Emergency Medicine: Open Access
Open Access
ISSN: 2165-7548
ISSN: 2165-7548
Case Report - (2018) Volume 8, Issue 1
Baking Soda is a universally available household product. It is used to treat heartburn, indigestion as a home remedy. It's generally well tolerated but abuse and overdose can cause toxicities with serious metabolic and neurological complications. We discuss here a case of a patient with acute baking soda toxicity that developed acute respiratory failure and large bilateral cerebral infarctions leading to death. To our research this is the first reported case of cerebral infarctions following baking soda toxicity. Our report underlines the need for healthcare professionals to be aware on the complications of baking soda overdose and its urgent treatment.
Keywords: Baking soda; Hypernatremia; Metabolic alkalosis; Cerebral infarction
Baking Soda (Sodium Bicarbonate) is a salt composed of sodium and bicarbonate ions [1,2]. It is a widely available household product used for cooking, baking, personal care and cleaning purposes [3]. It has long been used also as a home remedy for heartburn and indigestion, and also misused as an agent to “beat a urine drug test” and to treat urinary infections [4]. In clinical medicine it’s used to treat severe metabolic acidosis, hyperkalemia, dysrhythmias, tricyclics and diphenhydramine overdose [1,5]. In smaller recommended doses it’s generally well tolerated [1] but excessive ingestion can cause serious metabolic and neurological complications [6-9]. Despite its widespread use severe toxicity and fatality from baking soda overdose is very rarely reported in medical literature [6,9]. We report here a case of a patient who presented with severe metabolic alkalosis, severe hypernatremia, acute respiratory failure and Ischemic stroke after large volume baking soda ingestion. To our research this is the first documented case of ischemic stroke that developed after Sodium Bicarbonate overdose.
70 years old Female, an adult home resident, with history of Diabetes, hypertension, Anxiety, Depression and Non-Hodgkin’s Lymphoma in remission was brought to Emergency room with altered mental status. Patient was discharged from hospital two days ago after she was treated for dizziness and fall. Syncope workup including Echo, CT scan of the head (Figure 1). Carotid Doppler, and ECG done in that hospital stay were all normal. At presentation in the ED Patient was lethargic. Her Vitals were temperature 96, Pulse rate 104, and Respirations 18/minute blood pressure 142/66 mm of Hg and Oxygen saturation 95%. On physical examination patient was unresponsive to verbal or noxious stimuli, had moist mucous membrane, and decreased air entry on both lungs. She was tachycardia but had no murmurs or gallop rhythms. Her pupils were midsized and reactive on both sides.
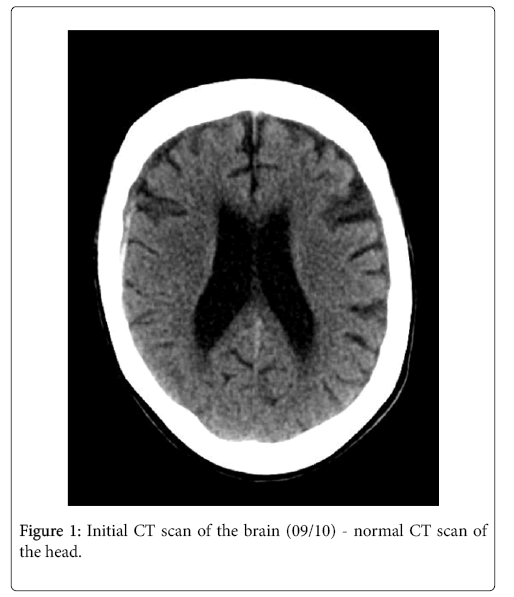
Figure 1: Initial CT scan of the brain (09/10) - normal CT scan of the head.
