
Journal of Clinical Toxicology
Open Access
ISSN: 2161-0495

ISSN: 2161-0495
Case Report - (2022)Volume 12, Issue 3
Intentional overdose with either Calcium Channel Blockers or Angiotensin Receptor Blocker individually typically does not cause severe hemodynamic instability. However, a combined overdose with agents of both classes is known to increase the risk for hemodynamic instability, and may worsen the clinical course. We describe such an overdose, with detailed hemodynamic monitoring using thermodilution and pulse contour analysis tracking the clinical course. In addition, we wish to emphasize the scarce evidence supporting treatment strategies for overdose with this combination of drugs and the need for a patient-based decision-making process in such cases.
Thermodilution hemodynamic monitoring; Calcium Channel Blockers; Angiotensin Receptor Antagonists; Overdose; Shock
We present a case of a severe combined intoxication with a dihydropyridine Calcium Channel Blocker (CCB), and an Angiotensin Receptor Blocker (ARB), that was accompanied by co-ingestion of benzodiazepines. A thermodilution and pulse contour analysis-based monitoring system (PiCCO2, Pulsion, Munich, Germany) was used during the majority of the shock reversal phase of the treatment. This case illustrates the hemodynamic influence of the various treatments utilized during the shock reversal phase in this patient. This kind of monitors are able to provide various hemodynamic parameters based on the thermodilution studies for calibration of the system and later derived from analysis of the invasive pressure measurement waveforms. These monitoring devices also provide information on the volume status of the patient in a more exact way than classic, standard monitoring. “Standard” monitoring (either invasive or non-invasive blood pressure, pulse- rate and rhythm, oxygen saturation) gives only a partial glimpse of the hemodynamic status of the patient, derived from hemodynamic parameters such as preload, Systemic Vascular Resistance (SVR), cardiac contractility.
A 50 year old female patient with a past medical history of wellcontrolled hypothyroidism and glaucoma treated with an oral carbonic anhydrase inhibitor, was transferred to our Emergency Department (ED) by the Emergency Medical Services (EMS) following an intentional ingestion of 50 tablets of amlodipinevalsartan combination (total ingested doses-amlodipine 250 mg and valsartan 8 gr; this being 12.5 times, and 25 times the maximal recommended daily dose of each respectively). She also ingested 2.5 mg of brotizolam. Upon presentation to the ED the patient was severely hypotensive (blood pressure of 60/40 mmHg) and non-rousable. Intravenous (IV) Flumazenil 0.2 mg had only a transient effect on the level of consciousness. IV fluid resuscitation was commenced with 4,000 ml of 0.9% NaCl, followed by a high dose dopamine infusion (up to 15 mcg/kg/ min), with concomitant IV boluses of calcium chloride (total of 3 gr) and two IV boluses of terlipressin 1 mg. All the above interventions failed to restore adequate circulation and blood pressure.
Due to the depressed level of consciousness and ongoing hemodynamic instability, the patient underwent endotracheal intubation, followed by IV infusions of norepinephrine (up to 1.2 mcg/kg/min), epinephrine (up to 0.25 mcg/kg/min), and vasopressin (2 units per hour). Owing to severe metabolic acidosis (pH=7.199, Serum bicarbonate 17.7 mEq/l), 100 mEq of sodium bicarbonate was administered as an IV bolus. An IV bolus of glucagon 1 mg had a minimal effect on the hemodynamics. Following the above treatments, a Hyper-Insulinemic Euglycemic (HIE) regimen was administered as follows-IV bolus of 1 IU/kg of rapidly-acting insulin followed by an infusion of 0.5 IU/kg/hr. The patient was then transferred to the Intensive Care Unit (ICU) for further treatment and monitoring.
