Journal of Psychology & Psychotherapy
Open Access
ISSN: 2161-0487
ISSN: 2161-0487
Research Article - (2024)Volume 14, Issue 6
Background: Postpartum Depression (PPD) is a global phenomenon that impacts nursing mothers and their children. However, there is limited research on PPD among nursing mothers in Akinyele Local Government Area of Oyo state, Nigeria. Therefore, this study sought to, determine the prevalence of PPD, examine knowledge of PPD, determine the influence of social factors on PPD among nursing mothers in Akinyele Local Government Area of Oyo state, Nigeria.
Materials and Methods: The descriptive cross-sectional and multiple linear regression research design were used in this study. The sample size for the study was 402 and data were collected using a self-developed structured and standardized questionnaire. Statistical Package for the Social Sciences (SPSS) version 23.0 was used to analyze the data using mean, standard deviation to determine the level of knowledge of the condition among the nursing mothers and prevalence while inferential statistics of multiple linear regression was used to examine the influence of social factors on PPD.
Results: There was a low level of knowledge of PPD among the nursing mothers. The prevalence of PPD is 72.1% among the population the study was carried out. Also, the social support (β=0.403, p<0.05) and cultural practices (β=0.224, p<0.05) independently influenced PPD among the nursing mothers in Oyo state, Nigeria.
Conclusion: The study found a significant poor knowledge of PPD, also, the prevalence of PPD was found to be high among nursing mothers in Akinyele Local Government Area of Oyo state. Inadequate social support and cultural practices were major contributing social factors that enhanced PPD among the nursing mothers. We recommend enhancing social support systems and cultural practices that promote wellness of nursing mothers and reduce PPD.
Social support; Cultural practices; Knowledge; PPD
The time following childbirth, known as the postnatal phase, is marked by a range of emotions, including happiness, worry, depression, anxiety, and occasionally a combination of these. PPD is a medical ailment characterized with complex physical, psychological and behavioral problems that usually affects 10 to 15% of new mothers [1]. The severity of postpartum mental health issues can range from mild PPD to more severe conditions such as postpartum psychosis. Postpartum psychosis is an acute illness with a multifactorial origin and is considered a psychiatric emergency that requires immediate treatment. The lifetime risk of PPD is estimated to be between 10% and 25%. However, the risk is particularly elevated in the early postpartum period, with rates around 5.6% and 5.7% at 2 months after childbirth [2].
The distinct strongest risk factor for PPD is a history of major depression during a previous postpartum period or pregnancy. Other significant risk factors include low social support, experiencing significant life events, low socioeconomic status, obstetric complications, and untreated maternal health conditions. These risk factors for PPD can disrupt the mother infant bond and have negative consequences for the child's development and wellbeing [3,4].
The effect of Personality Disorders (PD) has detrimental consequences on children, such as a higher chance of delayed mental and motor development, cognitive impairment in infants, poor self-regulation, low self-esteem, and behavioral issues among others [5]. The syndrome has a major impact on the family health, resulting in problems like poor parenting, mood disorders, sleep disorders, interpersonal difficulties, and nursing challenges.
There are different forms of PPD which include postpartum anxiety, postpartum obsessive-possessive disorder, postpartum panic disorder, postpartum post-traumatic stress disorder, postpartum psychosis [6]. PPD by impact level has been classified into two types which are maternal and paternal PPD. Although both Diagnostic and Statistical Manual of Mental Disorders (2013) 5th edition (DSM-5) and International Classification of Disorders (2019) 11th edition (ICD-11) have specifiers for peripartum onset of major depressive order Mild to Moderate Depression (MMD), they do not have a specific classification for PPD disorder as a separate entity.
PPD is three times more common in underdeveloped nations than in industrialized ones, with several risk factors contributing to this difference [7]. In Africa, the estimated prevalence of PPD is 18.4%. However, this rate varies significantly by country. For instance, Uganda has reported a notably high prevalence rate of 43.0%, while Cameroon has a prevalence of 23.4% [8]. Conversely, countries like Ethiopia and Ghana have lower rates, with prevalence reported at 13.1% and 3.8%, respectively. Morocco also has a relatively lower prevalence rate at 11.6%. In Zambia and other Southern African nations, the prevalence of PPD is also on the higher end of the spectrum. Studies indicate that the prevalence of PPD in Zambia is approximately 20.7% [8]. Similarly, neighboring countries such as Zimbabwe and Malawi report higher prevalence rates, with Zimbabwe at 23.0% and Malawi at 19.5% [9,10]. These elevated rates underscore the importance of addressing risk factors and providing appropriate support for new mothers to promote maternal mental health and positive outcomes for both mother and child.