There was no neck stiffness. Relevant laboratory values at presentation were Serum Na+ 169; K+ 2.8; Cl- 99; HC03- 59, BUN 30; Creatinine 0.81; Ca+2 11.3, Glucose 409; Hematocrit 41.3; Arterial blood gas with 3 oxygen showed pH of 7.550; CO2 63.9; PO2 249; base excess of - 29.6; Urine pH was 8.5. Urine Na+ 176, and Urine Creatinine 15.5 and Fractional Excretion of Sodium (FeNa) was 5.4% (Tables 1-3).
| Serum Electrolyte | 09-09-17/23:27 | 09-09-17/23:27 | 09-10-17/3:04 |
| Sodium | 169 H* ICI | 165 H* | |
| Potassium | 2.8 L* CI | 3.1 LC | |
| Chloride | 99 (;) | 107 5 | |
| Carbon Dioxide | 59 HQ | 46 HQ | |
| BUN | 30.0 H CP | 30.0 H V | |
| Creatinine | 0.81 CP | 0.78 c) | |
| Glucose | 409 H c) | 465 H* ICI | |
| POC Glucose | |||
| Whole Bid Lactic Acid | 2.7 H la | ||
| Calcium | 10.9 H Ci | ||
| Phosphorus Magnesium | |||
| Iron | |||
| TIBC | |||
| Ferritin | |||
| Total Bilirubin | 0.5 CI | 0.6 CI | |
| AST | 40 H | 38 H C) | |
| ALT | 42 CI | 39 CI | |
| Alkaline Phosphatase | 120 CI | 118 CI | |
| Total Creatine Klnase | |||
| CK-MB (CK-2) | |||
| CK-MB (CK-2) % | |||
| Troponin I Ultra-Sens | |||
| Total Protein | 6.3 CI | 5.9 L CI | |
| Albumin | 3.7 C) | 3.5 Ca | |
| EGFR Interpretation | 69.90 CI | 73.01 CI | |
| Vitamin 612 | |||
| Folate |
Table 1: Serum electrolytes at presentation.
| Arterial blood values | 09-09-17 | 09-10-17 | 09-11-17 | 09-12-17 | 09/13/17 |
| 11:44:00 PM | 3:10:00 AM | 10:10:00 AM | 8:15 | 0.361111111 | |
| MG pH | 7.550 H S 7.666 H e | 7.510 H Si | 7.532 H Si 7.457 H S 7.428 S | ||
| ABG pCO2 | 63.9 H M 39.3 CD | 56.7 H CD | 39.5 CD 37.5 CD 33.0 5 | ||
| AUG p02 | 249.0 H S 250.0 H ci | 140.0 H S | 309.0 H S | 199.0 1-1 0 | 182.0 H a |
| MG HCO3 | 53.5 H 45.9 H | 42.9 H | 33.4 H | 26.8 | 22.6 |
| ABG 02 Saturation | 99.7 H S 99.9 H S | 98.9 S | 99.7 II Si | 99.3 H S | 99.4 H Si |
| ABG Base Excess | 29.6 H 21.6 H | 19.9 H | 9.6 H | 2.5 H | -2.3 |
| Blood Gas Modality | NC CD PRVC CD | 8/400/35/5 | CD vent S | vent CD | vent CD |
| F102 | 3 litres S 50 Si | 35 S | 60 S | 40 S | 40 S |
Table 2: Arterial blood gas values.
| NIPIWI | 09/10/17 09/10/17 09/10/17 09/10/17 09/10/1 | 09/14/17 | ||||
| 0:00 | 1:30 | 1:30 | 16:00 | 16:00 e | 10:50 | |
| Urine Color | Yellow s | Cancelled | Yellow s | |||
| Urine Clarity | clear e | cloudy a s | ||||
| Urine pH | 8.5 h a | 6.0 e | ||||
| Ur Specific Gravity | 1.015 ci | 1.020 la | ||||
| Urine Protein | 30 h s | Negative s | ||||
| Urine Glucose (UA) | 500 h s | >-1000 h q | ||||
| Urine Ketones | trace h e | Negative cl | ||||
| Urine Blood | negative e | moderate a ci | ||||
| Urine Nitrite | negative e | Negative ci | ||||
| Urine Bllirubin | negative s | Negative s | ||||
| Urine Urobilinogen | 1.0 s | 0.2 e | ||||
| Ur Leukocyte Esterase | negative e | Large a la | ||||
| Urine RBC | 0.2 / hpf | 20.50 / hpf h | ||||
| Urine WBC | 2 to 5 | 20-50 | ||||
| Urine WBC Clumps | occasional | Few clumps seen | ||||
| Ur Squamous Epith Cells | trace | Small | ||||
| Urine Bacteria | Small | |||||
| Urine Mucus | Numerous | |||||
| Urine Yeast | ||||||
| Ur Random Sodium | 176 H S 63 e | |||||
| Ur Random Potassium | 30.2 (;) 117.2 S | |||||
| Urine Myogiobin | 15.5 S | |||||
| Urine Creatinine | 87.7 S | |||||
Table 3: Urinalysis and urine electrolytes.