In the ICU the main stay of treatment included escalation of the HIE treatment (Figure 1A) and further administration of inotropes and vasopressors (Figure 1B). The patient was connected to a PiCCO2 monitor. An IV bolus of lipid emulsion (Lipofundin MCT/LCT 20%, B Braun Melsunen AG, Melsungen, Germany) 1.5 ml/kg was administered over 10 minutes, followed by an infusion of 1.5 ml/kg/hr over 1 hour. This also failed to demonstrate a beneficial clinical impact. Following the lipid emulsion infusion there was a mild increase in SVR, but without a concomitant increase in parameters of cardiac contractility as measured by PiCCO2, or an actual decrease of inotrope and/or vasopressor support requirements. An IV dose of methylene blue of 2 mg/kg also failed to increase SVR or affect blood pressure.
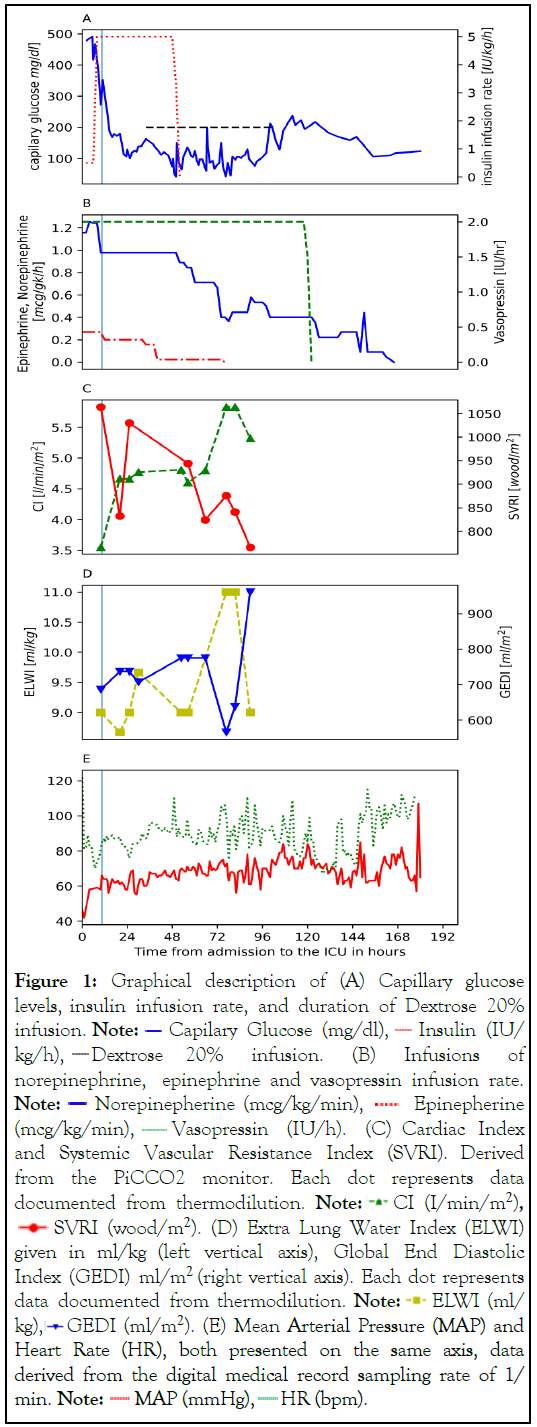
Figure 1: Graphical description of (A) Capillary glucose
levels, insulin infusion rate, and duration of Dextrose 20%
infusion. Note:  Capilary Glucose (mg/dl),
Capilary Glucose (mg/dl),  Insulin (IU/
kg/h),
Insulin (IU/
kg/h),  Dextrose 20% infusion. (B) Infusions of
norepinephrine, epinephrine and vasopressin infusion rate. Note:
Dextrose 20% infusion. (B) Infusions of
norepinephrine, epinephrine and vasopressin infusion rate. Note:  Norepinepherine (mcg/kg/min),
Norepinepherine (mcg/kg/min),  Epinepherine
(mcg/kg/min),
Epinepherine
(mcg/kg/min),  Vasopressin (IU/h). (C) Cardiac Index
and Systemic Vascular Resistance Index (SVRI). Derived
from the PiCCO2 monitor. Each dot represents data
documented from thermodilution. Note:
Vasopressin (IU/h). (C) Cardiac Index
and Systemic Vascular Resistance Index (SVRI). Derived
from the PiCCO2 monitor. Each dot represents data
documented from thermodilution. Note:  CI (I/min/m2),
CI (I/min/m2),  SVRI (wood/m2). (D) Extra Lung Water Index (ELWI)
given in ml/kg (left vertical axis), Global End Diastolic
Index (GEDI) ml/m2 (right vertical axis). Each dot represents
data documented from thermodilution. Note:
SVRI (wood/m2). (D) Extra Lung Water Index (ELWI)
given in ml/kg (left vertical axis), Global End Diastolic
Index (GEDI) ml/m2 (right vertical axis). Each dot represents
data documented from thermodilution. Note:  ELWI (ml/
kg),
ELWI (ml/
kg),  GEDI (ml/m2). (E) Mean Arterial Pressure (MAP) and
Heart Rate (HR), both presented on the same axis, data
derived from the digital medical record sampling rate of 1/
min. Note:
GEDI (ml/m2). (E) Mean Arterial Pressure (MAP) and
Heart Rate (HR), both presented on the same axis, data
derived from the digital medical record sampling rate of 1/
min. Note:  MAP (mmHg),
MAP (mmHg),  HR (bpm).