The prevalence of PPD was found to be low in two studies conducted in South-Eastern Nigeria (10.7%, 30.0%, and 44.5%), while it was reported to be 21.8% in Northern Nigeria [11]. Due to several variables, such as screening techniques, study designs, geographic region, socioeconomic position, and cut-off scores, the prevalence of PPD varies both internationally and within Nigeria and there is limited research that focus on PPD among nursing mothers in the region in Nigeria [12].
Theoretical framework for the study
The Postpartum Depression Theory (PDT) was used to underpin this study. According to psychology writing, PDT was based on PPD research and was applied to professionally help women get through this challenging life span with the goal of changing the perception of PPD and to improve patient care [13]. The model views PPD as a biological problem consisting of four stages. The four stages of PPD, according to the theory, include encountering terror, dying of self, struggling to survive, and regaining control [14]. Experiencing terror can be expressed in “horrifying anxiety attacks, obsessive thinking, and enveloping fogginess,” and dying of self can feel like “alarming un-realness, isolation of self, and contemplation of self-destruction [15]. Understanding the structure of the phenomenon of PPD is the most important component and goal of the theory, as it allows one to change the attitude towards bad mood and well-being after childbirth, which millions of women faces [16].
The main benefit of the theory is that women can change attitudes towards their condition and get rid of feelings of guilt for it [17]. At the same time, appreciation to health professionals in understanding of this condition, women can receive adequate assistance [18,19]. Understanding the biological causes of PPD can also improve the social relationships of a woman and her environment by raising her expectations for social support. The cultural significance is attributed to an increased culture of interaction between health professionals and patients and a decrease in secondary irritation [20]. The universality of the theory is expressed in the fact that it applies to women of any socioeconomic status and age. The theory is of unique importance for all health faculties, education, and researchers as it allows patients to change their attitudes towards symptoms associated with PPD. Additionally, the knowledge of the existence of PPD allows for timely treatment and interventions [21,22].
Study design
A cross-sectional study was conducted to investigate PPD among nursing mothers in Akinyele Local Government Area, Oyo state, Nigeria.
Study settings
The study took place in Akinyele Local Government Area, focusing on government owned health facilities within the region.
Study population
The target population included nursing mothers attending postnatal clinics in the selected health facilities.
Sampling methods and sample size
A total sample size of 402 was established, reflecting 50% of the estimated population derived from local government records. The sampling methodology utilized a multistage approach, beginning with purposive sampling to identify 37 government operated health facilities from the available options. Subsequently, a random selection process was employed to choose 15 facilities from the initial 37, prioritizing those with high postnatal attendance rates. Simple random sampling without replacement and convenient sampling techniques were then applied to select participants from these facilities based on accessibility and a willingness to engage in the study.
Data collection
Data was collected using a self-developed and validated questionnaire. The questionnaire was translated from English to Yoruba, the predominant language in the rural setting, and then back to English to ensure reliability and consistency. Prevalence of Postpartum Depression Scale was self-developed (PPPDS) (r=0.65), Knowledge of Postpartum Depression Scale (KPPDS) (r=0.71), Edinburgh Postnatal Depression Scale (EPDS) was used for PPD and social factors scales comprising social support and cultural practices were used with r=0.74 and 0.80 respectively. The dependent variable in the study was PPD while the independent variables were social support and cultural practices.
Data analysis
The data collected were analyzed using SPSS version 23. Statistical methods included frequency counts, simple percentages, standard deviations, and multiple linear regression analysis.
Sociodemographic information of the respondents
Table 1, illustrates that more than half of the respondents, specifically 59.3%, fell within the age range of 30 to 39 years. Additionally, 54.5% indicated that they had one child, while 79.9% identified as married. Furthermore, 58.8% of the participants reported their affiliation with the Islamic faith.
| Age | Frequency | Percentage |
|---|---|---|
| Less than 30 years | 115 | 28.9 |
| 30-39 | 236 | 59.3 |
| 40-49 | 36 | 9 |
| 50-59 | 12 | 3 |
| Total | 398 | 100.0 |
| No. of childbirth | ||
| One | 217 | 54.5 |
| Less than 3 | 126 | 31.6 |
| More than 3 | 55 | 13.8 |
| Total | 398 | 100.0 |
| Religion | ||
| Christianity | 146 | 36.7 |
| Islam | 234 | 58.8 |
| Traditional | 12 | 3 |
| Others | 6 | 1.5 |
| Total | 398 | 100.0 |
| Marital status | ||
| Married | 318 | 79.9 |
| Single mother | 59 | 14.8 |
| Divorce | 17 | 4.3 |
| Widow | 4 | 1 |
| Total | 398 | 100.0 |
| Educational qualification | ||
| No formal educational | 194 | 48.7 |
| Formal education | 204 | 51.3 |
| Total | 398 | 100.0 |
Table 1: Sociodemographic information of the respondents.
