
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Research Article - (2020)Volume 11, Issue 6
Background: “Short Neck” is a term used by anesthesiologists and emergency physicians to describe one of the risk factors of difficult airway management; but there is no consensus on what length constitutes short neck.
Study objective: To measure neck length and associate it with intubation difficulty in obese patients, the secondary objective to find any relationship between short neck, difficult intubation and increasing body mass index.
Design: A pilot, cross sectional prospective single blinded study.
Sample: 97 adult patients scheduled for elective surgery, in Hamad General Hospital between March 2018 and October 2018, under general anesthesia, was recruited for the study.
Results: Airway assessment using anthropometric measurements, including neck length, were documented prior to anesthesia. Operators (anesthesiologists) were blinded. Intubation Difficult Scale was used. All data were documented and analyzed afterwards. Patients were of three groups according to Intubation Difficulty Scale (IDS): Group A: IDS 0, Group B: IDS>0 - ≤ 5 and Group C: IDS>5. Five patients (5.2%) with intubation difficulty score>5 have a mean neck length 7.6 cm. “Short Neck” was found to have a significant p value 0.022 within the three groups.
Conclusions: A patient's features relevant to airway assessment are rather difficult to quantify. This is the first reported attempt to obtain an objective value for Short Neck in routine airway assessment.
Short neck; Airway assessment
The term commonly used by physicians caring for patients in acute care areas, when assessing patient’s airway is “Short Neck”, which indicates the possibility of difficult airway and certainly would influence the management. Most of the airway management guidelines [1,2], audits [3], books, and articles [4-9] refer to this term as a criterion. Unfortunately, the term Short Neck is very subjective and none of these references addressed the term in a methodical approach. Some medical and nonmedical specialties have tried to define Short Neck in their own way, but there is no consensus on neck length measurement, and none have been standardized [10-13].
According to the medical definition of “neck”, it is the “part of the body where the head is connected to the trunk; it extends from the base of the cranium to the top of the shoulders” or it is “the usually narrowed part of an animal that connects the head with the body; specifically: the cervical region of a vertebrate” [see Dictionary 1,2]. Gray’s anatomy describes the neck as the part that “extends from the base of the cranium and the inferior border of the mandible to the thoracic inlet” [14].
On the other hand, Short Neck was defined by the National Human Genome Research Institute as “decreased distance from the point where neck and shoulders meet to the inferior margin of the occipital bone ” [15]. This lack of clarity surrounding Short Neck despite its relevance in airway management raised many questions, such as: How do we define a Short Neck? How does Short Neck affect airway management? This motivated us to perform a literature review on the subject in search for answers.
Our main objective is to measure Short Neck with a special reference to obese patients, i.e. to identify the threshold length of the neck below which most patients would be difficult to intubate. Our secondary objective was to identify any association between Short Neck, difficult airway and increasing BMI.
This was a pilot prospective single blinded study. Following the approval of the Medical Research Centre (MRC) and the Institutional Review Board (IRB) of Hamad Medical Corporation, obese adult patients of both genders scheduled for elective surgery at Hamad General Hospital between March 2018 and October 2018, with Body Mass Index (BMI)>30 kg/sq. m, were prospectively identified and recruited. Exclusion criteria were any patients with congenital anomalies, thyroid nodule, tumor of the neck and face or cervical injury/limitation of movement, as these features may cause Short Neck or interfere with measurement and overall assessment or intubation.
Standard airway assessment parameters were considered including: Mouth Opening (MO); Thyromental Distance (TMD); Mallampati Score (MMP); Neck Circumference (NC) at the cricoid level; Prognathism (PRO) for under or overbite; Dentition (Full, Loose and Edentulous); and Neck Length (NL).
The procedure was explained to the patient and their consent was obtained. A measuring tape was used to determine MO, TMD, NC and NL, while other variables (MMP, PRO and dentition) were visually observed. This data was then documented on a data sheet.
