative (Normal hearing sensitivity) and true positive (Pathology ear) results. Diagnostic evaluations included diagnostic ABR for click, immittance evaluation and TEOAE. If in any case, click ABR was absent then tone burst ABR for 500 Hz was carried out. Overall the result revealed that 97.7% (n=559) ears had normal hearing sensitivity and 2.3% (n=13) had pathology in their ears. ABR for click was absent in 10 ears. Further, result of tone burst ABR for 500 Hz revealed that in only one ear V peak was identified among those 10 individuals who had absent ABR for click stimulus. In three ears, ABR for click stimulus was present but at elevated threshold. Interestingly, in two ears of them found to have poorer morphology.
Sensitivity and specificity of physiological test: In diagnostic tests it revealed 13 [true positive (TP)] ears had pathology and 559 [true negative (TN)] ears had normal hearing sensitivity. False positive (FP) was identified from subtracting true positive result of diagnostic evaluation from that of referred cases in each physiological test. False negative (FN) was identified from subtracting true negative result of diagnostic evaluation from that of passed cases in each physiological test. The following formulas were utilized to obtain sensitivity, specificity, false positive and false negative results, respectively.
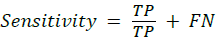
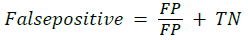
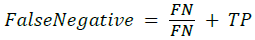
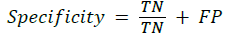
For example, in tympanometry, the test result showed 4 cases were referred of the 13 true positive response and negative response in 569 of the 559 true negatives. The sensitivity is 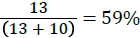 ; the specificity is
; the specificity is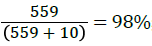 ;False positive is
;False positive is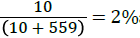 and false negative is
and false negative is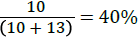 Similarly, sensitivity, specificity, false positive and false negative results were calculated for BBN ART, TEOAE and combined physiological tests (Table 2).
Similarly, sensitivity, specificity, false positive and false negative results were calculated for BBN ART, TEOAE and combined physiological tests (Table 2).
| Results | Tympanogram | BBNART | TEOAE | Combined physiological tests |
|---|---|---|---|---|
| Sensitivity (%) | 59 | 72 | 81 | 86 |
| Specificity (%) | 98 | 99 | 99 | 99 |
| False positive (%) | 2 | 1 | 1 | 0.3 |
| False Negative (%) | 4.1 | 2.8 | 1.9 | 1.3 |
Table 2: Sensitivity, specificity, false positive and false negative results of each test and Combine Physiologic Measure.
From Table 2, it is clear that BBN ART and OAE have more specificity in compared to tympanometry and combined PTs. However, false positive result was more in tympanometry and combined PTs compared to BBN ART and OAE. The sensitivity was more in OAE followed by BBN ART and then tympanogram and combined physiological tests, respectively. However, false negative result was more in tympanogram and combined physiological tests followed by BBN ART and then OAE.
Differentiate between the types of hearing loss from hearing screening tests: Table 3 gives the possible diagnostic significance based on the passed and referred results from hearing screening protocol. The screening protocol correctly identified normal hearing in 558 cases. In two cases at first instance OAE was referred. OAE was repeated once again and the result showed pass in two cases. The reflex for BBN was absent in three cases indicating either auditory neuropathy spectrum disorder (ANSD) or damage in efferent auditory pathway. This dilemma can only be solved by diagnostic evaluation. The result of ABR for click showed absent in one case indicated ANSD. In another two cases ABR for click was present but at the elevated threshold with poor morphology indicated probable damage in efferent auditory pathway.
| Tympanogram 1 KHz | BBN ART | OAE | Number of ears | Pathology site |
|---|---|---|---|---|
| P | P | P | 558 | No pathology |
| P | P | R* | 2 | |
| P | R | P | 3 | Auditory neuropathy |
| P | R | R | 5 | SNHL loss |
| P | P | R | 1 | ǂhigh frequency hearing loss |
| R | R | R | 4 | Conductive pathology ≠/ SNHL |
Table 3: Type of hearing loss information from the hearing screening protocol (*OAE repeated and the result showed pass, ǂABR for 500 Hz tone burst was present, ≠In one ear, ABR for click was present but at the elevated threshold).
In five cases BBN ART and OAE were referred indicate pathology in either sensory or neural hearing loss. On diagnostic evaluation it was revealed that on five ears ABR for click was absent. In yet another pattern, both tympanometry and reflex were passed but the OAE called for referral. Even in this case decision on site of pathology was difficult. On diagnostic testing, ABR for click stimulus was absent. However, ABR for 500 Hz tone burst was present till 50 dB nHL indicated high frequency hearing loss. In addition, it was noted that on four cases tympanometry, BBN ART and OAE were absent.
It is noted from Table 3 (last row) that the screening protocol cannot tell us either a sensorineural or conductive component is present in cases when all the three tests indicate a referral. On diagnostic evaluation it was confirmed that ABR for click was present in only one case but at the elevated threshold indicated as conductive pathology. In remaining three cases ABR for click and 500 Hz tone burst were absent indicate pathology in conductive and sensorineural pathway.