Prevalence of PPD among nursing mothers: The results presented in Figure 1, of this study indicate that 287 respondents, accounting for 72.1%, experienced PPD, whereas 111 respondents, or 27.9%, did not exhibit symptoms of PPD.
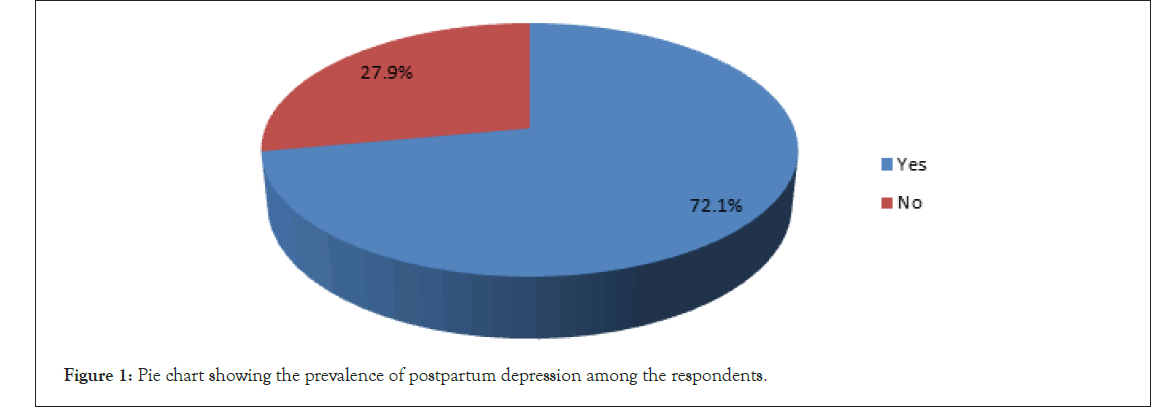
Figure 1: Pie chart showing the prevalence of postpartum depression among the respondents.
The level of knowledge of PPD among nursing mothers: Table 2, reveals insights into PPD among nursing mothers in the study. While 86.2% recognized it as a health concern, only 16.8% knew it was treatable, and 20.9% understood that symptoms could last from 4 weeks to 1 year. Alarmingly, 18.4% mistakenly thought it was contagious. Only 49% of mothers were generally aware of PPD. Majority of the respondents (83.2%) disagree PPD can be treated. Also, half of the respondents (51.0%) agree that mood swings and sleeplessness are symptoms of PPD (Table 3).
| S No. | Level of knowledge of postpartum depression | Yes | No |  |
Standard Deviation (SD) |
|---|---|---|---|---|---|
| 1 | PPD is a health-based issue | 184 (46.2%) | 214 (53.8%) | 1.13 | 0.317 |
| 2 | I have heard about PPD before | 111 (27.9%) | 287 (72.11%) | 1.57 | 0.293 |
| 3 | I know PPD can be contracted | 82 (20.6%) | 316 (79.4%) | 1.19 | 0.154 |
| 4 | I am aware of PPD | 195 (49%) | 203 (51%) | 1.15 | 0.285 |
| 5 | I know PPD can be treated | 67 (16.8%) | 331 (83.2%) | 1.12 | 0.167 |
| 6 | PPD could lead to suicide and infanticide | 103 (25.9%) | 295 (74.1%) | 1.63 | 0.312 |
| 7 | Have been diagnosed of PPD before | 26 (6.5%) | 372 (93.5%) | 0.74 | 0.095 |
| 8 | PPD symptoms last between 4 weeks to 1 year | 83 (20.9%) | 315 (79.1%) | 1.34 | 0.187 |
| 9 | Mood swings and sleeplessness are symptoms of PPD | 203 (51%) | 195 (49%) | 2.12 | 0.650 |
| 10 | PPD is infectious | 153 (38.4%) | 245 (61.6%) | 1.47 | 0.204 |
Table 2: Level of knowledge of PPD among nursing mothers.
| Range | Level | Frequency | Percentage |
|---|---|---|---|
| 0-1.32 | Low | 287 | 72.1 |
| 1.33-2.66 | Moderate | 111 | 27.9 |
| 2.67-4 | High | - | - |
Table 3: Test of norms indicating the level of knowledge regarding PPD among nursing mothers in Akinyele Local Government Area, Oyo state, Nigeria.