The NL was measured after the patients held their head in a neutral position. This neutral position was assumed by asking the patient to look forward and hold their head in a position that they felt was most comfortable. NL, specifically, was assessed by measuring the distance between the tip of the Mastoid, as it aligns with the level of the First Cervical vertebrae (Atlas) [16], to the meeting point between the neck and the shoulder (inflection point). We call this the “apparent neck” (Figure 1).
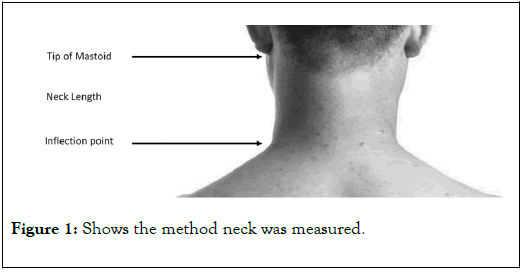
Figure 1. Shows the method neck was measured.
Data on demographics such as age, gender, height, weight, and Body Mass Index (BMI), were also collected. The study participants were intubated only by senior anesthesiologists (operator) who were blinded to the study. The operators were then given an intubation difficulty scale (IDS) sheet to fill out [17]. None of the investigators were involved in the intubation procedure. The IDS score was calculated by the investigators and along with the other data collected was entered in a coded Microsoft Excel spreadsheet for further statistical analysis.
Statistical analysis
The primary objective of the data analysis in this pilot study was to assess and quantify the significance of neck length in the airway assessment. The statistical analysis was categorical and continuous values were expressed as frequency (percentage), mean ± SD or median, and interquartile range (IQR) as appropriate. Descriptive statistics were used to summarize demographic traits, clinical measures, parameters related to airway assessment, laboratory, and other related parameters. The Kolmogorov-Smirnov (K-S) test or Q-Q Plot, as appropriate, were then used to test for normality of the data.
Associations between two or more qualitative variables will be assessed using chi-square (χ2) test and/or Fisher Exact test, as appropriate. Quantitative data between two and more than two independent groups will be analyzed using an unpaired ‘t’ test and one-way analysis of variance (ANOVA). Where an overall group difference was found to be statistically significant, pairwise comparisons were made using the appropriate post-hoc test. Relationships between two quantitative variables were examined using Pearson’s correlation coefficients.
In addition, appropriate univariate, and multivariate regression analysis (linear or logistic regression methods) were used to assess and quantify the effect of different factors and parameters, such as neck length, neck circumference, and age group etc. on the outcome of the variable difficult airway assessments. The results were presented with the associated 95% confidence interval. Visual presentations of the key results were made using appropriate statistical graphs. All p values presented were twotailed, and p values<0.05 are considered as statistically significant. All statistical analyses were done using statistical packages SPSS 22.0 (SPSS Inc. Chicago, IL) and Epi-info (Centers for Disease Control and Prevention, Atlanta, GA) software.
99 patients were initially enrolled in this pilot study. Two patients were excluded from the study due to incorrect documentation and intubation performed by a junior anesthetist. We concluded our study with 97 patients in the final analysis. In this study, we found that 5 patients (5.2%) had a mean NL of 7.6 cm (SD ± 0.9), with IDS>5. This reflects moderate to major difficulty in intubation, and a statistically significant p value, with p=0.022, considering the correlations between the groups (Table 1).
| Age(yrs.) | Gender | BMI | TMD(cm) | MO(cm) | MMP | NC(cm) | Neck Length(cm) | IDS |
|---|---|---|---|---|---|---|---|---|
| 46 | F | 36.79 | 6 | 4 | 3 | 35 | 7 | 6 |
| 46 | M | 35.08 | 6.5 | 5 | 3 | 41 | 7 | 7 |
| 45 | F | 32.52 | 7 | 5 | 3 | 37 | 8 | 6 |
| 64 | F | 34.13 | 6 | 3 | 3 | 39 | 7 | 6 |
| 50 | M | 35.6 | 6 | 6 | 3 | 46 | 9 | 7 |
BMI: Body Mass Index; TMD: Thyromental Distance; MO: Mouth opening; MMP: Mallampati; NC: Neck Circumference; IDS: Intubation Difficulty Score
Table 1: Airway assessment and other demographic criteria of the five patients who scored more than 5 in the IDS.