Tympanometry for 1 kHz probe tone frequency
In the present study 558 ears were passed in 1 kHz tympanometry and called for referral in 4 ears. However, the sensitivity of 1 kHz tympanometry is 59% and the specificity is 98%. The result of sensitivity is contrary to the previous studies by KC [21] and Harris [22], who reported sensitivity of 98.9% and 80%, respectively. This discrepancy is noted due to procedural variation. In their study the participants who are at risk and had failed in TEOAE and AABR were selected to evaluate the sensitivity of 1 kHz tympanometry. However, in the present study infants who are at risk and well babies were screened for hearing evaluation. The false negative response observed was 41%, that is, 9 cases were missed to indicate pathology by tympanometry. This is because these 9 cases have had pathology in other sites of auditory system but middle ear status was found to be normal in them. Hence, the false negative response was inflated. In addition, 2% of false positive response was noted, indicating pathology but they had normal hearing in them. The possible reason for it is collapsed canal. Other reason might be amniotic fluid accumulated in ear. The speculation was supported by the literature report MC Kenley [23] who reported false positive result in tympanometry using 1 kHz is most common due to vernix and residual mesenchyme, which are found to be a confounding factors to have failed in tympanometry screening. However after a few days to two weeks old, pass rates tend to be higher in newborns due to chance of clear ear canal and middle ear. Unfortunately in the present study one shot design was utilized. In present study tympanometry for 1 kHz was referred in four ears. Out of four ears in only one ear click ABR was present but at the elevated threshold indicate confirmed middle ear pathology. Whereas, in other three ears the ABR for click and tone burst for 500 Hz were absent suggestive of middle and sensory neural pathology.
Acoustic reflex threshold for broad band noise stimulus
In ART for BBN, 554 ears were passed and 18 ears were called for referral. The sensitivity of ART is 72% and the specificity is 99%. The result of specificity of present study is in accordance to the research report by Swanepoel DW [24] who successfully recorded ART from 94% of 143 healthy young infants aged 1 to 28 days using a 1 kHz probe tone and 1 kHz activator. However, the sensitivity of ART is contradictory to the previous study by Narne [25] who reported sensitivity of 88%. This is because they tested infants who had at risk for hearing impairment. Thus, the sensitivity was way high compared to our study. The false negative response observed was 28%, that is, 5 cases were missed to indicate pathology by ART. However, false positive response was 1% and the possible reason could be the presence of mesenchyme and immature neurological development. Absent ART alone cannot tell us the site of pathology. Thus, absent reflexes should be accompanied by diagnostic procedure to notify the probable site of pathology.
Otoacoustic emission
Of the 572 neonates who were screened, 562 (98.3%) yielded an OAE ‘Pass’ and 10 (1.7%) of them referred. The sensitivity of OAE is 81% and the specificity is 99%. The results of the present study is in contradictory to the research report of White, Behrens [26] who performed TEOAE screening on 1850 neonates and showed sensitivity of 100% and specificity of 73%. In present study, since the sensitivity is low the false negative response is higher which accounts to 19% (infants who have passed in OAE even though they have hearing loss). The reason could be OAE unable to detect the neural pathology. On diagnostic evaluation it was known that one of them have had suffered from auditory neuropathy and in other two ears indicated probable site of pathology in efferent pathway. The results of OAE infer that it is sensitive to both conductive and sensory pathologies, its absence cannot determine the type of hearing loss or pathology in auditory neural system. Interestingly, specificity is high and thus the false positive is low (infants who have failed in OAE even though they did not have any hearing loss). The reason for reduced false alarm in our OAE result is due to proper probe fit and test was conducted at quiet room. Kemp [27] suggested to record OAE in sound proof room or quiet environment. Contrary to previous study, Bantock and Croxson [28] who reported that sound roof room is not necessary to record OAE but the room should be quiet. In yet another study by Maxon [29], who suggested proper probe fit is almost necessary to reduce the false positive responses in infants.
Combined physiological tests
In two ears OAE was referred but the results of tympanogram and BBN for ART were passed. On analysing the referred result of OAE on two ears, it revealed noise floor was high. Thus, on same day after two hours of first evaluation OAE was administered. The result revealed passed OAE on two ears. Further, on five ears tympanometry result found referred but the results of ART for BBN and OAE were passed in them. If the middle ear pathology have present in all five cases then ART for BBN and OAE would have been absent in them. Interestingly, ART for BBN and OAE was present in all five ears thus it was not referred once gain for detailed audiological examination. The sensitivity of combined physiological test is 86% and the specificity is 99%. In three ears acoustic reflex were absent with passed results in tympanogram test and as well OAE test. This pattern of result leads to dilemma in deciding the site of pathology. Further on diagnostic evaluation, ABR was administered and results revealed no identifiable V peak was noted for either click or 500 Hz tone burst stimulus. It indicates the presence of auditory neuropathy spectrum disorder on these three infants. In yet another pattern, where tympanogram for 1 kHz was passed and other two tests (reflex and OAE) were referred. It suggests indicative of SNHL. The diagnosis was substantiated by the absent ABR for click and tone burst stimuli. It was also noted that OAE was absent in one ear, where tympanogram and reflex were absent. By looking at this pattern clinician can think of either ANSD or cochlear hearing loss. However, on administering diagnostic protocol it was revealed that ABR for click was absent and the tone burst ABR for 500 Hz was present till 40 dBnHL suggestive of high frequency hearing loss. Besides, another pattern was noted where all three tests were referred on four cases. In addition, ABR for click and tone burst ABR for 500 Hz stimuli were absent in all three cases indicate pathology in middle ear and in sensory neural pathway.
The screening protocol adopted in the current study assesses the peripheral and partly central auditory mechanism (lower brainstem structures). Peripheral auditory function can be accurately assessed by the results of tympanometry and otoacoustic emission. Auditory efferent and lower auditory brainstem mechanism was assessed by ART. Thus,the sensitivity of combined physiological tests targets 86% and the specificity is 99%. Use of this approach will reduce the number of false positive and also helps in suspecting neural disorders such as auditory neuropathy spectrum disorder. Depending on the results of these three measures, various diagnostic measures may be invoked that in turn may shed light on proper management strategies.