ECG showed sinus tachycardia; Urine toxicology screen was positive for benzodiazepines and negative for Opiates, amphetamines, salicylates and acetaminophen. CT of the head was with no acute findings.
A friend of the patient reported that the patient was taking Baking Soda for Hammer© Baking Soda was found in her room. Patient started to have worsening of respiratory status with diminished respiratory effort and absent air entry with hypoxemia (oxygen saturation 70%), and she was put on mechanical ventilation (Figure 2).
The Patient was transferred to ICU, started on IV Crystalloids with Normal saline and potassium replacement. Patient started to have frequent generalized tonic clonic seizures which were controlled with high doses of Levetiracetam and Lorazepam. Patient’s metabolic and electrolyte abnormalities were corrected gradually. After 72 hours on IV normal saline and electrolyte replacement her serum pH came down from 7.550 to a normal range of 7.428 and her serum Na+ also lowered from 169 on admission to 153. Her WBC was high starting from admission but she started to develop fever after 48 hrs in ICU, blood culture was negative but urine and endotracheal aspirate showed Candida Albicans. She was treated with broad spectrum antibiotics and Fluonazole. Her hemoglobin and hematocrit dropped from 14.1/44.7% on admission to 7.8/27.1 three days later. There was no gross bleeding in the rectum or any blood coming out through NGT (nasogastric tube), but her fecal occult blood was positive. She was transfused with 2 units of PRBC (Packed red blood cell). Patient was managed by multispecialty team involving Pulmonary/Critical care, Nephrology, Neurology, Endocrine, GI, Hematology and Infectious disease. Despite improvements in metabolic and electrolyte profile patient remained unresponsive and ventilator dependent. Follow up CT scan of the brain done 2 days after admission showed “Interval development of acute bilateral MCA distribution infarcts”; another follow up CT after 24 hours was consistent with the findings. MRI of the brain was not obtained due to patient’s condition and lack of ventilator compatible MRI.
Despite aggressive medical therapy patient’s condition deteriorated with absent brain stem reflexes and dilated and sluggish pupillary reflex. Palliative care was consulted and discussed with family about goals of care. As per patient’s previously stated wish, family opted for ventilator liberation and comfort care. Patient was extubated 11 days after admission and passed away 3 days later from respiratory failure.
Baking soda products contain 59 mEq sodium and bicarbonate per teaspoonful [4]. The short-term administration of large amounts of sodium bicarbonate to normal individuals usually results in very rapid renal excretion of the entire alkali load with minimal increase in the bicarbonate concentration [10,11]. Adults with normal renal function can tolerate up to 1700 mEq daily with minimal symptoms [2]. Excretion of sodium bicarbonate may be impaired if there is renal insufficiency, hypokalemia, hypochloremia or volume contraction [11-13].
Toxic effect of sodium bicarbonate is secondary to the hypernatremia from high sodium load and metabolic alkalosis (MA) from the bicarbonate ions. Severe MA is associated with very high mortality, up to 80% if pH is >7.65 [8,13]. Our patient had a pH of 7.66. Neuronal excitability due to disturbed calcium metabolism, increased release of acetylcholine at NM junction and redistribution hypokalemia can present as tetany and seizure when pH is >7.5. Reduced cerebral blood flow, cerebral vasoconstriction and CSF alkalosis has also been observed [8,13,14]. Myocardial irritability can lead to supraventricular and ventricular arrhythmias [4,9,15]. Respiratory failure is caused by compensatory hypoventilation, decreased tissue oxygen delivery from a left shift of oxygen dissociation curve (Bohr effect), and decreased sensitivity of peripheral chemoreceptors to hypoxia [16-18]. Acute severe hypernatremia from salt ingestion presents with seizures, coma, hypertonia, fevers, hemorrhagic infarctions and thrombosis of dural sinuses [6,19,20].
Vascular injury created by a suddenly shrinking brain causes intracranial hemorrhage [6]. Excessive sodium bicarbonate may also cause congestive heart failure exacerbation and pulmonary edema [1]. Other metabolic and clinical effects from baking soda ingestion include hypertension, gastric rupture, rhabdomyolysis hyporeninemia, hypokalemia, hypochloremia, intravascular volume depletion, and urinary alkalinization [1,6,7,9,21,22].