55 patients fell in the group, IDS=1-5 (slight difficulty) with a mean NL of 8.1 cm (SD ± 1.24). The remaining 37 patients who scored IDS=0 had a mean NL of 8.77 cm (SD ± 1.24). Patients’ NL was divided into three groups: ≤ 7 cm, 7-10 cm, and>10 cm. Considering IDS groups related to NL, we found the five patients with IDS>5 fell into the first two groups.
All of them exhibited MMP score of 3 and BMI<40. There was a significant negative correlation observed between NL and IDS score: correlation coefficient (r=-0.339, p=0.001). Other airwayc variables were weakly correlated with IDS score, except for TMD and age, with p value of 0.015 and 0.035, respectively (Tables 2 and 3).
| Variable | IDS=0 Mean ± SD | IDS 1 to 5 Mean ± SD | IDS>5 Mean ± SD | p-value |
|---|---|---|---|---|
| Age(yrs.) | 38.9(11.3) | 43.3(10.3) | 50.2(7.95) | 0.035 |
| Weight(kg) | 106.4(22.8) | 107.3(20.7) | 91.1(8.2) | 0.264 |
| Height(m) | 1.65(0.09) | 1.64(0.09) | 1.62(0.08) | 0.678 |
| BMI | 38.8(8.2) | 39.4(6.4) | 34.8(1.6) | 0.383 |
| TMD(cm) | 7.8(1.0) | 7.4(1.2) | 6.3(0.4) | 0.015 |
| MO(cm) | 5.2(1.1) | 4.9(0.9) | 4.6(1.1) | 0.205 |
| MMP | 2.3(0.7) | 2.5(0.8) | 3.0(0.0) | 0.102 |
| NC(cm) | 40.9(4.4) | 42.4(5.2) | 39.6(4.2) | 0.243 |
| Neck Length(cm) | 8.8(1.3) | 8.1(1.2) | 7.6(0.9) | 0.022 |
IDS: Intubation Difficulty Score; BMI: Body Mass Index; TMD: Thyromental Distance; MO: Mouth opening; MMP: Mallampati; NC: Neck Circumference.
Table 2: Comparison of anthropometric and various other parameters across different IDS score values.
| Variables | IDS-Group | p-value | |||
|---|---|---|---|---|---|
| N=0(%) | N=1-5(%) | N>5(%) | |||
| Neck length groups (cm) | <=7 | 3 (8.1%) | 15 (27.3) | 3 (60) | 0.02 |
| >7 to 10 | 29(78.4) | 38(69.1) | 2(40) | ||
| >10 | 5(13.5) | 2(3.6) | 0(0) | ||
| Dentition | F | 36(97.3) | 54(98.2) | 5(100) | 0.96 |
| E | 1(2.7) | 1(1.8) | 0(0) | ||
| Prognathism | U | 31(83.8) | 47(85.5) | 4(80) | 0.937 |
| O | 16(16.2) | 8(14.5) | 1(20) | ||
N: Number of Patients, F: Full Dentition; E: Edentulous; U: Underbite; O: Overbite
Table 3: Association categorized IDS score and neck length and other variables. The percentage is within the IDS groups.
Apparently, short TMD has a strong relation to short neck (Tables 1 and 2). On the Other Hand, no significant correlation was observed between BMI and neck length (r=0.010; p=0.924) and IDS score (r=-0.040; p=0.701) (Table 4). In considering patients’ height and NL, we found a non significant correlation between the two (r=0.171; p=0.094) (Table 2).
| IDS | BMI ≤ 40 n (%) | BMI>40 n (%) | p-value |
|---|---|---|---|
| IDS=0 | 25(40.3) | 12(34.3) | 0.148 |
| IDS 1 to 5 | 32(51.6) | 23(65.7) | |
| IDS>5 | 5(8.1) | 0(0) |
BMI: Body Mass Index; IDS: Intubation Difficulty Score.
Table 4: Association between BMI and IDS score.