Regression analysis of the correlation between social factors and PPD in nursing mothers: Table 4, illustrates the findings of a regression analysis that investigates the correlation between social factors and PPD in nursing mothers residing in the Akinyele Local Government area of Oyo state. The results indicate that both social support and cultural practices serve as significant predictors of PPD. Notably, social support is identified as the most influential predictor, exhibiting a standardized coefficient (Beta (β)) of 0.403 and a t-value of 8.640 (p<0.002). Additionally, cultural practices are also found to significantly predict PPD, with a standardized coefficient (β) of 0.224 and a t-value of 3.645 (p<0.004). The unstandardized coefficients (β) for social support and cultural practices are 0.908 and 0.462, respectively, accompanied by standard errors of 0.105 and 0.127. The regression equation's constant term has an unstandardized coefficient of 23.157 (standard error=2.839) and is statistically significant (p<0.001, t-value=8.155).
| Correlation coefficient (R) | Coefficient of determination (R2) | Adjusted coefficient of determination (R2) | Function (F) | Numerator degrees of freedom (df1) | Denominator degrees of freedom (df2) | Probability value (p-value) | |||
|---|---|---|---|---|---|---|---|---|---|
| PPD | 0.335 | 0.122 | 0.106 | 16.754 | 2 | 377 | 0.001 | ||
| Predictor | Unstandardized coefficients (B) | Standard Error (SE) | Test statistic (T) | Probability value (p-value) | Beta (β) | Lower | Upper | Variance Inflation Factor (VIF) | Tolerance |
| Intercept | 23.157 | 2.839 | 8.155 | 0.001 | - | 0.46 | 1.95 | 3.32 | 0.135 |
| Social support | 0.908 | 0.105 | 8.640 | 0.001 | 0.403 | 0.74 | 2.48 | 4.75 | 0.202 |
| Cultural practice | 0.462 | 0.127 | 3.645 | 0.004 | 0.224 | 0.21 | 1.47 | 1.05 | 0.485 |
Table 4: Regression analysis of correlation between social factors and PPD in nursing mothers in Akinyele Local Government, Oyo state.
The study examined specifically the prevalence of PPD among nursing mothers, knowledge of PPD among nursing mothers and influence of social factors on PPD; the association between cultural practices and PPD as well as association between spousal support and PPD [23]. The study found a high prevalence of PPD at 72.1%, which is notably higher than prevalence rates reported in other regions of Nigeria. For instance, studies from Northern and Eastern Nigeria reported lower rates, with Southeastern Nigeria showing a prevalence of 30.6% at an EPDS cutoff score of 10 Osterman et al. [24]. The higher prevalence observed in this study may be attributed to regional differences, variations in risk factors, and differences in study designs and methodologies. The rural setting of Akinyele, characterized by limited healthcare access and traditional practices, could have contributed to these elevated rates.
The results indicated that the majority, specifically 287 nursing mothers (72.11%), reported that they had not previously heard of PPD, and 331 mothers (83.2%) were unaware that it is treatable. Additionally, only 26 mothers (6.5%) had received a prior diagnosis of PPD. The overall average weighted mean for the knowledge level regarding PPD was calculated to be 2.12. These findings suggest that the awareness of PPD among nursing mothers in the Akinyele Local Government area is notably low, with 72.1% (n=287) exhibiting a low level of knowledge and 27.9% (n=111) demonstrating a moderate level of understanding regarding the condition suggesting that targeted interventions are necessary to enhance maternal mental health and wellbeing in this community.
The finding also revealed that 72.1% of nursing mothers were unaware of PPD. This finding aligns with Gureje et al. [25,26], who reported widespread ignorance and misconceptions about mental health in Nigeria. Also in agreement, a study by Hannah et al., found 42% of the respondents did not understand depression among mothers, suggesting that while awareness is low, the impact of PPD is substantial across different regions [27]. The rural context of Akinyele likely exacerbates the lack of awareness and knowledge of PPD, as access to mental health education and resources is often limited.
Regression analysis in our study indicated that social support (β=0.403, p<0.05) had a stronger impact on PPD compared to cultural practices (β=0.224, p<0.05). The results indicate that social support and cultural practices are important factors in predicting PPD among the nursing mothers in this study, with social support exerting a more pronounced effect. The F-ratio calculated at 16.754 is statistically significant (p<0.0001), highlighting the importance of the joint effects of cultural practices and social support on PPD. Nevertheless, the relatively modest R2 value suggests that additional variables not incorporated in this analysis may account for a considerable amount of the variance in PPD. Consequently, these results support the rejection of the null hypothesis, affirming that social factors, namely cultural practices and social support, are significant predictors of PPD among the nursing mothers in this research.
This finding is consistent with Kumar et al., who emphasized the importance of spousal support in preventing PPD [28]. Additionally, Okasha et al., found that feeling unloved by a partner and experiencing marital problems were associated with higher PPD rates [29]. The significant role of social support corroborates findings from studies in Turkey, which also highlighted the importance of social networks in mitigating PPD, cultural practices and cultural factors, such as gender preference, have been identified as predictors of PPD in other studies [6]. For example, research from Kenya and Turkey has shown that cultural norms, including gender preference for male children, contribute to PPD [30-32]. This article findings regarding cultural practices align with these results, suggesting that cultural expectations and practices significantly influence postpartum mental health. Our study's results are also supported by Adeyemo that who found the domestic violence increases the risk of PPD, highlighting the detrimental impact of partner violence on mental health [2,33]. Similarly, Logsdon et al., and Lee et al., found a strong correlation between social support and PPD, emphasizing that lack of support, especially from partners, can worsen PPD symptoms [32,34].
This research indicates a significant occurrence of PPD among nursing mothers in the Akinyele Local Government Area of Oyo state, Nigeria, primarily due to a lack of awareness and understanding of the condition. The study emphasizes that inadequate social support and specific cultural practices play a substantial role in the prevalence of PPD within this demographic. The results highlight the urgent necessity for enhanced social support frameworks and improved mental health education, especially in rural Nigerian settings, to combat the elevated rates of PPD. The observed differences in prevalence and the impact of social determinants across various studies stress the importance of considering regional and cultural factors when formulating strategies to tackle postpartum mental health challenges.
This study focuses on social factors as predictors of PPD in Akinyele Area of Oyo state, Nigeria. PPD may also be enhanced by other factors such as marital factors and socioeconomic factors. Depression may also affect both the young and the old irrespective of socioeconomic status. It is acknowledged that this study was carried out in one local government area out twelve as it does not represent all women in Oyo state. The study will contribute to depression study, and it can also be replicated in other local government areas and across other large settings.
To effectively address PPD, a comprehensive approach is essential. This should involve bolstering social support systems by engaging family members, healthcare professionals, and community leaders. Moreover, there is a pressing need for extensive awareness initiatives and educational programs aimed at mothers throughout the prenatal, perinatal, and postnatal periods. These efforts should focus on enhancing knowledge about PPD, its symptoms, and the resources available for support. Additionally, healthcare policies and interventions must be customized to address the specific cultural and social elements identified as contributing factors to PPD in this area. By adopting culturally sensitive and community-oriented strategies, it may be feasible to significantly lower the incidence of PPD and foster improved maternal health outcomes. Future investigations should concentrate on creating and assessing targeted interventions that respond to the distinct challenges encountered by nursing mothers in this cultural milieu, with the objective of developing more effective and contextually appropriate methods for the prevention and management of PPD.
Ethical approval was granted by the Oyo state Ministry of Health Research Ethics Committee with (Reference No: AD 13/479/235). Written informed consent was obtained from all respondents, ensuring voluntary participation with no penalties for noninvolvement or withdrawal. Confidentiality of the information collected was strictly maintained, and questionnaire forms were collected on the spot by four trained research assistants to ensure high retrieval rates.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Johnson BO, Twizelimana D, Nkhata LA (2024). Social Factors as Predictors of PPD among Nursing Mothers in Akinyele Local Government Area of Oyo State, Nigeria. J Psychol Psychother. 14:495.
Received: 30-Sep-2024, Manuscript No. JPPT-24-34399; Editor assigned: 02-Oct-2024, Pre QC No. JPPT-24-34399 (PQ); Reviewed: 16-Oct-2024, QC No. JPPT-24-34399; Revised: 23-Oct-2024, Manuscript No. JPPT-24-34399 (R); Published: 30-Oct-2024 , DOI: 10.35841/2161-0487.24.14.495
Copyright: © 2024 Johnson BO, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.