HR (bpm).
Following the first 24 hours of HIE the blood glucose levels decreased significantly, to the range of 100-200 mg/dl (from initial values ranging between 400-500 mg/dl). In response, we administered an IV dextrose 20% infusion in combination with the HIE (Figure 1A). On the third day of the ICU admission the insulin infusion was discontinued, however, an IV dextrose infusion was continued to maintain euglycemia. The dextrose 20% infusion was indicated until the fourth day of ICU stay.
On the fourth day in the ICU the patient developed tense ascites and bilateral pleural effusions. These collections were drained percutaneously, yielding 4 liters of ascitic fluid (with SAAG<1.1) and about 750 ml of transudative fluid from each pleural cavity. The serum albumin levels during the ICU stay were 30 g/dl at the nadir, and serum sodium levels were within normal limits. All bacterial cultures taken from the drained fluids were negative. Following diuresis with furosemide, the fluid collections did not recur (Figures 1A-1E).
(A) Capillary glucose levels–solid blue line (left vertical axis, reported in mg/dl), insulin infusion rate-dotted red line (right vertical axis, reported in IU/kg/hr), and duration of Dextrose 20% infusion–black dashed line, rates are not reported. (B) Infusions of both norepinephrine solid blue line, and epinephrine interrupted red line are given in mcg/kg/min (left vertical axis). Vasopressin dashed green line infusion rate reported in IU/hr (right vertical axis). (C) Cardiac Index (CI) full green triangles connected by interrupted line given in l/min/m2 (left vertical axis) and Systemic Vascular Resistance Index (SVRI) wood/m2 (right vertical axis) and it is derived from the PiCCO2 monitor. Each dot represents data documented from thermodilution. (D) Extra Lung Water Index (ELWI) given in ml/kg (left vertical axis), Global End Diastolic Index (GEDI) ml/m2 (right vertical axis). Each dot represent data documented from thermodilution (E) Mean Arterial Pressure (MAP) is given in mmHg and Heart Rate (HR) is given in Beats Per Minute (BPM), both presented on the same axis, data derived from the digital medical record sampling rate of 1/ min. In all of the panels a teal solid vertical line indicates administration of intravenous lipid emulsion at 10 hours after admission to the IUC.
During her stay in the ICU advanced hemodynamic monitoring demonstrated ongoing low SVR. The lowest documented Cardiac Index (CI) was 3.55 L/min/m2 at the beginning of the clinical course. Later, the CI recovered (Figure 1C). However, these readings were obtained under significant inotropic support-HIE and epinephrine infusions (Figures 1A and 1B).
Regarding circulating and extravascular fluid status, the patient had both high Global End Diastolic Index (GEDI)-an estimator of the preload in all four cardiac chambers, and Extra Lung Water Index (ELWI)-a metric representing the amount of interstitial fluid in the lungs, throughout the resuscitation phase (Figure 1D). Of note, PiCCO2 monitoring was initiated only 10 hours following admission to the ICU and 16 hours following the intoxication. So, unfortunately, the initial phases of the resuscitation were not analyzed by this monitoring modality.