Apart from congenital anomalies such as Klippel-Fleil, Noonan and Down syndromes and many others which have short neck, in case of obesity, there is a predilection for deposition of fatty tissue around the neck which causes an increase in neck circumference and the neck length appears shorter. The “ apparent ” reduction in neck length limits neck movement during laryngoscopy, as the operator cannot extend the neck, hence it can make visualization of the cords difficult during direct laryngoscopy, which is why obese people are deemed to be of the difficult airway category. In addition, deposition of fat at the back of the neck “Hump neck” would magnify the difficulty by further reducing mobility. As a result, different approaches, such as optimizing patient ’ s position “ ramping ” or video laryngoscopy are utilized as an adjunct.
Consequently, it is recommended practicing extra caution in managing the airway of obese patients with all three findings, namely thick neck, hump neck and short neck, by preparing the patient and equipment adequately and contemplate using the video laryngoscope, when available, as the primary intubation technique to achieve success in the first attempt.
Short Neck has not been clearly defined or systematically measured leading to a rather subjective assessment. Although it is commonly mentioned in airway textbooks, guidelines, and articles as a predictor of difficult airway, there has been no clear explanation on why a short neck makes intubation difficult and how they assess it. In their risk analysis of difficult intubation in obstetric anesthesia Rocke et al. reported that they assess short neck as one of the potential factors for difficult airway (RR 5.01) with a reference that they assessed it subjectively, though they were probably the first who linked obesity and short neck [8].
Despite the fact that the same pattern of subjectivity in predicting difficult intubation was seen in Noppens et al. report when they tried to compare C-MAC® video laryngoscope or the Macintosh laryngoscopein ICU patients, short big neck was a major factor in difficult intubation>20% of cases [18] while Prakash et al. mentioned range of neck movement and short neck separately as predictors of difficult airway without correlating them as a possible cause and effect and again without objective measurement of “short neck” [19].
Mosier et al. found that when comparing video laryngoscopy vs. direct laryngoscopy in difficult airway in the emergency department; short neck seemed to be a significant factor in predicting difficult intubation with unadjusted OR 2.2, however there was no mention of the method of how they assessed short neck [20].
In Sakles et al. study of management of patients with predicted difficult airways in the emergency department, the term “short neck” appeared as important predictor of approximately 43% of the patients under the categories of challenging to difficult intubation with a clear subjective scheme of assessment [21].
Joshi et al. in their study of difficult airway characteristics in the intensive care patients, considering all anatomical and other airway assessment were done subjectively, however the study showed that short neck and obesity scored the highest in the difficulty on intubation with a percentage and p value of 22%, 0.003 and 29%, 0.004 respectively [22]. All of the authors in the above studies and many others [23-25] have had used different approaches to airway assessment or even descriptive (subjective) method, and the reader can find that obesity and short neck are common denominators in predicting difficult intubation (just similar to Obstructive Sleep Apnea). Hence, the association of obesity with neck mobility, range of movement, thyromental, sternomental, and thyrohyoid distances, probably if short neck was excluded other variables would have been eliminated as risk factors. An association which led us to the study of short neck in obese patients only.
We measured neck length as explained above, as this is the part of the neck that is involved in neck movements especially flexion and extension. To improve visualization of the cords during laryngoscopy-the oral, pharyngeal, and laryngeal axes need to be aligned by assuming the sniffing position. Neck movement is essential for this. As the neck length reduces, the neck movement becomes increasingly restricted. Consequently, a SN makes cord visualization difficult. Many published articles that we reviewed focused on limited neck movement but did not refer to Short Neck as a possible cause [26-30].
The patients included in our study were divided into three groups depending on their NL: Group I - ≤ 7 cm, Group II-7-10 cm, and Group III>10 cm. Subsequently, we used the IDS to assess and communicate the degree of airway difficulty. An IDS of 0-easy intubation, IDS of 1-5-moderately difficult intubation and IDS of>5-very difficult to impossible intubation. In our study 5 patients scored>5 on the IDS. All these patients fell either into group I or Group II with a mean NL of 7.6 cm. Therefore, the authors propose that physicians consider obese patients with NL ≤ 8 cm to have potential difficult airways and prepare accordingly.