Our patient presented with acute severe metabolic alkalosis, severe hypernatremia, hypokalemia, high urine pH, compensatory hypoventilation and coma. Subsequently the patient developed bilateral middle cerebral artery distribution ischemic strokes. Even though hemorrhagic encephalopathy [6] and hypoxic encephalopathy [9] have been reported in the past this is the 1st time an ischemic stroke is documented following ingestion of baking soda. It may be explained by cerebral vasoconstriction, the decreased cerebral blood flow due to metabolic alkalosis [8,13,14], tissue hypoxia [16-18] and hypernatremia associated neuronal injury [6,19].
Patients with baking soda overdose can present with mild to severe symptoms depending on the amount and duration of ingestion [1,4,6,9,19]. Patients commonly present with abdominal symptoms like nausea and vomiting and in few severe cases can present with neurological symptoms like change in mental status, seizures, coma and even cardiopulmonary arrest [4,6,9]. Abdominal distention and possible damage or rupture of the stomach can also occur from carbon dioxide release when large amount of baking soda is ingested [23].
Initial work up must include CBC, complete metabolic panel, arterial blood gas study and EKG. Urine pH, Urine Osmolarity and urine electrolytes are also important [1,6-9]. Fractional excretions of sodium (FeNa) >2% in children is consistent with acute salt ingestion (poisoning) [24]. Our patient had FeNa of 5.4%.
Patients with neurological symptoms like seizures and change in mental status need CT scan of the Brain and EEG [6,9]. Because of the risk of arrhythmia and neurologic complications patients with severe signs and symptoms will need continuous cardiac monitoring frequent neuro checks in ICU setting [1].
Patients who present with hypernatremia and alkalosis must be suspected for sodium bicarbonate overdose [6,7,9,12]. Therapy should be aimed at early correction of electrolyte abnormalities and volume resuscitation with chloride and K containing IV solutions [1,19,25,26].
Hypochloremia and hypokalemia worsen metabolic alkalosis by increasing renal reabsorption of bicarbonate and should be corrected immediately [11,13,27]. I.V fluids with 0.9 % normal saline or 0.45% Normal saline with KCL can be used. The serum sodium should be lowered rapidly to a near-normal level in less than 24 hours [13,18]. Because of the time required for the cerebral adaption, only patients with hypernatremia for at least 48 hours are at risk for overly rapid correction. Patients with Sodium Bicarbonate toxicity may develop severe symptoms of hypernatremia but are not likely to be at risk from overly rapid correction [13,18]. If renal function is severely depressed or if intractable CHF and hyperkalemia present, precluding the use of Na and K, peritoneal or hemodialysis with low bicarbonate dialysate may be indicated to correct metabolic alkalosis [8,13].
In patients with very severe alkalemia (pH greater than 7.55, or severe symptoms of toxicity) not responding to conventional treatment, therapy with ammonium chloride or dilute HCl may be considered [1,13]. Severe metabolic alkalosis could be safely corrected to a pH of 7.45 within six to 12 hrs using 0.25 N (250 meq/L) of HCL at a rate of 100 ml/hr in central venous catheter. The dose and rate of HCL administration depends on the weight, chloride deficit and base excess of the patient [9,28]. Hypoxemia and tissue hypoxia can be corrected by administering high flow oxygen. Assisted ventilation with correction of the PCO2 to normal should be avoided, as this will acutely raise the arterial pH and may lead to deepening coma, seizures and tetany [9,17].
In our patient Electrolyte abnormalities were only corrected gradually over 48-72 hours despite early IV fluid hydration with 0.45 % NaCl and K replacement. Metabolic alkalosis may have been worsened by mechanical ventilation that has offset the respiratory compensation. Patient could also have benefited from IV Hydrochloric acid.
Our case highlights a severe toxicity from baking soda that lead to severe hypernatremia, severe metabolic alkalosis, acute respiratory failure, and acute cerebral ischemic stroke that resulted in fatality. Emergency physicians and health care providers should be aware of the potential misuse and toxicity from baking soda and also be well versed in the management of severe toxicity as early intervention can improve outcome.