On the eighth day of ICU stay, the patient underwent successful tracheal extubation. After nine days in the ICU, the patient was discharged for ongoing treatment in a medical ward. There the patient suffered sudden onset of arterial hypoxemia, dyspnea, and pleuritic chest pain. A chest X-ray demonstrated a new pneumothorax and a pig-tail intercostal drain was inserted. After excluding other possible causes, a diagnosis of spontaneous pneumothorax was made. The pneumothorax resolved within 3 days and the drain removed uneventfully. There was a KIDIGO stage 1 acute kidney injury (serum creatinine increase from admission base line of 86 mmol/l to a maximal value of 116 mmol/l during the first day of ICU stay), which rapidly resolved with later improvement of hemodynamics. Urinary output was preserved throughout the stay in the ICU. The patient was subsequently transferred to the Psychiatric Ward from where she was discharged home in good condition.
We present a case report of severe co-ingestion of an ARB and a dihydropyridine CCB which resulted in a severe prolonged shock, refractory to all vasopressors and inotropes, responsive only to HIE. The patient was monitored using a PiCCO2 monitor within several hours after the initial presentation. The main findings during the resuscitation phase were of volume overload and severe vasoplegia, with preserved Cardiac Indexunder significant inotropic and vasopressor support with coadministration of HIE (Figure 1A). Administration of HIE had a beneficial effect on the vasopressor requirements and on hemodynamics, while both lipid emulsion therapy and methylene blue had a negligible effect (Figure 1, timing of lipid emulsion infusion administration is noted by a teal vertical line on all panels). A further interpretation of the clinical data may indicate a combined mechanism of shock, both vasodilatory and cardiogenic. Without accurate and invasive hemodynamic monitoring, this distinction would not have been possible.
There are several added benefits to utilization of advanced hemodynamic monitoring in complex cases such as the one being presented. Firstly, it allowed us to differentiate the mechanism of shock, or more accurately, to assess the severity of each component of the shock. As dihydropyridine CCB’s ingested at high dose lose their selectivity to peripheral L-type calcium channels, and they cause a cardioplegic effect. In such a scenario administration of vasopressor alone may be detrimental. Secondly, its use as a continuous monitoring device (pulse contour analysis) with recurrent calibration (thermodilution based study) enables the clinician to assess in depth the effect of various treatments, in the specific patient. For example, this device demonstrated the lack of beneficial effect to administration of both lipid emulsion and methylene blue. Lastly, would be the ability of such a device to demonstrate hemodynamic parameters which remain concealed when using clinical judgement or standard monitoring alone.
Both ARB’s and Angiotensin Converting Enzyme Inhibitors (ACEI) have well-described side effects predicted by their mechanism of action. Acute ARB’s toxicity, in isolated ingestion, not exceeding five times the maximum daily dose, is usually of mild presentation [1]. Having said that, a retrospective review demonstrated that a combined intoxication by dihydropyridine CCB and ACEI/ARB’s causes a more severe hemodynamic compromise than isolated dihydropyridine CCB intoxication. A synergistic effect caused by the combination of the drug types, both prolongs the duration and increases the severity of hypotension [2]. This study’s main hemodynamic outcomes were both systolic (SBP) and Mean Arterial Pressures (MAP), while we noted several additional aspects of the hemodynamic collapse secondary to the co-ingestion as shown in the figures above. Moreover, the study population of the review represented a mixed group of patients, with variable degrees of hemodynamic compromise and level of support required [2]. Our case describes a patient in deep shock and represents a much worse response to the combined overdose and therefore can provide insights into the significant hemodynamic support such patients may require.
The current recommendations regarding treatment of severe CCB poisoning favor administration of the following treatments: IV Calcium, HIE if myocardial dysfunction is evident, and norepinephrine/epinephrine as required [3]. In case this first line of treatment fails, incrementing the insulin dose up to 10 IU/kg/hr and lipid therapy are recommended [3,4]. With further worsening, Veno-Arterial Extra Corporeal Membrane Oxygenation (VA-ECMO) and/or cardiac pacing should be considered based on the clinical status of the patient [3,5]. In the case of cardiac arrest, administrations of IV calcium and lipid therapy are recommended as well as extracorporeal resuscitation and adherence to the Advanced Cardiac Life Support (ACLS) guidelines.
HIE has gradually became a cornerstone of resuscitation in patients in deep shock secondary to ingestion of CCB [4]. This treatment has been proven to be beneficial in animal models and later in the clinical setting. A bolus of 1 IU/kg of insulin is followed by a continuous infusion. Over time recommended infusion rates gradually increased from 0.5-1 IU/kg/hr, to rates as high as 1-10 IU/kg/hr. The optimal rate is yet to be found. HIE was proven to be superior to calcium infusion, glucagon administration and vasopressor/inotropes when these agents were given alone.
Insulin’s beneficial effect is mediated through three main mechanisms: 1. Positive inotropic effect; 2. Increase in the intracellular glucose levels; and 3. Vasodilation-this effect is particularly beneficial in cases of cardiogenic shock. The main possible detrimental effects of HIE are hypoglycemia and hypokalemia. Therefore, co-administration of glucose under tight monitoring of both serum glucose and electrolytes is indicated [4].
The Extracorporeal Treatment in Poisoning (EXTRIP) workgroup has published a systemic review recommending against utilization of extra corporal support (dialysis, liver replacement devices etc.) for treatment of CCB namely amlodipine, verapamil, and diltiazem-overdose [6]. Yet, utilization of Molecular Adsorbent Recirculating System (MARS) in severe intoxications is reported as a beneficial intervention in some case reports/series [7-9] treating both dihydropyridine and non-dihydropyridine CCB severe toxicity. The beneficial effect is partially explained by amlodipine being a highly protein bound substance; therefore its elimination halflife could be enhanced by the albumin dialysis utilized in MARS. However, there are no randomized controlled trials supporting its use in cases of severe CCB toxicity. We should bear in mind that this is a very invasive, expensive, and complex modality of therapy with a well-described profile of adverse events, which requires a high degree of specialization by the treating team to provide it effectively. VA-ECMO support has been reported to be beneficial in case reports [10,11] as well as in a review and is depicted in expert opinions as a last resort option for patients in cardiac arrest or severe refractory cardiogenic shock [3].
Another possible line of treatment in cases of refractory shock may be infusion of angiotensin-II. This drug has been found to be beneficial in the setting of refractory vasodilatory shock [12]. A later subgroup analysis revealed a sub-population of patients with relative angiotensin deficiency that may benefit from the drug’s administration [13]. A recent systemic review demonstrated potential beneficial effects of angiotensin-II administration in intoxication induced shock [14]. Though the quality of evidence in the review is low (case reports, without randomized trials) a positive hemodynamic response in the terms of MAP and SBP has been seen.
Treating a severe combined intoxication is a challenging clinical task for several reasons. There might be deleterious synergistic effects between the drugs ingested, causing significant alteration in the clinical course of the patient or the severity of presentation as seen in our case. As the evidence is scarce and of lower quality, it is difficult to plot an optimal treatment based on the literature alone. Application of advanced hemodynamic monitoring tools may allow a more precise diagnosis of the shock mechanism and therefore allow more appropriate support in the critical phase of the patient’s course.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Firman S, Batzofin BM, van Heerden PV, Nachshon A (2022) Severe Amlodipine and Valsartan Overdose: A Case Report Describing the Utilization of Thermodilution and Pulse Contour-Based Hemodynamic Assessment. J Clin Toxicol. 12:511.
Received: 30-May-2022, Manuscript No. JCT-22-17682; Editor assigned: 01-Jun-2022, Pre QC No. JCT-22-17682 (PQ); Reviewed: 15-Jun-2022, QC No. JCT-22-17682; Revised: 22-Jun-2022, Manuscript No. JCT-22-17682 (R) ; Published: 29-Jun-2022 , DOI: 10.35248/2161-0495.22.12.511
Copyright: © 2022 Firman S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.