Our study failed to show any significant correlation between SN and difficult airway with increasing BMI, and that is most probably due to the small number of patients. Nevertheless, the theorem of association of BMI and difficult airway had been challenged by many authors [31-33].
As with any predictor of difficult airway a single component lacks sensitivity and specificity. This can be improved only by considering multiple factors together for that given clinical situation. Neck length adds to that armamentarium of predictors that we have, to foresee a difficult airway more accurately and possibly more effectively. This allows for better preparation consequently leading to lesser airway related morbidity and mortality.
Finally, using fingers’ width might be an easy and fast way of measuring SN, like measurements such as thyromental distance and mouth opening. Even though fingers’ breadth is not an accurate method, it can be used subjectively in a quick assessment, especially in emergency situations.
The limitations of our study are that it is a pilot study; used a small number of patients, only obese patients were considered and other anatomical variables such as cervical mobility were not used. In addition, this study was conducted in an academic single center; Hamad General Hospital where most complex surgical procedures were performed and have a high quality control by leading experienced anesthesiologists. Nonetheless, we suppose we have established a new and quantitative value for the term Short Neck.
The term Short Neck (SN) has long been used by anesthesiologists and acute care physicians in order to subjectively define a patient with possible difficult airway, particularly for tracheal intubation. However, it had not been clearly defined or quantified. Through this pilot study, we think we have established a provisional quantitative value for SN of ≤ 8 cm between the tip of the mastoid process and the point of inflection between the shoulder and the neck “apparent neck” should be regarded as a potential for difficult airway.
Addition of another variable in airway assessment will help physicians in acute care areas (Anesthesiologists, ICU and Emergency Physicians) to determine difficulty or the risk associated with tracheal intubation which entails early preparation in terms of requesting help of another person and/or other devices for possible management of difficult intubation.
To further our understanding on this topic, we hope that future studies will recruit a larger number of patients in conjunction with a comparative study that includes lean patients. Building on our pilot study, these developments will introduce new perspectives and further clarity to the subject of SN.
Assistance with the study: We would like to thank Dr. Prem Chandra, Ph D, for his assistance and statistical analysis, and would like to thank Ms. Nadia Ibrahim MA and Ms. Luma Hameed BA, for their editorial assistance. Special thanks to Dr. Francisco Lobo MD, for his assistance in reviewing and commenting on the manuscript.
Financial support and sponsorship: This work was financially supported by Hamad Medical Corporation. The Biostatician of the Academic Health Center has helped in the analysis only.
The study was approved by the Medical Research Centre (MRC) and the IRB of Hamad Medical Corporation, reference number 16323/16 dated 19 November 2017. All patients recruited had consented in writing to the study.
YEA, CBR, TMY, NK, SK, and AMRT have helped in obtaining informed consent, assessing inclusion and exclusion criteria, airway assessment and measurements and in providing feedback to the Principal investigator, JHF. SKM has helped in tables in addition to the above mentioned duties. ALA has helped in preparing the preoperative airway assessment sheet (Excel sheet) and in writing the manuscript including formatting it. JHF, principal investigator, led the overall supervision of the study, ensuring strict compliance, collecting, and recruiting patients, writing the manuscript, answering queries raised by co-authors and steering pre-study and follow-up meetings with all coauthors. All authors read and approved the final manuscript.
The authors declare that they have no competing interests.
None.
Citation: Faraj JH, Ahmed YE, Raval CB, Yousif TM, Kumar N, Kamat S, et al. (2020) Short Neck, a New Criterion for Airway Assessment: A Pilot, Cross Sectional Single Blind Study. J Anesth Clin Res. 11: 956. DOI: 10.35248/2155-6148.20.11.954
Received: 03-Jun-2020 Accepted: 23-Jun-2020 Published: 30-Jun-2020 , DOI: 10.35248/2155-6148.20.11.954
Copyright: © 2020 Faraj JH, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited